Medicaid eligibility and enrollment in Mississippi

Mississippi has not yet expanded Medicaid, but several Medicaid expansion bills have been introduced by lawmakers in early 2024

Who is eligible for Medicaid in Mississippi?
As published by CMS, these are the income limits for key coverage groups under Mississippi’s Medicaid program (note that these numbers include a built-in 5% income disregard that’s used for income-based Medicaid eligibility determinations):
- Adults with dependent children are eligible if their household income doesn’t exceed 24% of poverty level. This is about $488 per month for a family of three,1 one of the lowest thresholds in the country.
- Infants under one are eligible for Medicaid if their household income is up to 199% of poverty.
- Children 1 – 5 are eligible if their household income is up to 148% of poverty.
- Children 6 – 18 are eligible if their household income is up to 138% of poverty.
- Children with household incomes above the Medicaid thresholds are eligible for CHIP if their household incomes are up to 214% of poverty
- Pregnant women are eligible for Medicaid if their household income does not exceed 199% of poverty. (Postpartum coverage for the mother continues for 12 months after the birth;2 Mississippi enacted legislation in 2023 to extend it from the 60-day limit that was previously used.)
Mississippi has not implemented Medicaid expansion under the ACA, so non-disabled adults without dependent children are not eligible for Medicaid regardless of how low their income is. Several Medicaid expansion bills have been introduced in Mississippi’s legislature in 2024 to expand Medicaid under the ACA.3
A separate bill (HB1146), introduced in February 2023, calls for the state to obtain federal permission to expand Medicaid eligibility up to 100% of the poverty level, and also implement a program that would provide financial assistance with employer-sponsored health insurance or individual/family health insurance if the household’s income is above the poverty level but not more than 200% of the poverty level. Depending on income, these programs would cover some or all of the premium and/or out-of-pocket costs that enrollees would otherwise have.4
In previous years, Medicaid expansion bills have failed to advance out of committee, but Mississippi House Speaker Jason White clarified in the fall of 2023 that Medicaid expansion would be addressed by the legislature in 2024.5
Apply for Medicaid in Mississippi
You can enroll through HealthCare.gov or you can fill out a PDF of the Mississippi Medicaid Application Form. You can also enroll by phone at 800-318-2596.
Eligibility: Parents with dependent children are eligible with household incomes up to 22% of FPL. Children are eligible for Medicaid or CHIP with household incomes up to 209% of FPL, and pregnant women are eligible with household incomes up to 194% of FPL.
Has Mississippi expanded Medicaid eligibility?
Mississippi Medicaid has not been expanded as allowed under the Affordable Care Act (ACA), despite the state medical association’s support of expansion going back to August 2016.
Mississippi is one of just 10 states that have not yet expanded Medicaid as of early 2024. Several new pieces of legislation to expand Medicaid were introduced in Mississippi in early 2024.6
An additional bill (HB1146) was introduced in February 2024, and takes a different approach than regular Medicaid expansion as called for in the ACA. This bill would direct the state to seek federal approval to expand Medicaid up to 100% of the poverty level (instead of 138%), and to also create a program under which the state would provide financial assistance for people enrolling in employer-sponsored health insurance or individual/family health insurance, if their household income is above the poverty level but not more than 200% of the poverty level. The assistance would help to cover some or all of the premiums and out-of-pocket costs these enrollees would otherwise face, with more assistance available to those on the lower end of the income spectrum.4
Medicaid expansion bills had been introduced in 2023 and died in committee,7 but Mississippi House Speaker Jason White addressed the issue in the fall of 2023, saying that Medicaid expansion would be addressed by the legislature in 2024. White noted “I think we as Republicans have probably earned a little bit of the bad rap we get on health care in Mississippi. Part of that is that we haven’t had a full-blown airing or discussion of Medicaid expansion. We’ve just said, ‘No.’”5
Non-disabled adults without children are not eligible for Medicaid in Mississippi regardless of how low their income is, and parents with dependent children are only eligible with incomes that don’t exceed 24% of the poverty level. This is one of the lowest eligibility caps in the country — only Texas and Alabama have lower limits.8
If Mississippi did expand eligibility for Medicaid as called for in the ACA, an estimated 220,000 would be newly eligible for coverage. Unfortunately, in the poorest, sickest state in the U.S., the majority of lawmakers and two governors have opted to reject federal funds that would provide health insurance for the state’s poorest residents.
