Home > Health insurance Marketplace > Massachusetts
Massachusetts Marketplace health insurance in 2025

Compare ACA plans and check subsidy savings from a third-party insurance agency.

Massachusetts health insurance Marketplace guide
This guide was created to help you better understand the health coverage options available to you and your family in Massachusetts. The options found in Massachusetts’s ACA Marketplace may be a good choice for many consumers, and we will guide you through the options below.
Massachusetts residents use a fully state-based health insurance marketplace known as Massachusetts Health Connector to obtain ACA Marketplace plans offered by several private health insurance companies. Eight insurers offer individual/family plans via MA Health Connector in 2025, and all of them will continue to do so in 2026.3
Massachusetts also
- provides state-funded subsidies, in addition to the federal subsidies that are available nationwide. State-funded subsidies in Massachusetts became available to more people as of 2024, as described below.
- has stricter medical loss ratio requirement than most states (88%,4 as opposed to the 80% federal minimum),
- caps premiums for older enrollees at no more than double the rate for a 21-year-old (as opposed to a 3:1 ratio in most states),5
- requires residents to maintain health insurance or face a tax penalty, under a rule that predates the ACA.
- Has a merged individual and small group market, which means rates and rate changes are the same in both markets6 (subsidies offset a significant portion of premiums in the individual market, but not the small group market).
Frequently asked questions about health insurance in Massachusetts
Who can buy Marketplace health insurance?
To purchase health coverage through the Massachusetts Marketplace, you must:7
- Live in Massachusetts
- Be lawfully present in the United States
- Not be incarcerated
- Not be enrolled in Medicare
Eligibility for premium subsidies and cost-sharing reductions through the Marketplace depends on your income and how it compares with the cost of the second-lowest-cost Silver plan in your area. In addition, to qualify for financial assistance with your Marketplace plan you must:
- Not have access to affordable health coverage through your employer. If your employer offers coverage but you feel it’s too expensive, you can use our Employer Health Plan Affordability Calculator to see if you might qualify for premium subsidies in the Marketplace.
- Not be eligible for Medicaid or CHIP.8
- If married, file taxes jointly with your spouse.9 (with very limited exceptions)10
- Not be able to be claimed by someone else as a tax dependent.11
It’s important to note that Massachusetts is one of the states that has its own individual mandate, and residents who don’t have health insurance are subject to a penalty when they file their state tax returns.12 The individual mandate in Massachusetts pre-dates the ACA. It was paused from 2014 through 2018, when there was a federal penalty for not having health insurance. Massachusetts revived the state-based penalty in 2019.
When can I enroll in an ACA-compliant plan in Massachusetts?
The open enrollment period for individual/family health coverage in Massachusetts runs from November 1 to January 23. This is slightly longer than in most states.13
(Starting in the fall of 2026, open enrollment will have to end by December 31, under new federal rules that were finalized in 2025.)
Outside of open enrollment, a qualifying life event is generally necessary to enroll in a plan or make coverage changes. But residents who are eligible for ConnectorCare can enroll anytime if they are newly eligible or haven’t previously enrolled.14
Massachusetts also has a “Simple Sign Up Program” that allows people to use their state tax return to gain access to health coverage.15 Several other states have similar programs (easy enrollment programs).
How do I enroll in a Massachusetts Marketplace plan?
To enroll in an ACA Marketplace plan in Massachusetts, you can:
- Visit the Health Connector to access Massachusetts’s state-based health insurance marketplace. Here you will find an online platform to shop, compare, and choose the best health plans.
