
Medicare in Arkansas
Original Medicare, Medicare Advantage, Part D prescription drug, and Medigap coverage in Arkansas
Key takeaways
- More than 674,000 Arkansas residents are enrolled in Medicare.1
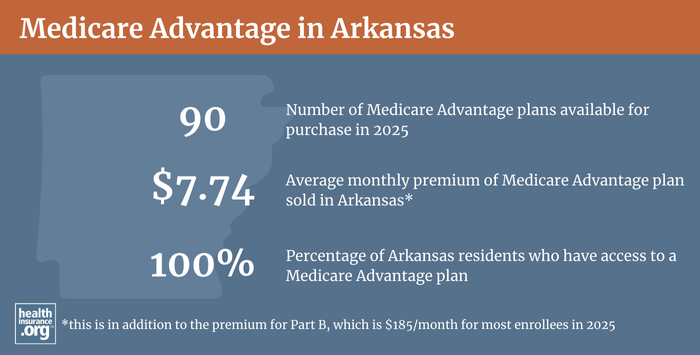
- 45% of Arkansas Medicare beneficiaries are enrolled in Medicare Advantage plans (this is lower than the national average, but steadily increasing).1
- Medicare Advantage availability depends on the county.
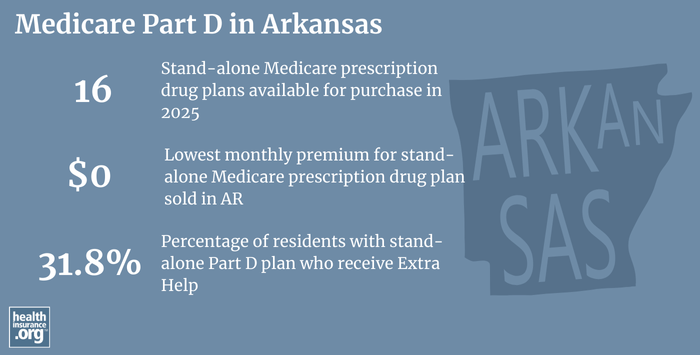
- There are 16 stand-alone Part D prescription plans available in Arkansas for 2025, with premiums that start as low as $0/month.2

Medicare enrollment in Arkansas
As of June 2024, there were 674,169 residents with Medicare in Arkansas.1 That’s 18% of the state’s population.3
Medicare enrollment happens for most Americans when they turn 65 — either automatically, if they’re already receiving Social Security or Railroad Retirement benefits, or during a seven-month enrollment window when they can complete the process of filing for Medicare benefits.
But Medicare eligibility is also triggered for younger people if they’re disabled and have been receiving disability benefits for 24 months, or if they have ALS or end-stage renal disease.
Nationwide, almost 11% of Medicare beneficiaries are under the age of 65,4 but over 16% of the people with Medicare in Arkansas are eligible due to disability rather than age.1
Learn about Medicare plan options in Arkansas by contacting a licensed agent.



Explore our other comprehensive guides to coverage in Arkansas

The ACA Marketplace allows individuals and families to shop for and enroll in ACA-compliant health insurance plans. Subsidies may be available based on household income to help lower costs.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Arkansas.


Learn about Arkansas’ Medicaid expansion, the state’s Medicaid enrollment and Medicaid eligibility.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage. Learn more about short-term plan availability in Arkansas.

