Home > Health insurance Marketplace > Arizona
Arizona Marketplace health insurance in 2025

Compare ACA plans and check subsidy savings from a third-party insurance agency.

Arizona health insurance Marketplace guide
This guide was created to help you better understand the Arizona health insurance Marketplace and pick the right health plan for you and your family. For many, an Affordable Care Act (ACA) Marketplace (exchange) plan – also called an Obamacare plan – may be a good choice.
Arizona uses the federally-facilitated Marketplace, so residents enroll through HealthCare.gov. Eight private insurance companies will offer coverage through Arizona’s health insurance Marketplace for 2025, with varying coverage areas.3 There were also eight insurers in the Arizona Marketplace in 2024,4 but there is one new insurer for 2025 and one exiting insurer (details below).
Marketplace plans are used by people who need to buy their own insurance, including those who are self-employed, workers at small businesses without health benefits, and early retirees under 65 who need coverage until Medicare.
Frequently asked questions about health insurance in Arizona
Who can buy Marketplace health insurance?
To buy Marketplace health coverage in Arizona:5
- You must live in Arizona.
- You must be lawfully present in the U.S.
- You can’t be incarcerated.
- You can’t be enrolled in Medicare.
To qualify for financial assistance (which depends on your household income) through the Arizona Health Insurance Marketplace:
- You can’t be eligible for affordable coverage offered by an employer. You can use this tool to see if the employer-sponsored coverage available to you is considered affordable.
- You can’t be eligible for AHCCCS (Medicaid) or KidsCare (CHIP)
- You can’t be eligible for premium-free Medicare Part A.6
- If married, file a joint tax return.7
- Not be able to be claimed by someone else as a tax dependent.7
When can I enroll in an ACA-compliant plan in Arizona?
Arizona’s open enrollment period to sign up for ACA Marketplace individual and family health plans is between November 1 and January 15. The enrollment window applies whether you enroll through the exchange or directly with an insurer.
If you want your coverage to begin on January 1, enroll by December 15. If you sign up between December 16 and January 15, your coverage will start on February 1.
If the open enrollment deadline passes, you may still be able to sign up for or make changes to an ACA Marketplace health plan through a special enrollment period (SEP). To qualify for a SEP, you’ll generally need a qualifying life event.
But there are instances where you don’t need a specific qualifying life event to apply outside of open enrollment. For example:
- If you’re eligible for premium tax credits and your income is not more than 150% of the poverty level, you can enroll anytime.
- If you’re part of the American Indian/Alaska Native population, you can enroll whenever necessary.
If you lose AHCCCS or KidsCare (Medicaid/CHIP) coverage between March 31, 2023 and November 30, 2024, you can enroll through the extended SEP.8
How do I enroll in a Marketplace plan in Arizona?
Here are the main ways to enroll in a Marketplace health plan in Arizona:
- Directly through HealthCare.gov
- By phone at (800) 318-2596 (TTY: 1-855-889-4325). Talk to an agent 24 hours a day, seven days a week, except for holidays.
- With the help of a local agent/broker, Navigator, or certified application counselor.
- Via an approved enhanced direct enrollment entity (EDE).9 (Make sure you request an on-exchange enrollment if that’s your preference, as EDEs can also generally enroll you in off-exchange coverage if you prefer that.)
How can I find affordable health insurance in Arizona?
In Arizona, individuals and families can generally find affordable health insurance coverage by shopping on HealthCare.gov, which is Arizona’s health insurance Marketplace. The Marketplace offers two different types of income-based subsidies:
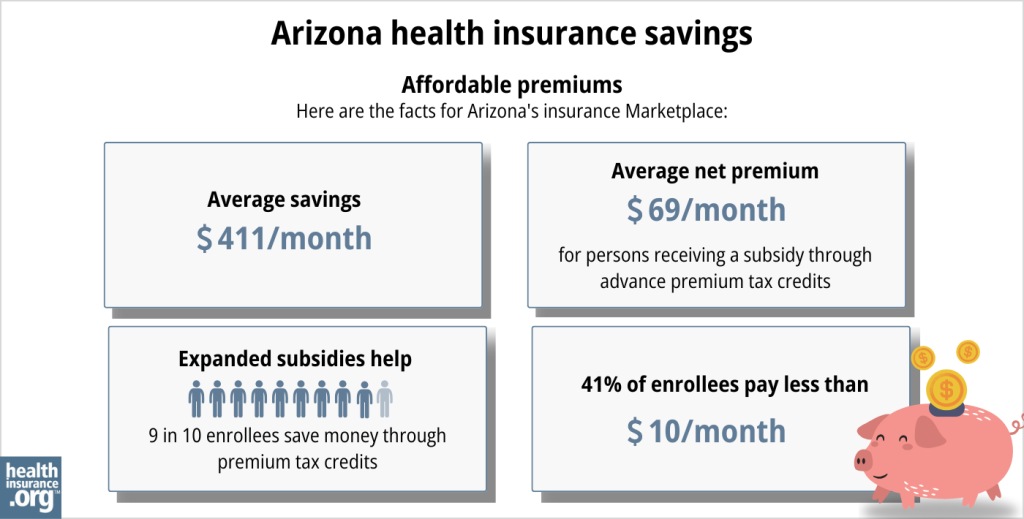
- Premium subsidies: Depending on your household income, you could be eligible for subsidies known as Advance Premium Tax Credits (APTC) that help lower your monthly premiums. About 90% of Marketplace enrollees in Arizona qualified for premium subsidies in 2024, saving on average $453 monthly. With subsidies, enrollees paid an average of $115 per month for health coverage.10 (Note that these numbers are based on effectuated enrollment; the metrics and data in the chart below are different and are based on all applications submitted during the open enrollment period for 2024 coverage.)