- Purchase individual and family health coverage with the help of an insurance agent or broker, a Navigator or certified application counselor, or an approved enhanced direct enrollment entity.16
The Massachusetts Health Connector debuted a program for automatic enrollment in 2022. It allows applicants to check a box on the application indicating that if they are eligible for a $0 premium ConnectorCare plan but don’t select a plan themselves, the exchange will automatically enroll them in a $0 premium plan. If the applicant had coverage in the past with a carrier that offers one of the available $0 premium plans, the exchange will enroll the person with that carrier. If not, and if multiple $0 premium plans are available, the exchange will randomly assign the person to one of the available plans. But applicants in this scenario have the option to select a different plan instead of the one to which they’re automatically assigned.17
The federal government reported that 1,568 people who previously had MassHealth coverage had been automatically enrolled into a qualified health plan by the Massachusetts Health Connector between April and June 2023.18
How can I find affordable health insurance in Massachusetts?
Residents in Massachusetts use the Health Connector to enroll in Marketplace health coverage as well as to determine subsidy eligibility. Both non-standardized and standardized health plans are available through the Health Connector.19
The Affordable Care Act provides income-based advance premium tax credits (subsidies) that offset premium payments to help keep your expenses down. More than 83% of Massachusetts Health Connector enrollees saved money on 2025 premiums. The average subsidy for these enrollees was $404/month, resulting in an average after-subsidy premium of $126/month.20
In addition to federal subsidies, Massachusetts residents may also qualify for additional subsidies via the ConnectorCare program. ConnectorCare plans qualify for the federally funded ACA premium tax credits, but are also subsidized by the state, resulting in even lower premium and out-of-pocket costs for eligible residents.21
ConnectorCare was historically available to applicants with income up to 300% of the poverty level. But starting in 2024, ConnectorCare eligibility was expanded to 500% of the poverty level.22 The expansion was a two-year pilot program, initially slated to sunset at the end of 2025. But the state’s 2026 Fiscal Year budget extended the pilot program so that eligibility for ConnectorCare will continue to extend to 500% FPL in 2026.23
ConnectorCare enrollment has been steadily increasing since mid-2023, due to the post-pandemic return to normal eligibility redeterminations and disenrollments for MassHealth (Medicaid). Many people who are no longer eligible for MassHealth are now eligible for ConnectorCare instead.24 And the expansion of eligibility to 500% of the poverty level also helped to drive ConnectorCare enrollment to record-high levels for 202425 and 202526 A large majority of all 2025 Massachusetts Health Connector enrollees are in ConnectorCare.26
ConnectorCare plans are offered by the same insurers that offer other QHPs via MA Health Connector. There are seven plan variations available, access to each plan depends on the applicant’s income. The 2025 premiums range from $0/month (for those with income up to 150% FPL) to $264/month (for those with income between 400% and 500% FPL).27

Source: CMS.gov28
How many insurers offer Marketplace coverage in Massachusetts?
Are Marketplace health insurance premiums increasing in Massachusetts?
The following average rate changes have been proposed for 2026 for the merged individual and small group markets in Massachusetts, amounting to an overall average increase of 13.4%.30
Massachusetts’ ACA Marketplace Plan 2026 PROPOSED Rate Increases by Insurance Company |
|
|---|---|
| Issuer | Percent Increase |
| Mass General Brigham Health Plan | 10.5% |
| Boston Medical Center Health Plan /WellSense Health Plan | 16.2% |
| Fallon Community Health Plan | 9.9% |
| Health New England (HNE) | 10.4% |
| Tufts Health Public Plans, Inc. | 13.2% |
| Blue Cross Blue Shield of Massachusetts (BCBSMA/ HMO Blue) | 12.9% |
| Harvard Pilgrim Health Care, Inc. | 14.8% |
| UnitedHealthcare | 12.3% |
Source: Massachusetts Division of Insurance; Office of Consumer Affairs and Business Regulation30
Although the proposed average rate increase for 2025 is 13.4%, most people enrolled in individual/family coverage through MA Health Connector are subsidy-eligible and thus do not pay the full price of their coverage.20 Subsidies are designed to keep pace with the cost of the benchmark plan (second-lowest-cost Silver plan), so they will grow if the price of the benchmark plan increases. (Although federal subsidies will decrease in 2026 if the federal subsidy enhancements sunset at the end of 2025.)
