Home > Health insurance Marketplace > Illinois
Illinois Marketplace health insurance in 2025

Compare ACA plans and check subsidy savings from a third-party insurance agency.

Illinois health insurance Marketplace guide
Illinois runs a partnership exchange with the federal government. The state operates Get Covered Illinois, which has a website, in-person help, and a help desk,3 but Illinois residents use the federally-facilitated HealthCare.gov platform to enroll in Affordable Care Act (ACA) Marketplace health plans.
But starting in the fall of 2025, for coverage effective in 2026, Illinois will have its own state-based enrollment platform.4
Eleven insurance companies offer Marketplace coverage in Illinois for 2025,5 with service areas that vary quite a bit from one insurer to another.6
Use this guide to help you understand the Illinois Marketplace and choose the right health plan for you and your family. ACA Marketplace plans – or Obamacare or exchange – are affordable choices for many people. Enrolling on the exchange may make you eligible for financial assistance through an advance premium tax credit.
Frequently asked questions about health insurance in Illinois
Who can buy Marketplace health insurance?
You can buy a health plan through the exchange if:7
- You reside in the United States.
- You are a U.S. citizen or national.
- You are not incarcerated.
- You are not already covered Medicare.
Qualification for financial assistance, including premium subsidies and cost-sharing reductions (CSR), depends on your income and how it compares with the cost of the second-lowest-cost Silver plan in your area. This can vary based on where you live and your age. Moreover, to be eligible for financial aid for your Marketplace plan, you must:
- Not have affordable health coverage available through your job or your spouse’s job. If you have access to employer-sponsored insurance, but it seems too expensive, you can use our Employer Health Plan Affordability Calculator to see if you might be eligible for premium subsidies on the Marketplace.
- Not qualify for Medicaid or CHIP.
- Not be eligible for premium-free Medicare Part A.8
- If married, file a tax return jointly with your spouse9 (with very limited exceptions)10
- Not be able to be claimed by someone else as a tax dependent.11
When can I enroll in an ACA-compliant plan in Illinois?
In Illinois, open enrollment for ACA Marketplace individual and family health coverage is from November 1 through January 15.12
You can sign up for an exchange plan — or make changes to your coverage — outside of open enrollment if you meet special enrollment period (SEP) requirements.13 This generally means you must have a qualifying life event, such as losing your health insurance, getting married, or having a baby.
But some special enrollment periods don’t require a specific qualifying event. So if the open enrollment deadline has passed and you haven’t experienced a qualifying event, you may still be able to sign up for an ACA plan. For example:
- If you’re eligible for premium tax credits and your income is not more than 150% of the poverty level, you can enroll anytime.14
- If you’re a Native American, you can enroll anytime.15
For those who lose Medicaid or CHIP coverage between March 31, 2023 and November 30, 2024, an extended SEP allows you to enroll anytime during that window.16
Illinois legislation (HB5142) was enacted in 2022 that created an easy enrollment program, which became available as of early 2023, when 2022 tax returns were being filed.
For the time being, Illinois cannot offer a special enrollment period for marketplace plans in conjunction with the easy enrollment program, because using the federally-facilitated exchange means there cannot be state-specific SEP opportunities. That will change as of 2026, when Illinois is running its own exchange platform.
For now, Illinois residents can indicate on their state tax return whether they’d like their information to be shared with applicable state agencies (This is Step 12 on the 2023 Illinois state tax return).
If the person is found to be eligible for Medicaid or CHIP, the state can notify them and help them enroll, since those programs have year-round enrollment.17
During the 2024 legislative session, Illinois enacted a bill that will create a special enrollment period triggered by pregnancy beginning in 2026, once Illinois is running its own Marketplace enrollment platform.18
How do I enroll in a Marketplace plan in Illinois?
Here are the ways to enroll in a Marketplace health plan in Illinois:
- Online: You can sign up directly through HealthCare.gov, the federal Marketplace website. (Starting in the fall of 2025, Illinois will no longer use HealthCare.gov, and will instead use Get Covered Illinois as the enrollment platform.)
- By Phone: Dial 1-800-318-2596 (TTY: 1-855-889-4325) to enroll over the phone with a Marketplace representative. The call center is available 24 hours a day, seven days a week, but it’s closed on holidays.
