Medicare in Indiana

Legislation under consideration in 2024 would expand access to affordable Medigap plans for Indiana beneficiaries under age 65
Key Takeaways
- In Indiana, more than 1.3 million residents are enrolled in Medicare.1
- About 49% of Indiana Medicare beneficiaries are enrolled in Medicare Advantage plans.1
- Since 2020, Indiana has required Medigap insurers to offer at least Plan A to people under age 65, but the premiums are significantly higher than the premiums for a 65-year-old.
- About 82% of Indiana Medicare beneficiaries have Part D prescription coverage, either under a stand-alone plan or as part of their Medicare Advantage plans.1

Medicare enrollment in Indiana
As of August 2024, Medicare enrollment in Indiana stood at 1,372,886 people,1 which is nearly 18% of the state’s population.2
For most Americans, turning 65 is the path to Medicare enrollment. But younger Americans become eligible for Medicare if they have been receiving disability benefits for 24 months, or if they have ALS or end-stage renal disease. Nationwide, a little less than 11% of all Medicare beneficiaries are under age 65;3 in Indiana, about 12% of Medicare beneficiaries were under age 65 as of mid-2024.1
Read about Medicare’s open enrollment period and other important deadlines for Medicare coverage enrollment.
Indiana lawmakers passed legislation in 2024 (not yet signed into law as of February 2024) that would improve access to Medigap plans for beneficiaries under the age of 65.4This is described in more detail below, along with the state’s current rule for Medigap access when a beneficiary is younger than 65.
Learn about Medicare plan options in Indiana by contacting a licensed agent.



Explore our other comprehensive guides to coverage in Indiana

We’ve created this guide to help you understand the Indiana health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.

Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Indiana.

Learn about Indiana’s Medicaid expansion, the state’s Medicaid enrollment and Medicaid eligibility.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage. Learn more about short-term plan availability in Indiana.

