Guide to women’s health insurance

Learn how individual health insurance plans cover women’s healthcare services, including maternity, contraception and abortion.

Women’s health coverage
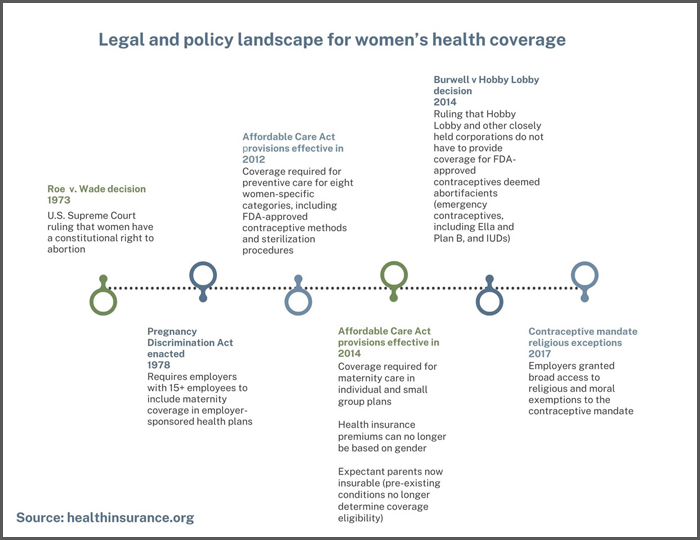
For women in the U.S., access to affordable coverage in the individual health insurance market has improved markedly over the past decade – due in large part to coverage improvements and consumer protections delivered by the Affordable Care Act.
Prior to the ACA’s implementation, which began mostly in 2014, women faced many barriers to coverage:
- Previously, more than half of individual plans charged higher premiums for a 40-year-old female non-smoker than for a 40-year-old male smoker – for the exact same coverage.
- More than 90% of individual health plans didn’t provide any routine maternity benefits.
- In all but five states, being pregnant was a pre-existing condition that prevented a woman from purchasing individual health insurance.
- Many individual health plans offered no contraceptive coverage.
- Coverage for women’s preventive care varied considerably from one state to another.
Suggested reading:
- Women, health insurance and the Affordable Care Act
- What is the ACA’s preventive health services coverage mandate?
We hope you’ll use this guide to get a clearer understanding of how coverage has improved – and what you should expect for coverage of women’s healthcare when you’re selecting a health plan.
Find affordable health insurance coverage that best suits your needs.
Get your free quote through a licensed insurance agent!



Preventive care for women under the Affordable Care Act (ACA)
Prior to implementation of the Affordable Care Act, coverage of women’s preventive care varied considerable from state to state. But beginning in August 2012, all health plans (other than grandfathered health plans) were required to provide coverage for certain women-specific categories of preventive care:
- Well-woman visits
- Gestational diabetes screening
- HPV testing
- Screening and counseling for domestic violence
- HIV testing and counseling for sexually transmitted infections
- Breastfeeding supplies
- Contraception and family planning counseling
(Note that additional preventive care mandates, including preventive care for children and all adults as well as additional woman-specific preventive care, took effect in 2014.)
Recent news
Access to women’s health care services was greatly expanded under the ACA. This was due not just to the ACA’s coverage mandates (for things like preventive care and maternity care), but also to the fact that the ACA resulted in far more women having health coverage. Medicaid expansion, the employer mandate, and access to subsidized coverage in the health insurance exchange/Marketplace have all played a role in this.
But women’s health coverage and care continue to be controversial topics, and the rules continue to evolve over time.
- Statement on 2022 Supreme Court ruling overturning Roe v. Wade
- Supreme Court upholds broad exemptions to ACA’s contraceptive mandate
- Biden administration proposed rule change to expand access to contraception (Proposed in early 2023, but not yet finalized as of late 2024.) This would limit exemptions from the contraceptive coverage mandate to only religious objections, removing the moral objection pathway. Would also provide a way for women to obtain zero-cost contraception even if their plan issuer has an exemption; rules put in place by the Trump administration made this accommodation process optional.
- 2024 FAQs to clarify health plan compliance with the ACA’s contraceptive coverage requirement.
Coverage of women's healthcare services

Prior to 2014, just 12% of individual-market health plans included maternity benefits. But the Affordable Care Act has been a game-changer. Maternity care is one of the essential health benefits that must be included on all individual and small-group policies. And women are no longer charged higher premiums than men, despite the fact that every new major medical health policy includes maternity coverage.
And coverage is guaranteed-issue during open enrollment and special enrollment periods, regardless of medical history. That means that an expectant parent can now obtain coverage in every state during open enrollment or during a special enrollment period triggered by a qualifying event.