- Cost-Sharing Reductions: If your income is no more than 250% of the federal poverty level11 and you select a Silver-level plan, you can receive cost-sharing reductions (CSR) in addition to APTC. CSRs help reduce your out-of-pocket costs, making medical care more affordable when you need it.12
Source: CMS.gov13
Medicaid: If you’re eligible for Medicaid, you can enroll through the Arizona Health Care Cost Containment System (azahcccs.gov) or Health-e-Arizona (healthearizonaplus.gov).
Short-Term Health Insurance: Consider short-term health insurance if you need a more budget-friendly option and are either ineligible for Marketplace subsidies or Medicaid, or missed the enrollment window for a Marketplace plan (in that case, you’ll want to make sure you go back to the Marketplace to enroll during the next open enrollment window, which begins November 1 each year).
How many insurers offer Marketplace coverage in Arizona?
Eight private insurance companies will offer coverage through Arizona’s health insurance Marketplace for 2025, with varying coverage areas.3 There were also eight insurers in the Arizona Marketplace in 2024,4 but Medica is leaving the Arizona market at the end of 2024, and Antidote Health Plan is new for 2025.
In 2024, only one carrier offered coverage statewide; the rest had varying coverage areas. In some areas of the state, plans were only available from one insurer.14
Are Marketplace health insurance premiums increasing in Arizona?
In Arizona’s individual/family insurance market, the following average rate changes have been approved for 2025, applicable to full-price plans (meaning before subsidies are applied):
Arizona’s ACA Marketplace Plan 2025 APPROVED Rate Increases by Insurance Company |
|
|---|---|
| Issuer | Percent Increase |
| Aetna CVS Health/Banner Health | 10.35% |
| Cigna HealthCare of AZ, Inc. | 3.92% |
| Blue Cross and Blue Shield of Arizona HMO | 5.36% |
| Blue Cross and Blue Shield of Arizona PPO | 7.05% |
| Imperial Insurance | -2.52% |
| Arizona Complete Health (Health Net of AZ) | -6.1% |
| Medica Community Health Plan | exiting the market |
| Oscar Health Plan, Inc. | 0.3% |
| UnitedHealthcare of Arizona, Inc. | 3.19% |
| Antidote Health Plan of Arizona | new for 2025 |
Source: Arizona Department of Insurance and Financial Institutions3
When looking at overall average rate changes, it’s important to understand:
- Published rates are for full-price plans. Most Arizona Health Insurance Marketplace enrollees receive premium subsidies,10 so their net rate change also depends on how much their subsidy changes.
- Averages don’t account for premiums increasing with age. People pay more each year as they get older.
- A weighted average lumps all plans together. But rate changes vary by insurer (as noted above) and plan.
For perspective, here’s a summary of how average pre-subsidy premiums have changed over time in Arizona’s individual/family health insurance market:
- 2015: Average decrease of 3%15
- 2016: Average increase of 12.3%16
- 2017: Average increase of 57%17
- 2018: Nearly flat rate for the two on-exchange insurers18
- 2019: Average decrease of 6.3%19
- 2020: Average decrease of 0.2%20
- 2021: Average increase of 0.4%21
- 2022: Average increase of 0.5%22 (three new insurers joined the exchange)
- 2023: Average increase of 4.3%23
- 2024: Average increase of 0.3%24
How many people are insured through Arizona’s Marketplace?
During the open enrollment period for 2024 coverage, 348,055 people signed up for private health plans through Arizona’s exchange.25
This was by far a record high (see chart below). The increase in enrollment was driven in large part by the enhanced premium subsidies available as a result of the American Rescue Plan and Inflation Reduction Act.26 But the 2024 enrollment spike was also driven by the “unwinding” of the pandemic-era Medicaid continuous coverage rule. According to CMS, more than 134,000 people had transitioned from Arizona Medicaid to a Marketplace plan by April 2024, during the unwinding process.27

Source: 2014,28 2015,29 2016,30 2017,31 2018,32 2019,33 2020,34 2021,35 2022,36 2023,37 2024,38 202539
What health insurance resources are available to Arizona residents?
HealthCare.gov
The official federal website where you can sign up for health insurance plans through the ACA Marketplace.
Arizona Department of Insurance
Regulates and licenses health plans, agents, and brokers. Provides consumer information about insurance.
Arizona Health Matters
A resource that provides information about health concerns in Arizona.
Arizona Association of Community Health Centers/Arizona Alliance for Community Health Centers
Community health centers that are also Arizona’s federally-funded Navigator. Help with exchange enrollments.