Because Marketplace subsidies are only available in Mississippi for people whose household incomes are at least 100% of poverty, an estimated 88,000 people in Mississippi are in the coverage gap and have no realistic access to health insurance9 (some analyses indicate that there are more like 130,000 people in the coverage gap in Mississippi). They aren’t eligible for Medicaid, and they also aren’t eligible for subsidies.
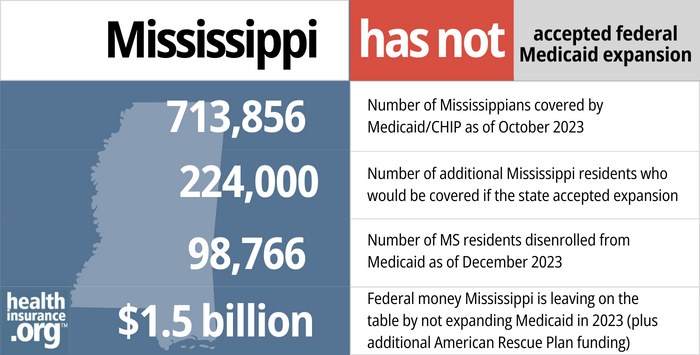
- 713,856 – Number of Mississippians covered by Medicaid/CHIP as of October 202310
- 224,000 – Number of additional Mississippi residents who would be covered if the state accepted expansion11
- 98,766 – Number of Mississippi residents disenrolled from Medicaid as of December 202312
- $1.5 billion – Federal money Mississippi left on the table by not expanding Medicaid in 2023 (plus additional American Rescue Plan funding)13
Explore our other comprehensive guides to coverage in Mississippi

Use this guide to help you find the right health plan in Mississippi. Many people find an ACA Marketplace (exchange) plan, also known as Obamacare, to be a cost-effective choice.
Learn about health insurance coverage options in Mississippi.


Need dental coverage? Learn about available options and find the right dental plan in Mississippi with our guide.


As of early 2023, there were 625,029 people with Medicare coverage in Mississippi.14 Our Mississippi Medicare guide explains what you need to know about the various parts of Medicare, as well as state regulations pertaining to Medigap plans.


In Mississippi, consumers can buy short-term health insurance plans with initial policy terms of up to 364 days with the option to renew for a total duration up to 36 months. As of 2023, there were at least eight insurers selling short-term health insurance plans in Mississippi.15
Learn about short-term insurance regulations in Mississippi.

Frequently asked questions about Mississippi Medicaid eligibility and enrollment
How do I enroll in Medicaid in Mississippi?
If you are under 65 and don’t have Medicare:
- You can enroll through HealthCare.gov, either online or by phone at 1-800-318-2596.
- You can fill out the PDF version of the Mississippi Medicaid Application Form and either click the application submit button, or save the completed PDF and email it to [email protected].
- You can also print out the PDF application, complete it by hand, and fax, mail, or deliver it in person. You can fax it to 601-576-4164. You can mail it to 550 High Street, Suite 1000, Jackson, MS 39201. Or you can take it to your nearest Mississippi Division of Medicaid regional office.
If you are 65 or older or have Medicare, use this website to apply for Medicaid.
How does Medicaid assist Medicare beneficiaries in Mississippi?
Many Medicare beneficiaries receive assistance through Medicaid with the cost of Medicare premiums, cost sharing, and services Medicare doesn’t cover — such as long-term care.
Our guide to financial assistance for Medicare beneficiaries in Mississippi explains these benefits, including Medicare Savings Programs, Extra Help, long-term care benefits, and income guidelines for assistance.
How is Mississippi handling Medicaid renewals after the pandemic?
Medicaid disenrollments were paused nationwide from March 202o through March 2023. Even if a person’s circumstances changed and they were no longer Medicaid-eligible, their coverage continued throughout the pandemic. Starting in early-mid 2023, states began checking the eligibility of everyone enrolled in Medicaid and disenrolling those who no longer met the eligibility criteria or who failed to respond to a renewal notice.