- In-person: Enrollment assistance is also available from trained Navigators and assisters who can answer your questions. Go to localhelp.HealthCare.gov or getcovered.illinois.gov to find in-person assistance in your area.
- With the help of a broker or via an approved enhanced direct enrollment entity.19 (Note that EDEs can also offer off-exchange plans and non-ACA-compliant plans. If you’re working with an EDE, be clear in specifying what type of coverage you want. Keep in mind that you can only get subsidies if you choose a Marketplace plan.)
How can I find affordable health insurance in Illinois?
Individuals and families who enroll in Marketplace coverage in Illinois can take advantage of two different types of income-based financial assistance:
- Premium subsidies: The ACA Marketplace is the only place where you can qualify for income-based subsidies known as Advance Premium Tax Credits (APTC) that help lower your monthly premiums. Nearly nine out of 10 Illinois exchange enrollees were eligible for subsidies on 2024 plans, saving an average of $545 monthly with premium tax credits in Illinois. As a result, the average after-subsidy monthly premium was $141 for people who qualified for APTC.20
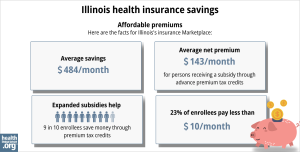
Source: CMS.gov21
- Cost-Sharing Reductions: You may qualify for cost-sharing reductions (CSR) if your income is no more than 250% of the federal poverty level. CSRs help reduce your out-of-pocket costs, making coverage more affordable. Forty-seven percent of the people who enrolled via the Illinois Marketplace during the open enrollment period for 2024 coverage selected plans that included CSR benefits.22
Medicaid: Illinois residents may qualify for affordable Medicaid coverage if eligible.
Short-Term Health Insurance: For people who are not eligible for subsidies, Medicare, or Medicaid, short-term health insurance may offer a more budget-friendly option. However, Illinois enacted legislation in 2024 that calls for a ban on the sale of short-term health insurance in the state, starting in January 2025.23
How many insurers offer Marketplace coverage in Illinois?
Eleven insurance companies offer Marketplace coverage in Illinois for 2025.5 But the number of carriers offering plans varies quite a bit from one part of the state to another,6 since each carrier sets its own service area.
Twelve insurers offered Marketplace plans in Illinois for 2024, up from 11 in 2023.24 But one of the existing insurers (Medica, formerly WellFirst/SSM) was not listed among the carriers that filed rates and plans for 2025.25 Illinois residents with Medica Marketplace coverage in 2024 need to select a new plan for 2025.
Are Marketplace health insurance premiums increasing in Illinois?
The following average premium changes were approved for 2025 for the insurers that offer Marketplace coverage in Illinois,26
Illinois’ ACA Marketplace Plan 2025 APPROVED Rate Increases by Insurance Company |
|
|---|---|
| Issuer | Percent Increase |
| Aetna Health | 6.94% |
| Aetna Life Insurance | 2.03% |
| Celtic Insurance Co. (Ambetter) | -4.1% |
| Cigna HealthCare of Illinois, Inc. | 6.4% |
| Health Alliance Medical Plans, Inc. (HAMP) | 10.05% |
| Health Care Service Corporation (Blue Cross Blue Shield of Illinois) | 6.6% |
| Quartz Health Benefit Plans Corporation | 9.9% |
| MercyCare HMO | 5.37% |
| Molina Healthcare of Illinois, Inc. | 1.6% |
| Oscar Health Plan, Inc. | 11.7% |
| UnitedHealthcare | 1.46% |
| Medica (formerly WellFirst Health/SSM Health Plan) | Exiting market |
Source: Illinois Department of Insurance26
Illinois historically had very little transparency in terms of rate filing details for health plans, and state regulators have not had the authority to modify or reject rate changes proposed by insurers. But that will change as of the 2026 plan year (for rates filed in 2025), due to a new law that was enacted in 2023.27
And for the 2025 plan year, the Illinois Department of Insurance debuted a new summary page that contains an overview of the rate changes that insurers have filed, along with some of the filing details (final rates were added as open enrollment got underway).25 Although summary pages like this have long been displayed on many states’ insurance department websites, that was not the case in Illinois before 2024.