Because Massachusetts has a merged individual and small-group market, each carrier’s rate changes apply to both individual and small-group plans.
For perspective, here’s a summary of how average premiums have changed in Massachusetts over time:
- 2015: 1.6% increase31
- 2016: 6.3% increase32
- 2017: 19% increase33
- 2018: 18% increase34
- 2019: 4.7% increase35
- 2020: 5.2% increase36
- 2021: 7.9% increase37
- 2022: 6.9% increase38
- 2023: 7.6% increase39
- 2024: 3.2% increase40
- 2025: 7.9% increase41
How many people are insured through Massachusetts’s Marketplace?
During the open enrollment period for 2025 coverage, 389,191 people enrolled in a health plan through the Massachusetts exchange.20
This was a record-high enrollment number (see chart below). The enrollment increase was driven by the continued enhancement of subsidies under the American Rescue Plan and Inflation Reduction Act, Massachusetts’ decision to extend ConnectorCare eligibility to 500% of the federal poverty level (up from 300% in previous years),25 and the “unwinding” of the pandemic-era federal Medicaid continuous coverage rule.
According to a CMS report, almost 89,000 Massachusetts residents transitioned from MassHealth to a Marketplace plan through Massachusetts Health Connector between April 2023 and April 2024, due to the “unwinding.”42
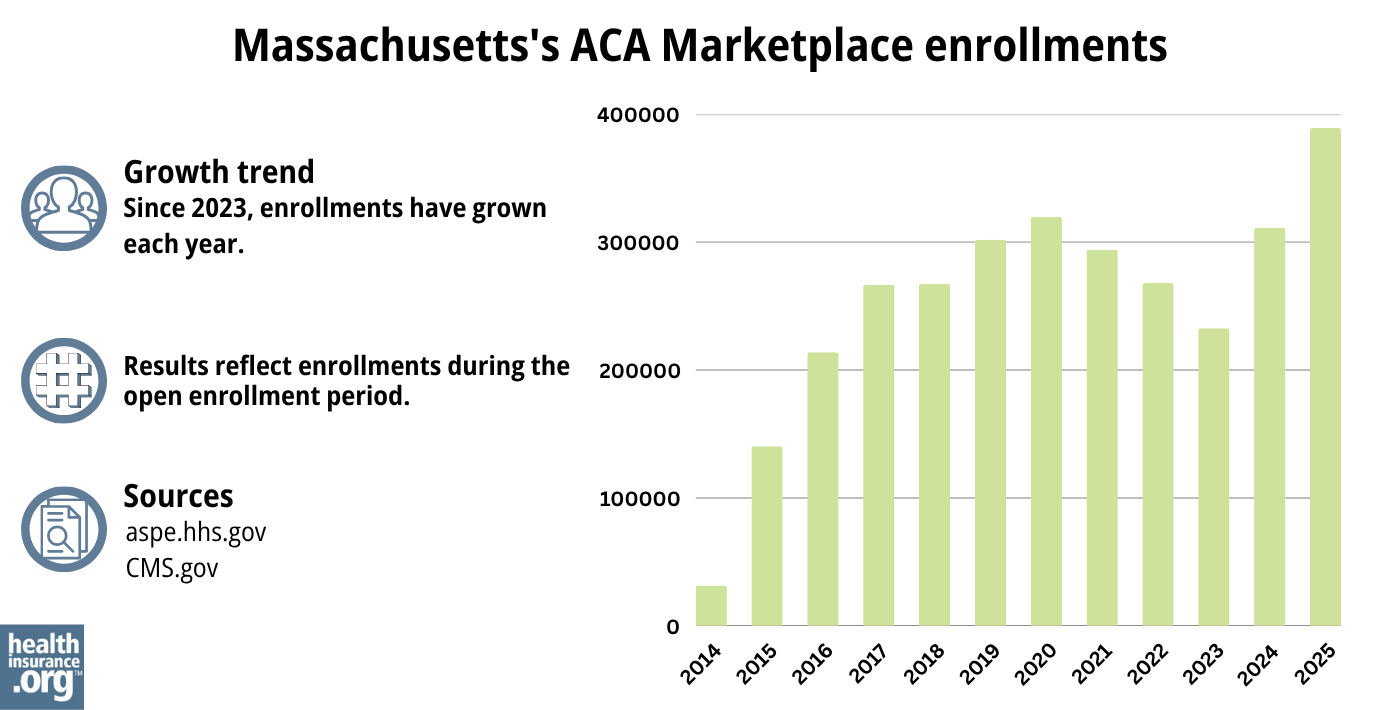
Source: 2014,43 2015,44 2016,45 2017,46 2018,47 2019,48 2020,49 2021,50 2022,51 2023,52 2024,53 202554
What health insurance resources are available to Massachusetts residents?