Frequently asked questions about Medicare in Indiana
What is Original Medicare?
Original Medicare is a federally-run program that does not vary from one state to another. So general Medicare eligibility in Indiana and Medicare enrollment in Indiana work the same way they do in every other state. For residents who aren’t yet receiving Social Security retirement benefits and thus aren’t automatically enrolled when they turn 65, the Medicare application in Indiana is done via the Social Security Administration, as is the case throughout the United States.
Available options for private Medicare coverage, including Medicare Advantage plans, Medigap plans, and Medicare Part D plans, do vary from state to state.
What is Medicare Advantage?
Medicare Advantage is available as a private alternative to Original Medicare. Medicare Advantage includes all of the benefits of Original Medicare (hospital and outpatient/physician coverage), although the out-of-pocket healthcare costs can be very different, as Medicare Advantage plans can set their own coinsurance, copays, and deductible levels (within parameters set by CMS).
Most Medicare Advantage plans also include Part D coverage for prescription drugs, as well as extra programs like dental and vision coverage. But Medicare Advantage plans tend to have localized healthcare provider networks, as opposed to Original Medicare’s nationwide access to healthcare providers. There are pros and cons to either option.
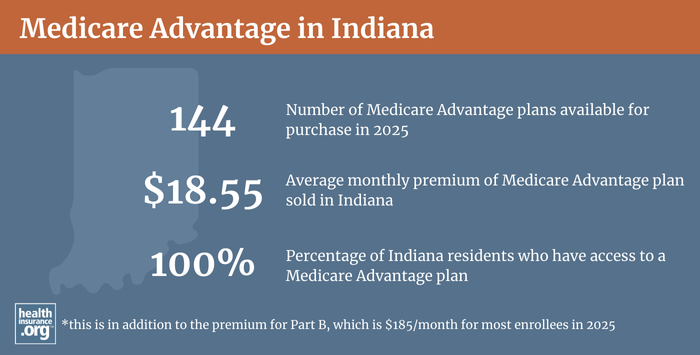
Twenty-eight percent of Medicare beneficiaries in Indiana were enrolled in Medicare Advantage plans as of 2018, compared with an average of 34% nationwide. As of August 2024, there were 678,862 Indiana Medicare beneficiaries enrolled in private Medicare plans.1
That’s in keeping with the national trend of increasing enrollment in Medicare Advantage plans over the last several years; Medicare Advantage accounted for about 50% of all Medicare beneficiaries nationwide as of August 2024.3
Medicare Advantage plan availability varies from one country to another. For 2024, Indiana residents can choose from among at least 44 Medicare Advantage plans, and up to 77 plans, depending on where they live (these numbers are a dramatic increase from 2020, when plan availability ranged from 11 to 30 plans, depending on the county).5
Medicare’s annual election period (October 15 to December 7 each year) allows Medicare beneficiaries to switch between Medicare Advantage and Original Medicare (and add or drop a Medicare Part D prescription plan). There is also a Medicare Advantage Open Enrollment Period (January 1 to March 31), during which a person who already has a Medicare Advantage plan can pick a different Advantage plan or switch to Original Medicare.
What are Medigap plans?
More than half of Original Medicare beneficiaries receive supplemental coverage through an employer-sponsored plan or Medicaid. But for those who don’t, Medigap plans (also known as Medicare supplement plans) are designed to pay some or all of the out-of-pocket costs (deductibles and coinsurance) that Medicare beneficiaries would otherwise have to pay themselves. Original Medicare does not limit out-of-pocket costs, so most enrollees use some form of supplemental coverage; Medigap plans are what’s available for people who don’t have access to an employer-sponsored plan (including retiree plans) or Medicaid.
Although Medigap plans are sold by private insurers, the plans are standardized under federal rules. There are ten different plan designs (differentiated by letters, A through N), and the benefits offered by a particular plan (Plan A, Plan F, etc.) are the same regardless of which insurer is selling the plan. So plan comparisons are much easier for Medigap policies than for other types of health insurance; consumers can base their decision on premiums and less tangible things like customer service, since the benefits themselves are uniform.
You can compare Medigap plans on Medicare.gov’s plan finder, or using Indiana’s plan comparison tool. According to an AHIP analysis, 387,689 people in the state had Medigap coverage as of 2021.
Unlike other private Medicare coverage (Medicare Advantage and Medicare Part D plans), there is no annual open enrollment window for Medigap plans. Instead, federal rules provide a one-time six-month window when Medigap coverage is guaranteed issue. This window starts when a person is at least 65 and enrolled in Medicare Part B (you must be enrolled in both Part A and Part B to buy a Medigap plan).
People who aren’t yet 65 can enroll in Medicare if they’re disabled and have been receiving disability benefits for at least two years, and about 12% of Indiana’s Medicare beneficiaries are under age 65.1 But federal rules do not guarantee access to Medigap plans for people who are under 65. However, the majority of the states have rules to ensure that disabled Medicare beneficiaries have at least some access to Medigap plans. Since mid-2020, Indiana has been among them, thanks to legislation that the state enacted in 2019 (S.B.392).
The bill passed with strong support in both chambers of Indiana’s legislature, and was signed into law in May 2019. As of July 2020, it requires Medigap insurers to offer at least one Medigap plan (Plan A) to Medicare beneficiaries who are under 65 and eligible for Medicare due to a disability. The legislation requires Medigap insurers to grant Medicare beneficiaries a six-month open enrollment period that begins when they’re enrolled in Part B (or determined eligible for retroactive Part B coverage), regardless of age. And for Indiana residents who were under 65 and already enrolled in Medicare due to a disability, a one-time six-month enrollment window ran from July through December 2020.