Illinois lawmakers have also enacted legislation that will call for a state-regulated factor that will be added to all silver-level plans starting in 2026.28 This is also known as “premium alignment” and it should result in gold plans becoming relatively less expensive than silver plans, for people who aren’t eligible for cost-sharing reductions. Texas, New Mexico, and Pennsylvania all have similar protocols, and Vermont will join them in 2025.
For perspective, here’s how average individual/family health insurance premiums have changed in Illinois over the years. Note that in Illinois, average rate changes are typically published based on rate changes for the lowest-cost plan at each metal level, rather than overall rate changes, which differs from how this information has typically been presented in other states (here’s an example, for 2025 coverage). And weighted averages have not typically been available in Illinois, due to the lack of transparency in the rate filing process. This should change in future years, under the terms of the state’s new law.
- 2015: Average increases ranged from 2.6% to 11%.29
- 2016: Average increases ranged from 5.3% to 11.3%.30
- 2017: Overall average increase of 45.1%.31
- 2018: Overall average increase of 30%.32
- 2019: Average rate changes generally ranged from -4% to +6%.33
- 2020: Average rate decrease of 0.3%.34
- 2021: Relatively flat rates for most insurers35
- 2022: Average increase of roughly 5%.36
- 2023: Average increase of roughly 7%37
- 2024: Average increase of 5.7%38
How many people are insured through Illinois’ Marketplace?
398,814 people signed up for private health coverage through the Illinois exchange during the open enrollment period for 2024 coverage, up from about 342,000 the year before.39 This marked the highest enrollment Illinois has ever had; the previous record high came in 2016, when about 388,000 people enrolled.40
Enrollment over time in the Illinois Marketplace is illustrated in the chart below. The increase in recent years is due in large part to the subsidy enhancements provided by the American Rescue Plan and Inflation Reduction Act. The increase for 2024 is also partially driven by the return to normal disenrollments for the Medicaid program, which was paused for three years during the pandemic. CMS reported that by March 2024, more than 99,000 Illinois residents had transitioned from Medicaid to a Marketplace plan during the “unwinding” of the pandemic-era continuous coverage rule.41
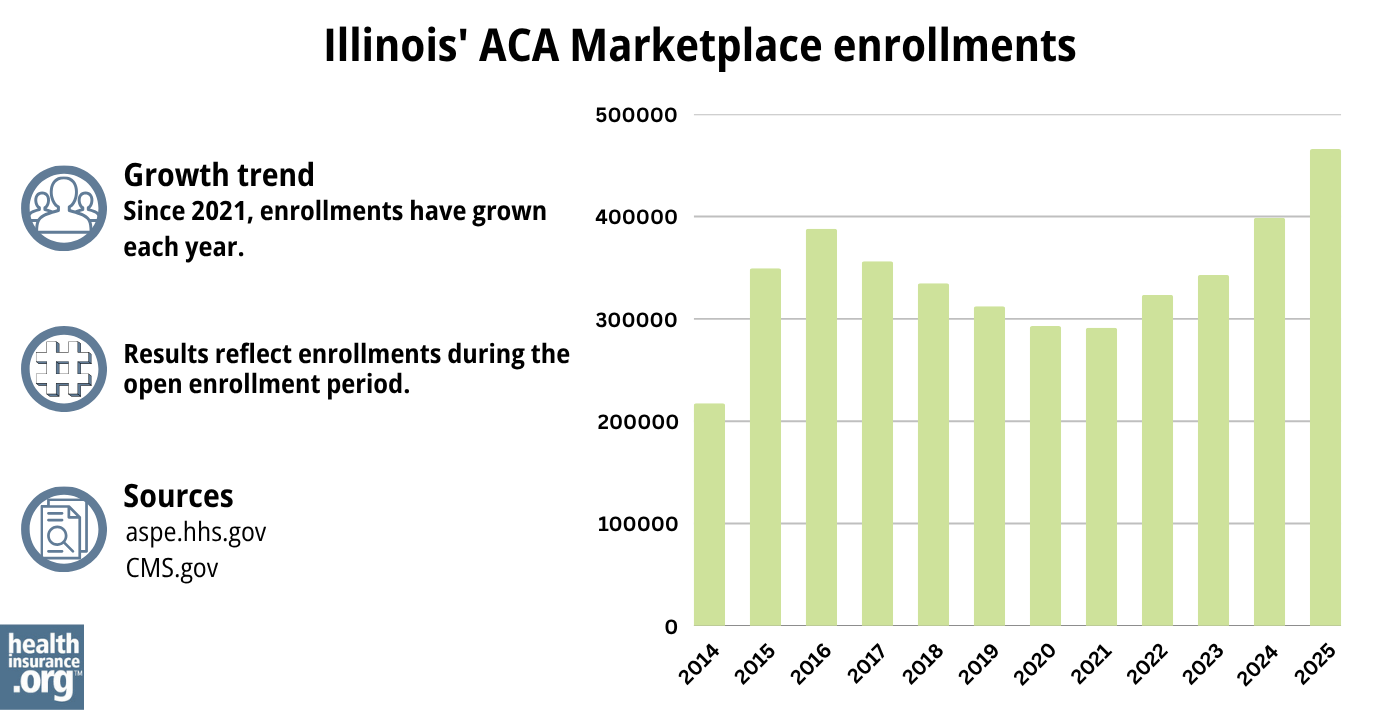
Source: 2014,42 2015,43 2016,40 2017,44 2018,45 2019,46 2020,47 2021,48 2022,49 2023,50 2024,51 202552
What health insurance resources are available to Illinois residents?