Arizona Health Care Cost Containment System
Administers Medicaid in Arizona. Provides coverage to low-income residents.
Medicare Rights Center
National service with a website and call center to assist Medicare beneficiaries and their caregivers.
Arizona State Health Insurance Assistance Program
Local counseling, advice, and assistance with Medicare issues.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Arizona?
Explore more resources for options in Arizona including short-term health insurance, dental insurance, Medicaid and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”2025 OEP State-Level Public Use File (ZIP)” Centers for Medicare & Medicaid Services, Accessed May 13, 2025 ⤶ ⤶
- ”Rate Review Submissions” RateReview.HealthCare.gov. Accessed Jan. 7, 2025 ⤶
- ”Individual and Small Group ACA Health Insurance Rate Changes” Arizona Department of Insurance and Financial Institutions. Sep. 16, 2024 ⤶ ⤶ ⤶
- “Insurers Offering Individual/Family Health Insurance in Arizona for Plan Year 2024” Arizona Department of Insurance and Financial Institutions. Accessed December 2023. ⤶ ⤶
- “A quick guide to the Health Insurance Marketplace” HealthCare.gov ⤶
- Medicare and the Marketplace, Master FAQ. Centers for Medicare and Medicaid Services. Accessed November 2023. ⤶
- Premium Tax Credit — The Basics. Internal Revenue Service. Accessed May 10, 2024 ⤶ ⤶
- ”HHS Takes Additional Actions to Help People Stay Covered During Medicaid and CHIP Renewals” CMS Newsroom. Mar. 28, 2024 ⤶
- “Entities Approved to Use Enhanced Direct Enrollment” CMS.gov, April 28, 2023 ⤶
- ”Effectuated Enrollment: Early 2024 Snapshot and Full Year 2023 Average” CMS.gov, July 2, 2024 ⤶ ⤶
- “Federal Poverty Level (FPL)” HealthCare.gov, 2023 ⤶
- APTC and CSR Basics. Centers for Medicare and Medicaid Services. June 2023. ⤶
- “2025 Marketplace Open Enrollment Period Public Use Files” CMS.gov, May 2025 ⤶
- Plan Year 2024 Qualified Health Plan Choice and Premiums in HealthCare.gov Marketplaces. Centers for Medicare and Medicaid Services. October 25, 2023. ⤶
- Analysis Finds No Nationwide Increase in Health Insurance Marketplace Premiums. The Commonwealth Fund. December 2014. ⤶
- FINAL PROJECTION: 2016 Weighted Avg. Rate Increases: 12-13% Nationally* ACA Signups. October 2015. ⤶
- Avg. UNSUBSIDIZED Indy Mkt Rate Hikes: 25% (49 States + DC). ACA Signups. October 2016. ⤶
- Major Medical Health Insurance Rate Filings and Final Rate Changes Effective Date January 1, 2018. Arizona Department of Insurance. October 2017. ⤶
- 2019 Rate Hikes. ACA Signups. October 2018. ⤶
- 2020 Rate Changes. ACA Signups. October 2019. ⤶
- Calculated by healthinsurance.org, based on approved rates and enrollment data in SERFF filings: Market share was as follows: 28% BCBSAZ; 15% Bright Health; 5% Cigna; 49% Health Net; 3% Oscar. Accessed December 2023. ⤶
- 2022 Rate Changes. ACA Signups. October 2021. ⤶
- UPDATED: FINAL Unsubsidized 2023 Premiums: +6.2% Across All 50 States +DC. ACA Signups. Accessed November 2023. ⤶
- So How’d I Do On My 2024 Avg. Rate Change Project? Not Bad At All! ACA Signups. December 2023. ⤶
- ”Health Insurance Marketplaces 2024 Open Enrollment Period Report” CMS.gov. March 22, 2024 ⤶
- Health Insurance Marketplaces 2023 Open Enrollment Report. Centers for Medicare and Medicaid Services. Accessed December 2023. ⤶
- ”HealthCare.gov Marketplace Medicaid Unwinding Report” Centers for Medicare & Medicaid Services. Data through April 2024; Accessed Aug. 14, 2024. ⤶
- “ASPE Issue Brief (2014)” ASPE, 2015 ⤶
- “Health Insurance Marketplaces 2015 Open Enrollment Period: March Enrollment Report”, HHS.gov, 2015 ⤶
- “HEALTH INSURANCE MARKETPLACES 2016 OPEN ENROLLMENT PERIOD: FINAL ENROLLMENT REPORT” HHS.gov, 2016 ⤶
- “2017 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2017 ⤶
- “2018 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2018 ⤶
- “2019 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2019 ⤶
- “2020 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2020 ⤶
- “2021 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2021 ⤶
- “2022 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2022 ⤶
- “Health Insurance Marketplaces 2023 Open Enrollment Report” CMS.gov, 2023 ⤶
- ”HEALTH INSURANCE MARKETPLACES 2024 OPEN ENROLLMENT REPORT” CMS.gov, 2024 ⤶
- “2025 Marketplace Open Enrollment Period Public Use Files” CMS.gov, May 2025 ⤶

