Home > Health insurance Marketplace > Oregon
Oregon Marketplace health insurance in 2025

Compare ACA plans and check subsidy savings from a third-party insurance agency.

Oregon health insurance Marketplace guide
This guide, including the FAQs below, is designed to help you understand the health coverage options and possible financial assistance available to you and your family in Oregon. Many people find that an ACA Marketplace (exchange) plan, often called Obamacare, is a cost-effective choice. Six private insurers are offering health plans through the Oregon Marketplace for 2025 coverage.3
Starting in July 2024, Oregon started operating a Basic Health Program — OHP Bridge — becoming just the third state in the country to do so. Coverage under this program is available to adults under age 65 whose household income is between 138% and 200% of the federal poverty level.4
Oregon operates a state-based health insurance Marketplace but uses the HealthCare.gov enrollment platform (ie, an SBE-FP). That will change as of the fall of 2026, however, when Oregon will start running its own Marketplace platform, under the terms of legislation (SB972) the state enacted in 2023.5
(Oregon had a fully state-based exchange in 2014 but the website didn’t work well and the state opted to switch to an SBE-FP starting in the fall of 2014.6 The state plans to transition back to an SBE in the fall of 2026.)
For now, you can visit OregonHealthCare.gov to gather information about health insurance plans, eligibility, and more.7 When you’re ready to apply and enroll, you’ll be directed to HealthCare.gov to complete the enrollment. Enrollment in OHP Bridge is done via one.Oregon.gov.
Frequently asked questions about health insurance in Oregon
Who can buy Marketplace health insurance?
You can buy a health plan through the Oregon exchange if:8
- You reside in Oregon.
- You are a U.S. citizen or national.
- You are not incarcerated.
- You are not already enrolled in Medicare.
To qualify for financial assistance (premium subsidies and cost-sharing reductions), you must meet additional requirements:
- Your eligibility for premium subsidies depends on your income and how it compares with the cost of the second-lowest-cost Silver plan in your area. The cost of that Silver plan varies based on your age and location.
- You must not have access to affordable health coverage offered by an employer. If your employer offers health insurance, but you feel it’s too expensive, you can use our Employer Health Plan Affordability Calculator to see if you might qualify for premium subsidies in the Marketplace.
- You must not be eligible for Medicaid or CHIP.
- You must not be eligible for premium-free Medicare Part A.9
- No one else can be able to claim you as a tax dependent.10
- If you’re married, you must file a joint tax return with your spouse.11 (with very limited exceptions)12
When can I enroll in an ACA-compliant plan in Oregon?
In Oregon, open enrollment for ACA Marketplace/exchange individual and family health coverage runs from November 1 through January 15.
OHP Bridge enrollment and Medicaid enrollment are both open year-round.
Enrolling in an exchange plan or changing your coverage outside of the open enrollment period is possible if you meet the criteria for a Special Enrollment Period (SEP).13 This typically means you must have a qualifying life event, such as losing your health insurance, getting married, or having a baby, although some SEPs aren’t dependent on a specific qualifying life event. For example:
- Your income falls at or below 150% of the poverty level, and you’re eligible for premium tax credits. In this scenario, you can enroll anytime. However, Oregon will no longer be using the HealthCare.gov enrollment platform after 2026. This means the state will have some flexibility to set its own SEP rules,14 and will be able to decide whether to continue to offer this SEP.
- Native Americans can enroll or switch plans year-round (this SEP is available nationwide, regardless of whether a state uses HealthCare.gov or runs its own exchange platform).
For people who lose Oregon Health Plan (Medicaid or CHIP) coverage between March 31, 2023, and November 30, 2024, there’s an extended SEP available for enrollment.15
Oregon also received federal approval to not disenroll people from Medicaid if their income wasn’t more than 200% of the poverty level (the normal limit is 138%), while the state waited to implement a Basic Health Program (OHP Bridge) that became operational as of July 2024.16 So some people were able to remain on Medicaid in Oregon during the “unwinding” process even though they would have been disenrolled in most other states. And as of July 2024, these individuals transitioned to OHP Bridge coverage.
How do I enroll in a Marketplace plan in Oregon?
Here are the main ways to enroll in a Marketplace health plan in Oregon:
- Online: You can visit OregonHealthCare.gov to learn more about health insurance plans and eligibility.17 When it’s time to apply and enroll, you’ll be redirected to the federal Marketplace website, HealthCare.gov. (Oregon’s new state-based Marketplace platform is expected to debut in the fall of 2026.)
- By Phone: Dial 1-800-318-2596 (TTY: 1-855-889-4325) to enroll with a Marketplace representative. The call center is available 24 hours a day, seven days a week, but it’s closed on holidays.
- In-person: Enrollment assistance is also available from trained Navigators and assisters who can answer your questions. Go to localhelp.HealthCare.gov or OregonHealthCare.gov/GetHelp to find local help in your area.18
Assistance is available from local Navigators and brokers. Enrollments can also be completed via an approved enhanced direct enrollment (EDE) entity, using the EDE’s website.19
How can I find affordable health insurance in Oregon?
