Home > Health insurance Marketplace > Nebraska
Nebraska Marketplace health insurance in 2025

Compare ACA plans and check subsidy savings from a third-party insurance agency.

Nebraska health insurance Marketplace guide
This guide, including the FAQs below, was developed to help you understand the health insurance coverage options and potential financial assistance available to you and your family in Nebraska.
Nebraska uses the federally-facilitated health insurance Marketplace (exchange), HealthCare.gov, where residents can purchase individual or family health insurance coverage. The Nebraska Marketplace provides access to health insurance products from five private insurers — including one newcomer for 20253 — all of which offer coverage statewide.4
Depending on your income and other circumstances, you may get help to lower your monthly insurance premium and possibly your out-of-pocket expenses. Most Nebraska Marketplace enrollees do qualify for financial assistance.5
Frequently asked questions about health insurance in Nebraska
Who can buy Marketplace health insurance?
To qualify for health coverage through the Nebraska Marketplace, you must:6
- Live in Nebraska
- Be lawfully present in the United States
- Not be incarcerated
- Not be enrolled in Medicare7
Eligibility for financial assistance in the form of premium subsidies and cost-sharing reductions depends on your household income.
In addition, to qualify for financial assistance with your Marketplace plan you must:8
- Not have access to an employer’s health coverage that’s deemed affordable. If your employer offers coverage but you feel it’s too expensive, you can use our Employer Health Plan Affordability Calculator to see if you might qualify for premium subsidies in the Marketplace.
- Not be eligible for Medicaid or CHIP.
- Not be eligible for premium-free Medicare Part A.9
- If married, file a joint tax return with your spouse.10
- Not be able to be claimed by someone else as a tax dependent.10
When can I enroll in an ACA-compliant plan in Nebraska?
In Nebraska the open enrollment period for individual/family health coverage runs from November 1 through January 15.11 (Due to the federal holiday on January 15, 2024, HealthCare.gov is allowing people until January 16, 2024 to enroll in coverage for 2024.)12
If you need your coverage to start on January 1, you must apply by December 15. If you apply between December 16 and January 15, your coverage will begin on February 1.8
Outside of the annual open enrollment period, you may still be able to enroll or make a plan change if you experience a qualifying life event, such as giving birth or losing other health coverage.
Here’s a guide to the special enrollment periods that will let you enroll or make a plan change outside of the annual open enrollment period.
How do I enroll in a Nebraska Marketplace plan?
To enroll in an ACA Marketplace plan in Nebraska, you can:
- Visit HealthCare.gov to compare the health plans that are available in your area, determine whether you’re eligible for financial assistance, and enroll in coverage during open enrollment or during a special enrollment period.
- Purchase individual and family health coverage with the help of an insurance agent or broker, a Navigator, or certified application counselor.
- Enroll in a Marketplace plan via an approved enhanced direct enrollment entity (EDE).13 Note that EDEs can also help you enroll in off-exchange coverage and even non-ACA-compliant coverage, so be clear about wanting a Marketplace plan, as that’s the only way you can qualify for financial assistance.
You can also call HealthCare.gov’s contact center by dialing 1-800-318-2596 (TTY: 1-855-889-4325). The call center is available 24 hours a day, seven days a week, but it’s closed on holidays.
How can I find affordable health insurance in Nebraska?
