Medicare in California

“Birthday rule” gives CA Medigap enrollees an opportunity to switch plans
Key Takeaways
- More than 10% of all Medicare beneficiaries live in California.1
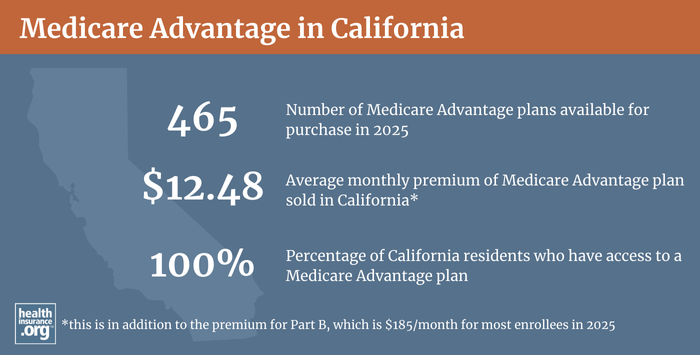
- Medicare Advantage plans are available in California, but plan availability varies significantly by county. 2
- Over half of California Medicare beneficiaries are enrolled in private Medicare Advantage plans.1
- 22 insurers offer Medigap plans in California 3and about 600,000 people have Medigap coverage in the state.4
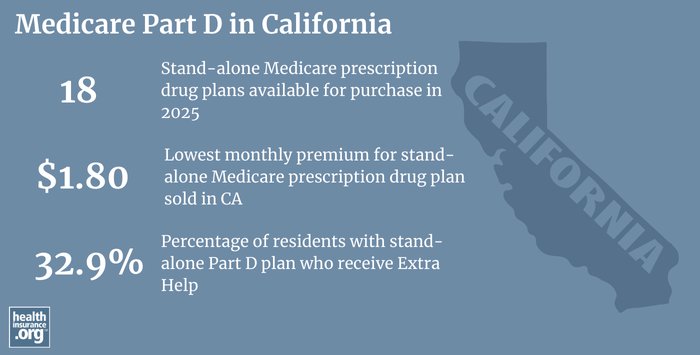
- California residents can select from among 18 stand-alone Part D prescription plans in 2025,5 with premiums starting at $1.80 per month5

Medicare enrollment in California
Nationwide, more than 67 million people are covered by Medicare6— and more than 10% of them are in California.1 As of June 2024, more than 6.8 million California residents had Medicare coverage.1 But that’s only about 16% of the state’s 39 million people, versus more about 19.5% of the United States population that is enrolled in Medicare.7
For most Americans, Medicare coverage enrollment goes along with turning 65. But Medicare eligibility is also triggered when a person has been receiving disability benefits for 24 months (people with ALS or end-stage renal disease do not have to wait 24 months for their Medicare enrollment). Nationwide, almost 11% of all Medicare beneficiaries are eligible due to disability.6 It’s lower in California, though, with under 8% of Medicare beneficiaries enrolled due to a disability.1
Medicare’s annual election period (October 15 to December 7 each year) allows Medicare beneficiaries the opportunity to switch between Medicare Advantage and Original Medicare and/or add or drop a Medicare Part D prescription plan. Medicare Advantage enrollees also have the option to switch to a different Advantage plan or to Original Medicare during the Medicare Advantage open enrollment period, which runs from January 1 to March 31.
Read our guide to Medicare’s open enrollment.
Learn about how California Medicaid (Medi-Cal) can assist Medicare beneficiaries with limited financial means. Note that under legislation California enacted in 2023, the state will pay Medicare Part A premiums for residents who are eligible for both Medicare and Medicaid (including some Medicare Savings Programs) and/or SSI benefits, if the person would otherwise have to pay a premium for Medicare Part A8 (most Medicare beneficiaries do not pay a premium for Part A, due to their work history).
Learn about Medicare plan options in California by contacting a licensed agent.



Explore our other comprehensive guides to coverage in California

We’ve created this guide to help you understand the California health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.
Learn about health insurance coverage options in California.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in California.


Learn about California’s Medicaid expansion, the state’s Medicaid enrollment and Medicaid eligibility.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage. Learn more about short-term plan availability in California.