The first round of disenrollments in Mississippi came in June 2023, and states must redetermine all enrollees’ eligibility during a year-long “unwinding” period. By December 2023, 98,766 people had been disenrolled from Mississippi Medicaid.12 The pace of disenrollments had slowed considerably, with more than 29,000 people disenrolled in June 2023,16 but fewer than 1,200 disenrolled in December 2023.17
Mississippi continued to request eligibility verification from enrollees throughout the pandemic, as did many other states. But people who didn’t respond or who were no longer eligible could not be disenrolled unless they requested that. Instead, Mississippi moved these people from managed care plans to fee-for-service Medicaid during the pandemic. This saved the state some money, but potentially reduced some enrollees’ access to the supplemental services that the Medicaid managed care plans provide.
If a person is no longer eligible for Medicaid and also not eligible for Medicare or an employer’s health plan, they will need to obtain their own replacement coverage. In most cases, the exchange/Marketplace is the best way to do this, and Mississippi uses HealthCare.gov as its marketplace. By September 2023, CMS reported that 13,083 people who had been disenrolled from Mississippi Medicaid had enrolled in a Marketplace plan.18
HealthCare.gov is offering an extended enrollment opportunity, from March 31, 2023 through July 31, 2024, for anyone who loses Medicaid at any time during that window. This means people do have to enroll within 60 days of losing their Medicaid, as would normally be the case. However, the best course of action is still to enroll as soon as possible, to minimize gaps in coverage (Marketplace plans do not have retroactive effective dates, so a gap in coverage results if you wait to sign up for the new plan until after your Medicaid has ended).
Because Mississippi has not expanded Medicaid under the ACA, the state does still have a coverage gap for adults with income below the poverty level. So it’s important for low-income residents to be aware of how to avoid this coverage gap.
Legislation impacting Mississippi Medicaid
Why did Mississippi's ballot not have a Medicaid expansion initiative?
In 2021, Medicaid expansion advocates in Mississippi began gathering signatures to get Initiative 76 on the 2022 ballot. This measure would have let the state’s voters decide whether Medicaid should be expanded, and it’s worth noting that this approach has resulted in Medicaid expansion in several other states and voters have never failed to pass a Medicaid expansion measure in any state when it has been on the ballot. However, Initiative 76 was suspended in mid-2021, after it was determined that a state Supreme Court ruling in 2020 had invalidated the Mississippi ballot initiative process. So voters in Mississippi did not get a chance to weigh in on Medicaid expansion in the 2022 election.
Pending Mississippi Medicaid work requirement could end coverage for thousands, but is unlikely to be approved by the federal government
Even though Mississippi hasn’t expanded Medicaid and has some of the most stringent eligibility guidelines in the country, the state has sought federal approval to make it even harder for people to get Medicaid coverage in Mississippi.
In October 2017, Mississippi submitted a proposed 1115 waiver to CMS, detailing the work requirement that the state wants to implement. The waiver was still pending approval as of 2024, and the Biden administration has informed states that Medicaid work requirements are not compatible with the mission of Medicaid. The Trump administration had approved several states’ proposed Medicaid work requirements, but the Biden administration has revoked all of those approvals. Proposals like Mississippi’s, which were still pending when the Biden administration took office, have been left pending and are unlikely to be approved.
(Georgia implemented a work requirement in 2023, but only for the population that became newly eligible for the state’s partial Medicaid expansion at the same time. The work requirement in Georgia does not apply to anyone who was already eligible for coverage.)
Mississippi’s proposal would allow the state to require some Medicaid enrollees to work, volunteer, attend school, participate in substance abuse treatment, or otherwise fulfill the work requirement for at least 20 hours per week.
People would be exempt if they are disabled, physically or mentally unable to work, a primary caregiver for someone in need of care, elderly, under the age of 19, pregnant, Native American, or included in various other exempt populations. Since Mississippi has not expanded Medicaid under the ACA, the vast majority of the state’s Medicaid enrollees would already be exempt from the work requirement. The work requirement would really only apply to certain low-income parents and people receiving transitional medical assistance (a program that extends Medicaid coverage for up to 12 months for people who start earning too much money to continue to qualify for Medicaid).
Mississippi Medicaid covers about 728,000 people, but only about 56,000 of them are in the low-income parent Medicaid eligibility category. And of those, most would have exemptions. About 15,000 to 20,000 people would end up having to work as a result of the work requirement, and many are already working.