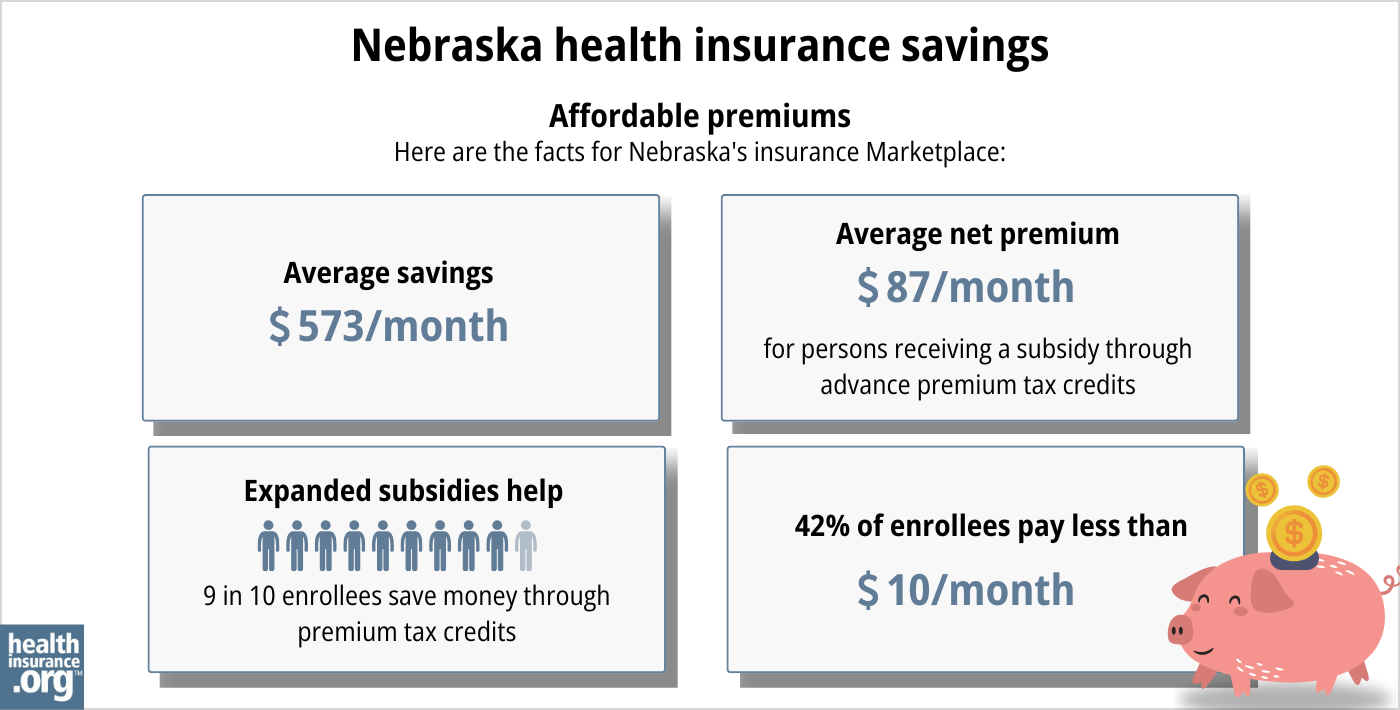
Ninety-five percent of Nebraska Marketplace enrollees saved money on 2024 premium payments amounting to an average savings of $580/month. With subsidies, enrollees paid an average of $115 per month for health coverage (that average includes the 5% of enrollees who paid full price). 14
(The numbers above are based on effectuated enrollment; the chart below shows some different metrics and is based on all applications submitted during the open enrollment period for 2024.)
The Affordable Care Act also provides income-based assistance with out-of-pocket costs, if the enrollee’s household income isn’t more than 250% of the poverty level and they select a Silver-level plan through the Marketplace.15
Between the premium subsidies and cost-sharing reductions, you may find that an ACA plan is the cheapest health insurance option for you.
Source: CMS.gov16
Nebraska expanded Medicaid under the ACA starting in late 2020. So adults (under 65) with household income up to 138% of the poverty level can qualify for Medicaid in Nebraska. Medicaid enrollment is available year-round for eligible applicants.
How many insurers offer Marketplace coverage in Nebraska?
Are Marketplace health insurance premiums increasing in Nebraska?
The following average premium changes were approved for 2025 for the health insurance companies that offer coverage in Nebraska’s individual market (calculated before any subsidies are applied):
Nebraska’s ACA Marketplace Plan 2025 APPROVED Rate Increases by Insurance Company |
|
|---|---|
| Issuer | Percent Increase |
| Blue Cross Blue Shield of Nebraska | 4.93% |
| Medica | 8.96% |
| Ambetter from Nebraska Total Care | 4.23% |
| Oscar Health | -2.14% |
| UnitedHealthcare | new for 2025 |
Source: RateReview.HealthCare.gov17
For perspective, here’s a summary of how average full-price (pre-subsidy) premiums have changed over time in Nebraska’s individual/family health insurance market:
- 2015: Average increase of 10%18
- 2016: Average increase of 16.2%19
- 2017: Average increase of 34.8%20
- 2018: Average increase of 31%21 (only one insurer remained at this point)
- 2019: Average increase of 2.2%22
- 2020: Average decrease of 6.9%23 (a second insurer joined)
- 2021: Average decrease of 2.6%24
- 2022: Average increase of 8.6%25 (two more insurers joined)
- 2023: Average increase of 0.4%26 (still four insurers, but with one exit and one new entrant)
- 2024: Average increase of 4.7%27
How many people are insured through Nebraska’s Marketplace?