Frequently asked questions about Medicare in California
What is Medicare Advantage?
Although Medicare is funded and run by the federal government, enrollees can choose whether they want to receive their benefits directly from the federal government via Original Medicare or enroll in a Medicare Advantage plan offered by a private insurer, if such plans are available in their area. There are pros and cons to Medicare Advantage and Original Medicare, and no single solution that works for everyone.
Although most counties in the United States do have Medicare Advantage plans available for purchase, Trinity County in northern California does not have any Medicare Advantage plans available for 2023. Of the 58 counties in California, Medicare Advantage plans are available in 57 of them as of 2023. Across those 57 counties, plan availability varies from just one or two plans in several rural counties to 67 plans in some parts of Los Angeles County.: 2
More than 3.5 million people are enrolled in Medicare Advantage in California (About 51% of California’s Medicare beneficiaries).1 Nationwide, Medicare Advantage enrollment had grown to about 50% of all beneficiaries.6
What are Medigap plans?
Original Medicare does not limit out-of-pocket costs, so most enrollees maintain some form of supplemental coverage. In 2020, over 14 million Original Medicare beneficiaries were enrolled in supplemental coverage.4 Medigap plans (also known as Medicare supplement insurance plans) are designed to pay some or all of the out-of-pocket costs (deductibles and coinsurance) that Medicare beneficiaries would otherwise have to pay themselves.
There are 22 insurers in California that offer Medigap plans.3 And as of 2020, there were about 600,000 California residents with Medigap coverage.4
Although California has by far the nation’s largest Medicare population, there were five states (Florida, Illinois, Ohio, Pennsylvania, and Texas) where more people were enrolled in Medigap plans as of 2020.
Medigap plans are sold by private insurers, but the plans are standardized under federal rules, with ten different plan designs (differentiated by letters, A through N). The benefits offered by a particular plan (Plan C, Plan K, etc.) are the same regardless of which insurer is selling the plan. So plan comparisons are much easier for Medigap policies than for other types of health insurance; consumers can base their decision on premiums (and how premiums change over time) and less tangible factors like customer service, since the benefits themselves are uniform. All Medigap insurers must offer at least Plan A. And if they offer any other plans, they must offer at least Plan C or Plan F to enrollees who were already eligible for Medicare prior to 2020, and at least Plan D or Plan G to enrollees who become eligible for Medicare in 2020 or beyond.
California does not dictate how Medigap insurers can adjust premiums based on age, so most Medigap insurers in the state use attained-age rating, which means that premiums increase as a person gets older. There are a few insurers in California that use issue-age rating instead, with premiums based on the age the person was when they enrolled. Community rating (also known as “no age” rating) means that rates do not vary with age at all, but there are no Medigap insurers in California that use community rating (several states require community rating or issue-age rating, but California is not among them).
Unlike other private Medicare coverage (Medicare Advantage plans and Medicare Part D plans), federal rules do not provide an annual open enrollment window for Medigap plans. Instead, federal rules provide a one-time six-month window when Medigap coverage is guaranteed-issue. This window starts when a person is at least 65 and enrolled in Medicare Part B (you must be enrolled in both Part A and Part B to buy a Medigap plan).
However, California law has long given Medigap enrollees an annual window, following their birthday, when they can switch to any other Medigap plan with equal or lesser benefits, without medical underwriting. This window used to be 30 days long, but legislation enacted in 2019 extended it to 60 days, as of 2020. California is one of several states that have this type of “birthday rule” that allows Medigap enrollees an opportunity to make limited plan changes without underwriting.
People who aren’t yet 65 can enroll in Medicare if they have amyotrophic lateral sclerosis (ALS) or end-stage renal disease (ESRD), or if they’re disabled and have been receiving disability benefits for at least two years, and about 511,000 Medicare beneficiaries in California are under 65.1 Federal rules do not guarantee access to Medigap plans for people who are under 65, but the majority of the states, including California, have stepped in to ensure at least some access to private Medigap plans for disabled enrollees under the age of 65 (federal legislation, including 2018’s H.R.6431, has been considered to expand access to Medigap plans to all Medicare beneficiaries, regardless of age, but the rules have thus far not changed).
For Medicare beneficiaries in California who are under age 65, Article 6 (Section 10192.11) of California’s insurance statute requires Medigap insurers in the state to offer at least plans A, B, D, and G (if offered by the company to any applicants; note that this used to be plans A, B, C, and F, but S.B.784 was enacted in 2019 to swap Plans C and F for Plans D and G, since Plans C and F are no longer available — nationwide — to newly-eligible Medicare beneficiaries as of 2020; the requirement to make plans C and F — if offered by the insurer — available is still applicable for disabled Medicare beneficiaries who became eligible for Medicare prior to 2020). The insurers must also offer either plan K or Plan L, if offered by the company, or Plan M or Plan N, if offered by the company. But none of these provisions apply to Medicare beneficiaries under age 65 who are eligible for Medicare due to having end-stage renal disease (kidney failure).