Treatment for infertility is not one of the Affordable Care Act’s essential benefits, and coverage for infertility treatment is not mandated by the ACA or any other federal law. But some states have regulations that go beyond the minimum requirements laid out by the federal government with their own laws, regulations, and mandates.
These state rules only apply to state-regulated plans, which include health plans that individuals and businesses purchase from an insurance company. Self-insured employer-sponsored health plans (which cover the majority of people who have employer-sponsored health coverage) are not subject to state insurance rules.
Recommended reading:


Abortion coverage is neither required nor banned under the ACA. But federal funds — including premium subsidies in the marketplace and federal funding for Medicaid and Medicare — cannot be used to pay for abortion unless the situation involves rape, incest, or danger to the mother’s life. Coverage for other abortions varies considerably from one health plan to another.


The Affordable Care Act improved access to highly effective, long-term contraceptives, without a cost barrier. Under the ACA, health policies that took effect on or after August 1, 2012 are required to cover — with no cost-sharing — at least one version of each FDA-approved contraceptive method for women. This includes sterilization, IUDs, and implants, which often had considerable up-front costs prior to the ACA.
Recommended reading:

Frequently asked questions about women's health coverage
Does the ACA require infertility treatment to be covered by health insurance?
Infertility treatment is not an essential health benefit under the ACA. However, 21 states and DC have laws that require at least some coverage for infertility treatment on at least some state-regulated health plans.
State-regulated plans include plans that individuals and businesses purchase from an insurance company. Self-insured health plans are not regulated by state insurance rules.
Is contraception covered by health insurance?
Under the ACA’s rules, health plans effective on or after August 1, 2012 are required to provide all FDA-approved contraceptive methods for women, including sterilization, with no cost-sharing. This means that at least one version of every type of contraceptive is covered at no cost to a patient.
But plan issuers with moral or religious objections can get an exemption from the contraceptive coverage mandate. And although the Obama administration created an accommodation that would allow women on exempt plans to obtain zero-cost contraception, the Trump administration made that accommodation optional for plan issuers.
However, the Biden administration proposed a rule change in 2023 that would eliminate the moral objection pathway for an exemption, and that would also ensure access to zero-cost contraception even if a woman is covered by a plan that has a religious exemption.
The Centers for Medicare and Medicaid Services issued FAQs in 2022 and 2024 clarifying a variety of details about contraceptive coverage. They note, for example, that health plans must fully cover necessary services that go along with tubal ligation, such as anesthesia, and that emergency contraception must be covered just like other forms of contraception.
How can I find a health plan that covers maternity care?
The ACA mandates that maternity coverage is included on all ACA-compliant individual and small group health plans nationwide. And large group health plans have been required to cover maternity care since the 1970s.1
Thanks to the ACA, being pregnant is no longer considered a pre-existing condition, which means pregnant women (and expectant fathers) can buy health insurance in the individual market in every state — assuming they are applying during open enrollment or have a qualifying event that allows them to enroll.
In DC and several states that run their own exchanges/Marketplaces, pregnancy itself is considered a qualifying life event that will allow the pregnant woman to enroll in health coverage without having to wait until the baby is born (nationwide, birth is a qualifying life event).
Do ACA health plans coverage abortion?
Whether your ACA plan covers abortion depends on the state where you live. In more than half of the states, health plans sold through the Marketplace are not allowed to cover abortions except for circumstances involving rape, incest, or the mother’s life being in danger. However, ten states (increasing to 11 as of mid-2025) require all state-regulated health plans to cover abortion services.
Footnotes
- ”Pre-ACA State Maternity Coverage Mandates: Individual and Small Group Markets” KFF.org. Accessed Oct. 14, 2024 ⤶