Frequently asked questions about Medicare in Arkansas
What is Medicare Advantage?
Private Medicare Advantage plans are an alternative to Original Medicare, and are available in all counties in Arkansas for 2023 coverage, although the service areas vary by plan, with availability varying across the state. The number of Medicare Advantage plan options for 2023 ranges from 28 in Howard County, to 63 in Conway County.
45% of Arkansas Medicare beneficiaries have Medicare Advantage plans as of June 2024,1 versus a nationwide average of 50%.4 As of June 2024, there were 305,454 Arkansas residents with private Medicare coverage, while the other 368,715 beneficiaries had coverage under Original Medicare.1
Original Medicare includes Medicare Part A (hospital coverage) and Medicare Part B (medical/physician/outpatient coverage). The coverage is provided directly by the federal government, and enrollees have access to a nationwide network of providers. But people with Original Medicare need additional supplemental coverage (from an employer-sponsored plan, Medicaid, Medigap plans, and/or Medicare Part D plans) for things like prescription drugs and out-of-pocket costs (out-of-pocket costs are not capped under Original Medicare).
Medicare Advantage plans include all of the benefits of Medicare Parts A and B, although out-of-pocket costs will differ significantly as Advantage plans set their own copays, deductibles, and coinsurance levels, within an allowable range established by the federal government – in 2024, the maximum out-of-pocket limit for Part A and B services under Medicare Advantage plans is $8,850.5 Advantage plans usually also have additional benefits, such as integrated Part D coverage for prescription drugs, and coverage for things like dental and vision care.
But Medicare Advantage insurers establish their own provider networks, which are generally localized and more limited than the nationwide network for Original Medicare. And out-of-pocket costs for Medicare Advantage plans are often higher than they would be if a beneficiary had Original Medicare plus a Medigap plan — but the latter combination also tends to have higher monthly premiums than a Medicare Advantage plan. There are pros and cons to either alternative, and no single solution works for everyone.
Medicare Advantage enrollment is available when a person first becomes eligible for Medicare, and there are also annual windows during which beneficiaries can enroll or change their Advantage coverage. Medicare’s annual election period (October 15 to December 7 each year) allows Medicare beneficiaries the chance to switch between Medicare Advantage plans and Original Medicare (and add, drop, or switch to a different Medicare Part D prescription plan). And people who are already enrolled in Medicare Advantage plans also have the option to switch to a different Advantage plan or to Original Medicare during the Medicare Advantage open enrollment period, which runs from January 1 to March 31.
What are Medigap plans?
Original Medicare does not limit out-of-pocket healthcare costs, so most enrollees maintain some form of supplemental coverage. More than half of Original Medicare beneficiaries get their supplemental coverage through an employer-sponsored plan or Medicaid. But for those who don’t, Medigap plans (also known as Medicare supplement plans) will pay some or all of the out-of-pocket costs they would otherwise have to pay if they had only Original Medicare.
205,964 people had Medigap coverage in Arkansas as of the end of 2022.6
Medigap plans are sold by private insurers, but the plans are standardized under federal rules. There are ten different plan designs (differentiated by letters, A through N), and the benefits offered by a particular plan (Plan A, Plan F, etc.) are the same regardless of which insurer sells the plan. Pricing, however, varies from one insurer to another.
But Arkansas is one of just eight states where Medigap premiums cannot vary based on an enrollee’s age (referred to as “no age rating” in Arkansas),7 as long as the enrollee is at least 65 years old (more on this below). Medigap premiums in Arkansas can still vary based on tobacco use and medical history, with preferred premiums and standard premiums for various scenarios.
There are 58 insurance companies that offer Medigap plans in Arkansas. Medigap insurers in the state are required to maintain minimum loss ratios of at least 65% for individual policies, and at least 75% for employer group policies. This means that at least 65% (or 75% for group plans) of the premium revenue that the insurers bring in must be spent on enrollees’ healthcare claims.
Unlike other private Medicare coverage (Medicare Advantage and Medicare Part D plans), there is no annual open enrollment window for Medigap plans. Instead, federal rules provide a one-time six-month window when Medigap coverage is guaranteed issue. This window starts when a person is at least 65 and enrolled in Medicare Part B (you must be enrolled in both Part A and Part B to buy a Medigap plan).
Note that Arkansas has directed Medigap insurers to honor this enrollment window for people who were enrolled in both Medicare and Medicaid during the pandemic, and were not disenrolled from Medicaid due to the federal continuous coverage rule that was in place from March 2020 through March 2023. When their Medicaid ends, they have a six-month window to sign up for Medigap without underwriting, even if they’ve already been enrolled in Medicare more than six months.
People who aren’t yet 65 can enroll in Medicare if they’re disabled and have been receiving disability benefits for at least two years or if they have ALS or kidney failure, and about 17% of Arkansas Medicare beneficiaries are under age 65.1 Federal rules do not guarantee access to Medigap plans for people who are under 65, but the majority of the states have implemented rules to ensure that disabled Medicare beneficiaries have at least some access to Medigap plans.