HealthCare.gov
Premium tax credits are available only through the ACA Marketplace.
Illinois Department of Insurance
The Illinois Department of Insurance regulates individual, small-group, and large-group health plans in the state (excluding self-insured ones). They also regulate brokers and agents selling private health insurance.
Illinois Senior Health Insurance Program (SHIP)
Contact them for assistance with Medicare questions.
Illinois Department of Healthcare and Family Services
Assistance with Medicaid eligibility or enrollment in Illinois and with All Kids, the state’s Children’s Health Insurance Program, and Family Care, the state’s Medicaid coverage for parents with minor children.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Illinois?
Explore more resources for options in Illinois including short-term health insurance, dental insurance, Medicaid and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”2025 OEP State-Level Public Use File (ZIP)” Centers for Medicare & Medicaid Services, Accessed May 13, 2025 ⤶ ⤶
- ”Rate Review Submissions” RateReview.HealthCare.gov. Accessed Jan. 7, 2025 ⤶
- ”Get Covered Illinois” getcovered.illinois.gov ⤶
- ”Gov. Pritzker Signs Legislation Authorizing a State-Based Marketplace for Health Insurance, Rate Review” Illinois.gov. June 27, 2023 ⤶
- ”IDOI Announces Open Enrollment for the Get Covered Illinois Health Insurance Marketplace and Releases Rates for the 2025 Plan Year” Illinois Department of Insurance. Nov. 1, 2024 ⤶ ⤶
- ”Plan Year 2025 Qualified Health Plan Choice and Premiums in HealthCare.gov Marketplaces” Centers for Medicare & Medicaid Services. Oct. 25, 2024 ⤶ ⤶
- “Are you eligible to use the Marketplace?” HealthCare.gov, 2023 ⤶
- Medicare and the Marketplace, Master FAQ. Centers for Medicare and Medicaid Services. Accessed November 2023. ⤶
- Premium Tax Credit — The Basics. Internal Revenue Service. Accessed MONTH. ⤶
- Updates to frequently asked questions about the Premium Tax Credit. Internal Revenue Service. February 2024. ⤶
- Premium Tax Credit — The Basics. Internal Revenue Service. Accessed January 12, 2024. ⤶
- “Get Covered Illinois FAQs” getcovered.illinois.gov, Accessed September 2023 ⤶
- “Special Enrollment Opportunities” HealthCare.gov, Accessed June 24, 2024 ⤶
- “Patient Protection and Affordable Care Act, HHS Notice of Benefit and Payment Parameters for 2025; Updating Section 1332 Waiver Public Notice Procedures; Medicaid; Consumer Operated and Oriented Plan (CO-OP) Program; and Basic Health Program” U.S. Department of the Treasury Department / Centers for Medicare & Medicaid Services. April 15, 2024 ⤶
- “Who doesn’t need a special enrollment period?“ healthinsurance.org, Accessed August 2023 ⤶
- ”Temporary Special Enrollment Period (SEP) for Consumers Losing Medicaid or Children’s Health Insurance Program (CHIP) Coverage Due to Unwinding of the Medicaid Continuous Enrollment Condition Operations for Plan Year 2024” CMS.gov, Mar. 28, 2024 ⤶
- “House Bill 5142” Illinois General Assembly, enacted 2022 ⤶