(Additional legislation passed in 2024 with strong support in both chambers of the Indiana legislature that, if signed into law, will require Medigap insurers to make all plans available to under-65 beneficiaries, as of 2025. It will also prohibit higher under-65 premiums for Medigap plans A, B, and D, and limit under-65 premiums for other Medigap plans to no more than 200% of the age-65 premiums.)4
Before mid-2020, Medigap insurers in Indiana were not required to offer coverage to beneficiaries under the age of 65—and none of them voluntarily chose to do so.
Indiana joined several other states that require Medigap insurers to offer at least one plan on a guaranteed-issue basis to disabled Medicare beneficiaries. But unlike some of those states, Indiana’s 2019 legislation does not limit premiums for these enrollees, so rates for people under 65 can be much higher than the rates for a person who is 65. As an example, premiums for Plan A for a 65-year-old non-smoking woman in Indianapolis range from about $0 to $322/month in 2024. But if she’s 64 instead, the premiums for the available plans range as high as $1,027/month.
(As noted above, new legislation passed in 2024 will require — if signed into law — insurers to offer Medigap plans A, B, and D to Indiana beneficiaries who are under age 65, without higher premiums. It would also require insurers to offer the other Medigap plans with premiums no higher than double the rates that apply to age-65 enrollees.4)
Medicare beneficiaries under age 65 also have the option to enroll in Medicare Advantage plans, as those plans are guaranteed issue for all Medicare beneficiaries within their service area, regardless of age.
Although the Affordable Care Act eliminated pre-existing condition exclusions in most of the private health insurance market, those regulations don’t apply to Medigap plans. Medigap insurers can impose a pre-existing condition waiting period of up to six months, if you didn’t have at least six months of continuous coverage prior to your enrollment. And if you apply for a Medigap plan after your initial enrollment window closes (assuming you aren’t eligible for one of the limited guaranteed-issue rights), the insurer can look back at your medical history in determining whether to accept your application, and at what premium.
What is Medicare Part D?
Original Medicare does not cover outpatient prescription drugs. Some Original Medicare beneficiaries have supplemental coverage via an employer-sponsored plan (from a current or former employer or spouse’s employer), and these plans often include prescription coverage. But Medicare enrollees without drug coverage through an employer-sponsored plan need to obtain Medicare Part D prescription coverage (note that people who are dually eligible for both Medicare and Medicaid also get their drug coverage through Part D, rather than the Medicaid program). Part D coverage can be purchased as a stand-alone plan, or as part of a Medicare Advantage plan that includes Part D prescription drug coverage.
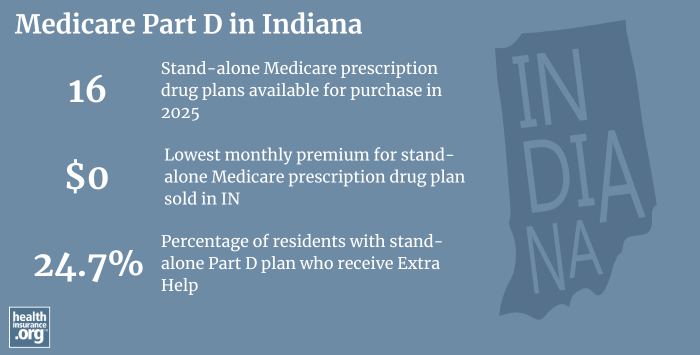
In Indiana, there are 16 stand-alone Part D plans for sale for 2025, with premiums as low as $0/month.6
As of August 2024, there were 1,150,227 Indiana Medicare beneficiaries who had Part D prescription coverage.1 About 45% had coverage under stand-alone Part D plans, while about 55% had Part D prescription coverage as part of their Medicare Advantage plans.1
Medicare Part D enrollment is available when a beneficiary first becomes eligible for Medicare. And the annual Medicare election period each fall (October 15 to December 7) allows beneficiaries the opportunity to switch to a different Medicare Part D plan or enroll for the first time if they didn’t do so when they were first eligible, although a late enrollment penalty can be assessed if they didn’t have creditable coverage before enrolling.
How does Medicaid provide financial assistance to Medicare beneficiaries in Indiana?
Many Medicare beneficiaries receive financial assistance through Medicaid with the cost of Medicare premiums, prescription drug expenses, and services Medicare doesn’t cover – such as long-term care.
Our guide to financial assistance for Medicare enrollees in Indiana includes overviews of these benefits, including Medicare Savings Programs, long-term care coverage, and eligibility guidelines for assistance.
What additional resources are available for Medicare beneficiaries and their caregivers in Indiana?
Do you have questions about Medicare eligibility or need help enrolling in Medicare in Indiana?
- The Indiana Department of Insurance (IDOI) website is good resource for eligibility, enrollment, and other general Medicare information.
- The Indiana State Health Insurance Assistance Program offers free assistance for Medicare beneficiaries. Call their central office at 1-800-452-4800 or find a local office.
- The Medicare Rights Center has a comprehensive national website and a helpful call center that can provide a variety of assistance with Medicare-related questions.
- Programs of All-Inclusive Care for the Elderly (PACE): A Medicare and Medicaid program that helps seniors receive the care they need in their homes and local communities, without having to move into a nursing home.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Indiana?
Explore more resources for options in Indiana including ACA coverage, short-term health insurance, dental insurance and Medicaid.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- “Medicare Monthly Enrollment – Indiana.” Centers for Medicare & Medicaid Services Data. Accessed December, 2024. ⤶ ⤶ ⤶ ⤶ ⤶ ⤶ ⤶ ⤶ ⤶
- U.S. Census Bureau Quick Facts: United States & Indiana.” U.S. Census Bureau, July 2023. ⤶
- “Medicare Monthly Enrollment – US” Centers for Medicare & Medicaid Services Data, December 2024. ⤶ ⤶
- Indiana Senate Bill 215. BillTrack50. Passed February 2024. ⤶ ⤶ ⤶
- ”Medicare Advantage 2024 Spotlight: First Look” KFF.org Nov. 15, 2023 ⤶
- ”Fact Sheet: Medicare Open Enrollment for 2025” (44) Centers for Medicare & Medicaid Services. Sep. 27, 2024 ⤶