In Nebraska, 117,882 people enrolled in health plans through the state’s ACA Marketplace exchange during the open enrollment period for 2024 coverage.28
The state has seen a significant increase in enrollment since 2021 (see chart below), driven in part by the American Rescue Plan (ARP) making ACA’s premium subsidies more substantial. Under the ARP – now extended through 2025 by the Inflation Reduction Act – subsidies are larger and more widely available than they used to be.29
The record-high enrollment in 2024 was also partially due to the “unwinding” of the pandemic-era Medicaid continuous coverage rule. Medicaid disenrollments resumed in 2023 after a three-year pause. CMS reported that by April 2024, nearly 24,000 people had transitioned from Nebraska Medicaid to a Marketplace plan.30
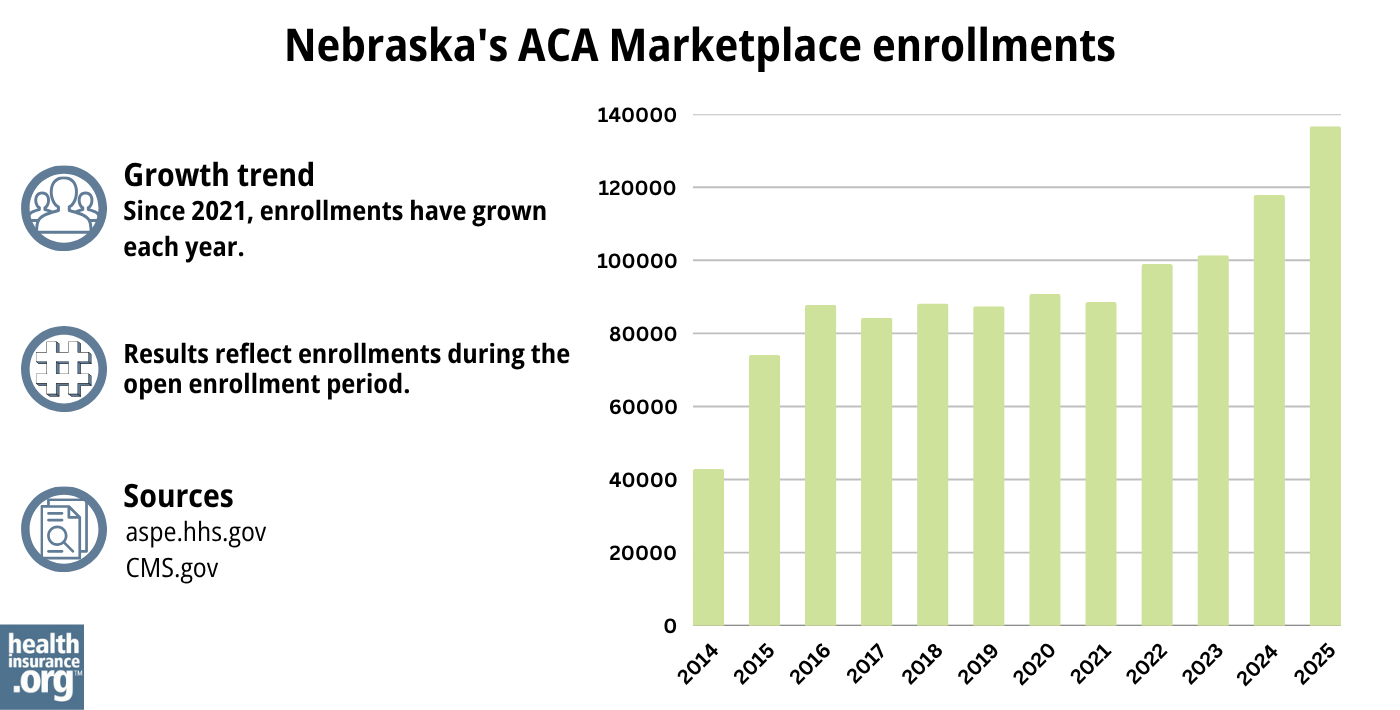
Source: 2014,31 2015,32 2016,33 2017,34 2018,35 2019,36 2020,37 2021,38 2022,39 2023,29 2024,40 202541
What health insurance resources are available to Nebraska residents?
HealthCare.gov
The federal government operates the exchange in Nebraska.
State Exchange Profile: Nebraska
The Henry J. Kaiser Family Foundation overview of Nebraska’s progress toward creating a state health insurance exchange.
Nebraska Department of Insurance
Assists consumers who have purchased insurance on the individual market or who have insurance through an employer who only does business in Nebraska.
(877) 564-7323 / Toll Free: (800) 833-7352
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Nebraska?