Arkansas joined them in 2018, with a law that was enacted in 2017 (Act 684). The law called for the Arkansas Insurance Department to amend the state’s rules so that people under age 65 would be able to purchase Medigap coverage by 2018 (prior to that, Medigap insurers in Arkansas did not have to sell plans to people under the age of 65).
Since July 2018, Medigap insurers must offer at least one Medigap plan to Medicare beneficiaries under the age of 65.8 Insurers can pick which plan they want to offer to disabled enrollees, and nearly all of them have chosen Plan A (the least comprehensive Medigap plan), although a few insurers offer other options.9 There is no requirement that Arkansas Medigap insurers extend the “no age rating” rule to people under the age of 65, and most of the insurers charge significantly higher premiums for disabled enrollees.9
Disabled Medicare beneficiaries have another Medigap open enrollment period when they turn 65. At that point, they can switch to a plan with the lower premiums that apply to people who are aging into Medicare, rather than qualifying due to disability.
Disabled Medicare beneficiaries can choose instead to enroll in a Medicare Advantage plan if it fits their needs. Medicare Advantage plans are available to anyone who is eligible for Medicare, and the premiums are not higher for those under 65. But as noted above, Medicare Advantage plans have more limited provider networks than Original Medicare, and total out-of-pocket costs in 2024 can be as high as $8,850 per year for in-network care, plus the out-of-pocket cost of prescription drugs.
Although the Affordable Care Act eliminated pre-existing condition exclusions in most of the private health insurance market, those rules don’t apply to Medigap plans. Medigap insurers can impose a pre-existing condition waiting period of up to six months if you didn’t have at least six months of continuous coverage prior to your enrollment. And if you apply for a Medigap plan after your initial enrollment window closes (assuming you aren’t eligible for one of the limited guaranteed-issue rights), the Medigap insurer can consider your medical history in determining whether to accept your application, and at what premium.
What is Medicare Part D?
Original Medicare does not provide coverage for outpatient prescription drugs. More than half of Original Medicare beneficiaries have supplemental coverage via an employer-sponsored plan (from a current or former employer or spouse’s employer) or Medicaid, and these plans often include prescription coverage.
But Medicare beneficiaries who do not have drug coverage through Medicaid or an employer-sponsored plan need to obtain Medicare Part D in order to have coverage for prescriptions. Part D can be purchased as a stand-alone plan, or as part of a Medicare Advantage plan with integrated Part D prescription drug coverage.
There are 16 stand-alone Medicare Part D plan options for sale in Arkansas for 2025 coverage, with premiums that start as low as $0/month.2
243,789 Medicare beneficiaries in Arkansas had prescription coverage under stand-alone Medicare Part D plans as of June 2024.1 Another 289,652 had Part D prescription coverage integrated with their Medicare Advantage plans.1 In line with the trend in most states, the number of people with Part D coverage for prescription drugs in Arkansas has been increasing as overall Medicare enrollment increases. But also in line with national trends, the number of Arkansas residents with stand-alone Part D plans has been declining in Arkansas, while the number of people with Part D coverage integrated with an Advantage plan has been increasing.
Medicare Part D enrollment is available when a beneficiary is first eligible for Medicare. And the same fall enrollment window that applies to Medicare Advantage plans also applies to Medicare Part D plans. So Medicare beneficiaries can change to a different Part D plan during the window from October 15 to December 7 each year, with coverage effective January 1. People who didn’t enroll when they were first eligible can add a Part D plan during this window, although a late enrollment penalty can apply if the person didn’t have creditable drug coverage during the time they delayed their enrollment in Part D coverage.
What additional resources are available for Medicare beneficiaries and their caregivers in Arkansas?
If you have questions about Medicare eligibility in Arkansas, Medicare enrollment in Arkansas, or need general information about health coverage for seniors, you can contact the Arkansas Senior Health Insurance Information Program (SHIIP). This state-based resource is designed to provide assistance on a wide range of Medicare-related questions.
Arkansas SHIIP Quick Guide to Medicare
The Arkansas Insurance Department’s Senior Health Page includes a variety of resources and information that are useful for people with Medicare in Arkansas.
The Medicare Rights Center is a nationwide service that can provide assistance and information regarding Medicare enrollment, eligibility, and benefits.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Arkansas?
Explore more resources for options in AR including ACA coverage, short-term health insurance, dental and Medicaid.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- “Medicare Monthly Enrollment – Arkansas.” Centers for Medicare & Medicaid Services Data. Accessed October, 2024. ⤶ ⤶ ⤶ ⤶ ⤶ ⤶ ⤶ ⤶ ⤶
- ”Fact Sheet: Medicare Open Enrollment for 2025” (11) Centers for Medicare & Medicaid Services. Sep. 27, 2024 ⤶ ⤶
- “U.S. Census Bureau Quick Facts: Arkansas.” United States Census Bureau, Accessed October, 2024. ⤶
- “Medicare Monthly Enrollment – National.” Centers for Medicare & Medicaid Services Data. October, 2024. ⤶ ⤶
- ”Final Contract Year (CY) 2024” mabenefitsmailbox.lmi.org. Accessed October, 2024 ⤶
- ”The State of Medicare Supplement Coverage” AHIP. May 2024 ⤶
- ”Act 710 of the 1989 Regular Session” Arkansas Legislature. Accessed Jan, 29, 2026 ⤶
- ”054.00.17 Ark. Code R. 003 – Proposed Rule 27: Minimum Standards for Medicare Supplement Policies” (Section 25). Cornell Legal Information Institute. Accessed Jan. 29, 2026 ⤶
- ”Supplement Insurance (Medigap) plans in Arkansas” (zip code 72002) Medicare plan comparison tool. Accessed Jan. 29, 2026 ⤶ ⤶