Ultimately, about 5,000 people would be expected to lose coverage in Mississippi each year if the work requirement were to be approved and implemented (as noted above, that is not likely to happen under the Biden administration). According to the Clarion-Ledger, 91% of the people who would lose access to Medicaid under the proposed work requirement in Mississippi are low-income mothers. And more than two-thirds are African American.
These low-income parents are in a catch-22 situation: If they earn more than 27% of the poverty level (that works out to about $518/month for a household of three), they’d no longer be eligible for Medicaid. And if they don’t work, they’ll also lose access to Medicaid as a result of the work requirement. So in order to have health insurance, they would either have to maintain a job that provides health insurance coverage, or earn at least 100% of the poverty level so that they could obtain premium subsidies in the exchange and purchase an affordable individual health plan. One hundred percent of the poverty level is about $1,919/month for a household of three, so it’s a big jump from the Medicaid eligibility cutoff to the start of eligibility for premium subsidies.
To address these concerns, the state proposed an additional 12 months of transitional Medicaid coverage for people who remain in compliance with the work requirement for the full 24 months. Georgetown University’s Joan Alker describes this as a “wholly inadequate solution.” It’s temporary, doesn’t provide any sort of solution after the 24 months of transitional Medicaid coverage ends, and hinges on the unrealistic expectation that low-income, working parents will not experience even one month of unemployment during their 24 months of transitional Medicaid.
CMS had initially opened a comment period in early 2018 for Mississippi’s waiver proposal. But after the state revised the proposal to add 12 months of transitional Medicaid coverage, the comment period was re-opened. During the re-opened comment period, 320 comments were submitted, and 319 of them were in opposition to the state’s proposed Medicaid work requirement. The revised proposal is still under review by CMS as of 2024, but is unlikely to ever be approved.
Mississippi Medicaid enrollment numbers
Total Mississippi Medicaid/CHIP enrollment was 728,144 as of September 2023,19 including 650,652 people with Medicaid and 77,492 children with health insurance coverage under CHIP.
Total enrollment was 18% higher as of the fall of 2023 than it had been in late 2013.20 The growth was largely due to the COVID pandemic, and enrollment began declining in mid-2023, after the pandemic-related continuous coverage rule ended (details above).
Missing out on billions in federal funding
As the ACA was written, it called for Medicaid expansion in every state for residents with incomes up to 133% of poverty (plus a 5% income disregard, bringing the effective eligibility threshold to 138% of the poverty level). But in 2012, the Supreme Court ruled that states could not be penalized for opting out of expansion, and Mississippi is one of a dwindling number of states that have not yet expanded Medicaid.
In states that expand Medicaid, the federal government paid the full cost of expansion through 2016. After that, states gradually began to pay a share of the expansion cost, but the federal government will always pay at least 90%. As a result, states that reject Medicaid expansion are leaving billions of dollars on the table.
From 2013 through 2022, Mississippi gave up $14.5 billion in federal funding that would otherwise have been available to the state to help provide medical care for low-income residents. And states that newly expand Medicaid after April 2021 are eligible for two years of additional federal Medicaid funding under the American Rescue Plan, but Mississippi has not yet taken advantage of that.
Since residents in states not expanding Medicaid still have to pay federal taxes, Mississippi residents have been subsidizing Medicaid expansion in other states. Over a decade, people in Mississippi are paying $1.7 billion in federal taxes that are used to pay for Medicaid expansion in other states.
Will Mississippi expand coverage?
Governor Tate Reeves, who assumed office in 2020, campaigned in opposition to Medicaid expansion. His viewpoint is consistent with former Governor Phil Bryant. Bryant claimed that the state wouldn’t be able to bear the cost if the federal government were ever unable to uphold its promise to pay at least 90% of the cost, and referred to accepting Medicaid expansion as a “fool’s errand.”
Mississippi’s share of traditional Medicaid costs climbed from fiscal year 2012 to fiscal year 2017. Lawmakers have highlighted this as a reason for not expanding coverage, but they’re missing the point (whether purposely or not) that Medicaid expansion is funded under different rules from traditional Medicaid. Under Medicaid expansion, the cost to cover newly eligible residents was fully funded by the federal government through the end of 2016. In 2020 and forward, states pay 10% of costs associated with the Medicaid expansion population.