- ”Illinois SB3130” BillTrack50. Enacted Aug. 2, 2024. ⤶
- “Entities Approved to Use Enhanced Direct Enrollment” CMS.gov, April 28, 2023 ⤶
- “2024 Marketplace Open Enrollment Period Public Use Files” CMS.gov, March 22, 2024 ⤶
- “2025 Marketplace Open Enrollment Period Public Use Files” CMS.gov, May 2025 ⤶
- “2024 Marketplace Open Enrollment Period Public Use Files” CMS.gov, March 2024 ⤶
- ”Illinois HB2499” BillTrack50. Enacted July 10, 2024 ⤶
- 2024 Analysis of Illinois On-Exchange Plans. Illinois.gov, 2023 ⤶
- ”Affordable Care Act (ACA) – Illinois Rate Filings” Illinois Department of Insurance. Accessed July 29, 2024 ⤶ ⤶
- ”Affordable Care Act (ACA) – Illinois Rate Filings” Illinois Department of Insurance. Accessed Nov. 13, 2024 ⤶ ⤶
- ”Illinois House Bill 2296” BillTrack50. Enacted 2023 2023 ⤶
- ”Illinois HB5395” BillTrack50. Passed May 24, 2024 ⤶
- ”Obamacare rates in Illinois: Higher premiums, more options in 2015” Venteicher, Wes, et al. Chicago Tribune. November 7, 2014 ⤶
- ”UnitedHealthcare of Illinois, Inc. History” Zippia.com ⤶
- ”Avg. UNSUBSIDIZED Indy Mkt Rate Hikes: 25% (49 States + DC)” ACA Signups ⤶
- ”Illinois: RATE-HIKE-A-PALOOZA! Six More States Added At Once!” ACA Signups ⤶
- ”Illinois Department of Insurance releases ACA Exchange health care insurance rates for 2019” Illinois.gov. October 10, 2018. ⤶
- ”Illinois: *Final* Avg. 2020 #ACA Premiums: 0.3% Decrease” ACA Signups. October 30, 2019. ⤶
- ”Illinois: Preliminary Avg. 2021 #ACA Premiums: -1.8% Indy; +5.2% Sm. Group (Unweighted)” ACA Signups. October 15, 2020. ⤶
- ”*APPROVED* Avg. 2022 #ACA Rate Changeapalooza! AK, CA, GA, HI, IL, KS, LA, MA, MS, MO, NE, NH, TX, WY” ACA Signups. November 2, 2021. ⤶
- ”Illinois: Final Avg. Unsubsidized 2023 #ACA Rate Changes: +7.1% (Updated)” ACA Signups. August 5, 2022. ⤶
- So How’d I Do On My 2024 Avg. Rate Change Project? Not Bad At All! ACA Signups. December 2023. ⤶
- “2023 Marketplace Open Enrollment Period Public Use Files” CMS.gov, March 2023 ⤶
- “HEALTH INSURANCE MARKETPLACES 2016 OPEN ENROLLMENT PERIOD: FINAL ENROLLMENT REPORT” HHS.gov, 2016 ⤶ ⤶
- ”HealthCare.gov Marketplace Medicaid Unwinding Report” Centers for Medicare & Medicaid Services. Data through March 2024; Accessed July 29, 2024. ⤶
- “ASPE Issue Brief (2014)” ASPE, 2015 ⤶
- “Health Insurance Marketplaces 2015 Open Enrollment Period: March Enrollment Report”, HHS.gov, 2015 ⤶
- “2017 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2017 ⤶
- “2018 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2018 ⤶
- “2019 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2019 ⤶
- “2020 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2020 ⤶
- “2021 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2021 ⤶
- “2022 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2022 ⤶
- “Health Insurance Marketplaces 2023 Open Enrollment Report” CMS.gov, 2023 ⤶
- ”HEALTH INSURANCE MARKETPLACES 2024 OPEN ENROLLMENT REPORT” CMS.gov, 2024 ⤶
- “2025 Marketplace Open Enrollment Period Public Use Files” CMS.gov, May 2025 ⤶