Massachusetts Health Connector
877-MA-ENROLL (877-623-6765)
State Exchange Profile: Massachusetts
The Henry J. Kaiser Family Foundation overview of Massachusetts’s progress toward creating a state health insurance exchange.
Health Care for All – Massachusetts Consumer Assistance Program
Assists people insured by private health plans, Medicaid, or other plans in resolving problems pertaining to their health coverage; assists uninsured residents with access to care.(800) 272-4232
Office of Patient Protection, Department of Public Health
800-436-7757 (toll-free nationwide)
Serves residents and other consumers who receive health coverage from a Massachusetts carrier, insurer, or HMO.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Massachusetts?
Explore more resources for options in Massachusetts including short-term health insurance, dental insurance, Medicaid and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”2025 OEP State-Level Public Use File (ZIP)” Centers for Medicare & Medicaid Services, Accessed May 13, 2025 ⤶ ⤶
- ”2025 Health Insurance Rates” Massachusetts Division of Insurance. Accessed Sep. 12, 2024 ⤶
- ”2026 Health Insurance Rates” Massachusetts Division of Insurance. Accessed July 11, 2025 ⤶
- “Chapter 288; An Act to Promote Cost Containment, Transparency, and Efficiency in the Provision of Quality Health Insurance for Individuals and Small Businesses” Massachusetts Legislature ⤶
- “Market Rating Reforms State Specific Rating Variations” Centers for Medicare and Medicaid Services. ⤶
- ”Report of the Merged Market Advisory Council” Massachusetts Commissioner of Insurance. Accessed June 25, 2024 ⤶
- ”A quick guide to the Health Insurance Marketplace” HealthCare.gov ⤶
- Medicare and the Marketplace, Master FAQ. Centers for Medicare and Medicaid Services. Accessed November 2023. ⤶
- Premium Tax Credit — The Basics. Internal Revenue Service. Accessed MONTH. ⤶
- Updates to frequently asked questions about the Premium Tax Credit. Internal Revenue Service. February 2024. ⤶
- Premium Tax Credit — The Basics. Internal Revenue Service. Accessed January 12, 2024. ⤶
- “Health Care Reform for Individuals” Mass.gov, 2023 ⤶
- “Request for Open Enrollment Waiver” Mass.gov, 2023 ⤶
- “ConnectorCare Health Plans” masshealthconnector.org ⤶
- Simple Sign Up Program. Massachusetts Health Connector. Accessed December 2023. ⤶
- “Entities Approved to Use Enhanced Direct Enrollment” CMS.gov, April 28, 2023 ⤶
- “Source is a discussion with the Massachusetts Health Connector Public Affairs Office” October 2023 ⤶
- “State-based Marketplace (SBM) Medicaid Unwinding Report” Medicaid.gov. September 29, 2023 ⤶
- “2024 Health and Dental Plan Proposed Seal of Approval (SOA)” Massachusetts Health Connector Board of Directors Meeting, March 2023 ⤶
- “2025 Marketplace Open Enrollment Period Public Use Files” CMS.gov, Accessed July 11, 2025 ⤶ ⤶ ⤶
- “ConnectorCare Health Plans” masshealthconnector.org, 2023 ⤶
- ”Massachusetts expands access to affordable health care” Massachusetts Health Connector. Aug. 15, 2023. ⤶