And of particular importance, states that have expanded Medicaid have seen substantially smaller growth in state Medicaid spending than states that haven’t expanded Medicaid.
In June 2013, Republicans in both chambers of the Mississippi legislature voted against Medicaid expansion. They did vote to continue the state’s existing Medicaid program, which came within days of expiring and had to be dealt with in a special legislative session called by Bryant. The issue of Medicaid expansion might not have even made it to a vote except that Democrats threatened to withhold their votes for renewing the existing Medicaid program unless Republicans would agree to take the issue of Medicaid expansion to a vote. No Republicans voted for Medicaid expansion, although one, Senator Billy Hudson of Hattiesburg, said that he would eventually vote for Medicaid expansion, “but not today.”
The Mississippi State Medical Association put forth a resolution in August 2016 calling for “expanded coverage” but didn’t use the words “Medicaid expansion” in their draft, knowing that the issue was too politically charged.
Mississippi might eventually pursue Medicaid expansion, possibly relying on a modified expansion waiver proposal similar to those used in a handful of other conservative states. And legislation has once again been introduced in 2024 that calls for Medicaid expansion.19 But for now, in the nation’s poorest state, the poorest residents have no access to health coverage at all.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- Income Limits for Medicaid and CHIP Programs. Mississippi Division of Medicaid. Accessed January 2024. ⤶
- MS SPA 23-0015 Postpartum Coverage approved by CMS. Mississippi Division of Medicaid. Accessed January 2024. ⤶
- Mississippi House Bill 436; Mississippi House Bill 379; Mississippi House Bill 368; Mississippi House Bill 464; Mississippi House Bill 479; Mississippi Senate Bill 2045; Mississippi Senate Bill 2046. BillTrack50. Introduced January 2024 ⤶
- ”Mississippi House Bill 1146” BillTrack50. Introduced February 2024. ⤶ ⤶
- Are Republicans about to leave Gov. Tate Reeves behind on Medicaid expansion? Mississippi Today. September 2023. ⤶ ⤶
- Mississippi House Bill 436; Mississippi House Bill 379; Mississippi House Bill 368; Mississippi House Bill 464; Mississippi House Bill 479; Mississippi Senate Bill 2045; Mississippi Senate Bill 2046. BillTrack50. Introduced January 2024. ⤶
- Mississippi Senate Bill 2070; Mississippi House Bill 458; Mississippi House Bill 447. BillTrack50. Introduced January 2023, did not advance. ⤶
- Medicaid, Children’s Health Insurance Program, & Basic Health Program Eligibility Levels. Centers for Medicare and Medicaid Services. December 2023. ⤶
- How Many Uninsured Are in the Coverage Gap and How Many Could be Eligible if All States Adopted the Medicaid Expansion? KFF. March 2023. ⤶
- “October 2023 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed February 2024 ⤶
- ”3.7 Million People Would Gain Health Coverage in 2023 If the Remaining 12 States Were to Expand Medicaid Eligibility“, Matthew Buettgens and Urmi Ramchandani Urban Institute, July 2022 ⤶
- PHE Unwinding Reports. Mississippi Division of Medicaid. June through December 2023. ⤶ ⤶
- ”Last 11 States Should Expand Medicaid to Maximize Coverage and Protect Against Funding Drop as Continuous Coverage Ends“, Center on Budget and Policy Priorities, January 2023 ⤶
- “Medicare Monthly Enrollment” CMS.gov, April 2023. ⤶
- “Availability of short-term health insurance in Mississippi” healthinsurance.org, January 24, 2023 ⤶
- Unwinding Eligibility and Enrollment Data Reporting Template, June 2023 Monthly Report. Mississippi Division of Medicaid Eligibility Subsystem. Accessed January 2024. ⤶
- Monthly Report – December 2023. Mississippi Division of Medicaid Eligibility Subsystem. Accessed January 2024. ⤶
- HealthCare.gov Marketplace Medicaid Unwinding Report. Centers for Medicare and Medicaid Services. Accessed January 2024. ⤶
- September 2023 Medicaid & CHIP Enrollment Data Highlights, Medicaid.gov, Accessed January 2024 ⤶
- Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment. KFF. September 2023. Accessed January 2024. ⤶