Explore more resources for options in Nebraska including short-term health insurance, dental insurance, Medicaid and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”2025 OEP State-Level Public Use File (ZIP)” Centers for Medicare & Medicaid Services, Accessed May 13, 2025 ⤶ ⤶
- ”Rate Review Submissions” RateReview.HealthCare.gov. Accessed Jan. 7, 2025 ⤶
- ”New 2025 Individual Exchange plans and prior authorization information” UnitedHealthcare. Oct. 1, 2024 ⤶ ⤶
- Plan Year 2025 Qualified Health Plan Choice and Premiums in HealthCare.gov Marketplaces. Centers for Medicare and Medicaid Services. October 25, 2024. ⤶ ⤶
- Effectuated Enrollment: Early 2023 Snapshot and Full Year 2022 Average. Centers for Medicare and Medicaid Services. Published 2023. ⤶
- ”A quick guide to the Health Insurance Marketplace” HealthCare.gov, Accessed September 2023 ⤶
- Medicare and the Marketplace, Master FAQ. Centers for Medicare and Medicaid Services. Accessed November 2023. ⤶
- “A quick guide to the Health Insurance Marketplace®” HealthCare.gov, Accessed August, 2023 ⤶ ⤶
- Medicare and the Marketplace, Master FAQ. Centers for Medicare and Medicaid Services. Accessed November 2023. ⤶
- Premium Tax Credit — The Basics. Internal Revenue Service. Accessed May 10, 2024 ⤶ ⤶
- “When can you get health insurance?” HealthCare.gov, 2023 ⤶
- Biden-Harris Administration Launches Window-Shopping Ahead of 11th ACA Marketplace Open Enrollment Period. Centers for Medicare and Medicaid Services. October 2023. ⤶
- “Entities Approved to Use Enhanced Direct Enrollment” CMS.gov, April 28, 2023 ⤶
- ”Effectuated Enrollment: Early 2024 Snapshot and Full Year 2023 Average” CMS.gov, July 2, 2024 ⤶
- APTC and CSR Basics. Centers for Medicare and Medicaid Services. June 2023. ⤶
- “2025 Marketplace Open Enrollment Period Public Use Files” CMS.gov, May 2025 ⤶
- ”Nebraska Rate Review Submissions” RateReview.HealthCare.gov. Accessed Nov. 6, 2024 ⤶
- Analysis Finds No Nationwide Increase in Health Insurance Marketplace Premiums. The Commonwealth Fund. December 2014. ⤶
- FINAL PROJECTION: 2016 Weighted Avg. Rate Increases: 12-13% Nationally* ACA Signups. October 2015. ⤶
- Nebraska: *Approved* 2017 Avg. Rate Hikes: 35% (Oh, And Aetna Is JOINING The Exchange??) ACA Signups. September 2016. ⤶
- 2018 Rate Hikes. ACA Signups. October 2017. ⤶
- 2019 Rate Hikes. ACA Signups. October 2018. ⤶
- 2020 Rate Changes. ACA Signups. October 2019. ⤶
- Both Bright and Medica decreased average rates by 2.6% for 2021. Data are in SERFF, under filing numbers BRHP-132268892 and MEDI-132402244. ⤶
- 2022 Rate Changes. ACA Signups. October 2021. ⤶
- UPDATED: FINAL Unsubsidized 2023 Premiums: +6.2% Across All 50 States +DC. ACA Signups. Accessed November 2023. ⤶
- So How’d I Do On My 2024 Avg. Rate Change Project? Not Bad At All! ACA Signups. December 2023. ⤶
- ”Health Insurance Marketplaces 2024 Open Enrollment Period Report” CMS.gov. March 22, 2024 ⤶
- “Health Insurance Marketplaces 2023 Open Enrollment Report” CMS.gov, Accessed August 2023 ⤶ ⤶
- ”HealthCare.gov Marketplace Medicaid Unwinding Report” Centers for Medicare & Medicaid Services. Data through April 2024; Accessed Aug. 14, 2024 ⤶
- “ASPE Issue Brief (2014)” ASPE, 2015 ⤶
- “Health Insurance Marketplaces 2015 Open Enrollment Period: March Enrollment Report”, HHS.gov, 2015 ⤶
- “HEALTH INSURANCE MARKETPLACES 2016 OPEN ENROLLMENT PERIOD: FINAL ENROLLMENT REPORT” HHS.gov, 2016 ⤶
- “2017 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2017 ⤶
- “2018 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2018 ⤶
- “2019 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2019 ⤶
- “2020 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2020 ⤶
- “2021 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2021 ⤶
- “2022 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2022 ⤶
- ”HEALTH INSURANCE MARKETPLACES 2024 OPEN ENROLLMENT REPORT” CMS.gov, 2024 ⤶
- “2025 Marketplace Open Enrollment Period Public Use Files” CMS.gov, May 2025 ⤶