This is important, because prior to 2021, federal rules also allowed Medicare Advantage plans to reject new applicants with end-stage renal disease, unless the plan was a special needs plan specifically designed for ESRD patients (such plans were not available in most of the state, meaning that ESRD patients had no option to cap their out-of-pocket costs unless they had access to a supplemental employer-sponsored or retiree plan). But this changed as of 2021, under the 21st Century Cures Act. Starting with 2021 coverage, Medicare Advantage plans are guaranteed-issue for all Medicare beneficiaries, including those with ESRD.
California’s statute allows Medigap insurers to charge higher premiums for people under age 65. But coverage must be guaranteed-issue during the six months after a person enrolls in Medicare Part B (regardless of age) or the six months after a person is determined to be retroactively eligible for Medicare Part B. And insurers cannot pay differing broker commissions based on the age of the Medigap enrollee (ie, insurers are not allowed to use lower commissions to dissuade brokers from selling Medigap plans to people under age 65).
Although the Affordable Care Act eliminated pre-existing condition exclusions in most of the private health insurance market, those regulations don’t apply to Medigap plans. Medigap insurers can impose a pre-existing condition waiting period of up to six months, if you didn’t have at least six months of continuous coverage prior to your enrollment. And if you apply for a Medigap plan after your initial enrollment window closes (assuming you aren’t eligible for one of the limited guaranteed-issue rights), the insurer can look back at your medical history in determining whether to accept your application, and at what premium.
What is Medicare Part D?
Original Medicare does not cover outpatient prescription drugs. More than half of Original Medicare beneficiaries have supplemental coverage via an employer-sponsored plan or Medicaid, and these plans often include prescription coverage. But Medicare enrollees without creditable drug coverage need to obtain Medicare Part D prescription coverage. Part D coverage can be purchased as a stand-alone plan, or as part of a Medicare Advantage plan that includes integrated Part D prescription drug coverage.
Insurers in California are offering 18 stand-alone Part D plans for sale in 2025,5 with premiums starting at $1.80/month.5 As of June 2024, there were more than 5.7 million Medicare beneficiaries in California with Part D prescription coverage.1 Over 2.3 million beneficiaries had stand-alone Medicare Part D plans, while more than 3.4 million had Medicare Advantage plans with built-in Part D coverage.1
Medicare Part D enrollment is available when a beneficiary is first eligible for Medicare, and also during the annual open enrollment period each fall, from October 15 to December 7.
How does Medicaid provide financial assistance to Medicare beneficiaries in California?
Many Medicare beneficiaries receive financial assistance through Medicaid with the cost of Medicare premiums, prescription drug expenses, and services not covered by Medicare – such as long-term care.
Our guide to financial assistance for Medicare enrollees in California includes overviews of these benefits, including Medicare Savings Programs, long-term care coverage, and eligibility guidelines for assistance.
What additional resources are available for Medicare beneficiaries and their caregivers in California?
Need help with Medicare enrollment in California, or have questions about Medicare eligibility in California?
- HICAP, California’s Health Insurance Counseling and Advocacy Program, is a helpful resource. Access their website or call 1-800-434-0222.
- California’s Department of Insurance, which oversees Medigap plans in California, has a helpful summary of state rules and regulations related to Medigap plans, and a general guide to Medigap plans in California.
- HICAP and the California Department of Aging also have a helpful toolkit for avoiding Medicare fraud and abuse.
- The Medicare Rights Center website provides information geared to Medicare beneficiaries, caregivers, and professionals.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in California?
Explore more resources for options in California including ACA coverage, short-term health insurance, dental insurance and Medicaid.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- “Medicare Monthly Enrollment – California.” Centers for Medicare & Medicaid Services Data, June, 2024. ⤶ ⤶ ⤶ ⤶ ⤶ ⤶ ⤶ ⤶ ⤶
- ”Medicare Advantage 2024 Spotlight: First Look” KFF.org Nov. 15, 2023 ⤶ ⤶
- “Explore your Medicare coverage options.” Medicare.gov. Accessed October, 2024. ⤶ ⤶
- ”The State of Medicare Supplement Coverage” AHIP. May 2024 ⤶ ⤶ ⤶
- ”Fact Sheet: Medicare Open Enrollment for 2025” (14) Centers for Medicare & Medicaid Services. Sep. 27, 2024 ⤶ ⤶ ⤶ ⤶
- “Medicare Monthly Enrollment – US.” Centers for Medicare & Medicaid Services Data, June, 2024. ⤶ ⤶ ⤶
- “U.S. Census Bureau Quick Facts: United States & California.” United States Census Bureau. Accessed October, 2024. ⤶
- ”Medicare Part A buy-in and automatic enrollment of Supplemental Security Income recipients into Qualified Medicare Beneficiary Program.” California Department of Health Care Services. December, 2024. ⤶