- ”Governor Healey Signs $60.9 Billion Fiscal Year 2026 Budget” Mass.gov. July 4, 2025 ⤶
- Massachusetts Health Connector Membership During MassHealth Redeterminations. Massachusetts Health Connector. December 2023. ⤶
- ”Massachusetts Health Connector ends busiest Open Enrollment in a decade with more than 72,000 new enrollments” Massachusetts Health Connector. Jan. 29, 2024 ⤶ ⤶
- ”Health Connector Board Report Metrics” Massachusetts Health Connector. Mar. 2, 2025 ⤶ ⤶
- ”ConnectorCare Health Plans: Affordable, high-quality coverage from the Health Connector” Massachusetts Health Connector. Accessed July 11, 2025 ⤶
- “2025 Marketplace Open Enrollment Period Public Use Files” CMS.gov, May 2025 ⤶
- ”2025 Health Insurance Rates” Massachusetts Division of Insurance. Accessed Sep. 12, 2024 ⤶
- ”2026 Health Insurance Rates” Massachusetts Division of Insurance. Accessed July 11, 2025 ⤶ ⤶ ⤶
- “Final Award of 2015 Seal of Approval” Massachusetts Health Connector. ⤶
- ”Massachusetts health insurance costs set to rise by 6.3 percent in 2016” Mass Live. August 30, 2015. ⤶
- ”Board of the Commonwealth Health Insurance Connector Authority Minutes” September 8, 2016 ⤶
- ”2018 Rate Hikes” ACA Signups ⤶
- ”Health Connector Rates Going Up 4.7%” The Sun. September 13, 2018. ⤶
- ”Massachusetts: *Final* Avg. Unsubsidized 2020 Premiums: 5.2% Increase” ACA Signups. October 30, 2019. ⤶
- ”Do You Live In Massachusetts? You’ll Probably Pay More For Health Insurance Next Year” WGBH. September 17, 2020. ⤶
- ”Board of the Commonwealth Health Insurance Connector Authority Minutes” September 9, 2021 ⤶
- ”Final Award of the 2023 Seal of Approval (VOTE)” Massachusetts Health Connector Board of Directors Meeting, September 2022 ⤶
- 2024 Health Insurance Rates. Office of Consumer Affairs and Business Regulation, Mass.gov, Accessed August 2023 ⤶
- ”2025 Health Insurance Rates” Massachusetts Division of Insurance. Accessed Sep. 12, 2024 ⤶
- ”State-based Marketplace (SBM) Medicaid Unwinding Report” Centers for Medicare & Medicaid Services. Data through April 2024; Accessed Aug 15, 2024. ⤶
- “ASPE Issue Brief (2014)” ASPE, 2015 ⤶
- “Health Insurance Marketplaces 2015 Open Enrollment Period: March Enrollment Report”, HHS.gov, 2015 ⤶
- “HEALTH INSURANCE MARKETPLACES 2016 OPEN ENROLLMENT PERIOD: FINAL ENROLLMENT REPORT” HHS.gov, 2016 ⤶
- “2017 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2017 ⤶
- “2018 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2018 ⤶
- “2019 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2019 ⤶
- “2020 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2020 ⤶
- “2021 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2021 ⤶
- “2022 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2022 ⤶
- “Health Insurance Marketplaces 2023 Open Enrollment Report”CMS.gov, Accessed August 2023 ⤶
- ”HEALTH INSURANCE MARKETPLACES 2024 OPEN ENROLLMENT REPORT” CMS.gov, 2024 ⤶
- “2025 Marketplace Open Enrollment Period Public Use Files” CMS.gov, May 2025 ⤶