Oregon’s ACA Marketplace (HealthCare.gov) is a one-stop shop where individuals and families can find affordable health insurance coverage in Oregon. There are two types of financial assistance available through the Marketplace:
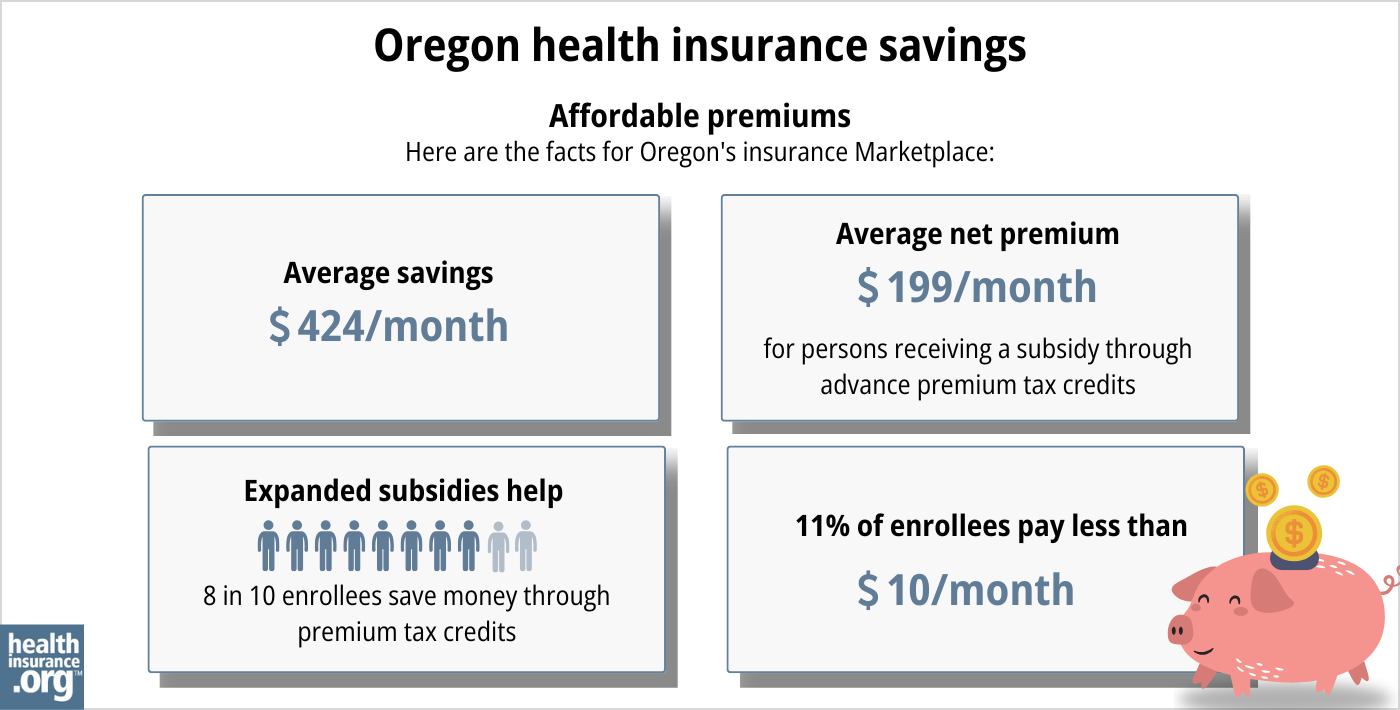
- Premium subsidies: You may qualify for income-based subsidies known as Advance Premium Tax Credits (APTC) that help lower your monthly premiums through the ACA Marketplace. About eight out of 10 Oregon exchange enrollees qualified for premium subsidies in 2024, saving around $524 monthly. People who receive these subsidies pay an average monthly premium of $164 in 20243.20
Source: CMS.gov21
- Cost-sharing reductions: You may be eligible for cost-sharing reductions (CSR) if your income is no more than 250% of the federal poverty level,22 and you enroll in a Silver-level plan through the Oregon Marketplace. CSRs help lower your out-of-pocket costs, making coverage more affordable.23
Oregon implemented a reinsurance program starting in 2018, using a 1332 waiver that allows the state to capture federal savings generated by the program.24 Reinsurance is designed to keep unsubsidized (full-price) premiums lower than they would otherwise be. Although most enrollees do qualify for premium subsidies, the reinsurance program helps to minimize premiums for those who don’t.
Oregon also requires all state-regulated health plans, including Marketplace plans, to cover both female and male contraception (including vasectomies), as well as abortion, all without out-of-pocket costs.25
Medicaid: Oregon residents may qualify for Medicaid coverage if eligible based on income. Medicaid in Oregon is called Oregon Health Plan, and has no monthly premiums.26
Basic Health Program: Oregon has created a Basic Health Program — OHP Bridge —that became operational in July 2024.4 Federal approval for OHP Bridge was granted in June 2024.27
Coverage under OHP Bridge is available to Oregon adults (under age 65) with income above 138% of the poverty level but not above 200% of the poverty level.16 (Children at this income level were already eligible for OHP coverage, so OHP Bridge does not need to cover children.)
Short-term health insurance: If you’re not eligible for subsidies, Medicare, or Medicaid, short-term health insurance, available in Oregon with terms of up to three months, might be an affordable temporary solution.
How many insurers offer Marketplace coverage in Oregon?
Are Marketplace health insurance premiums increasing in Oregon?
The following average rate changes have been approved for 2025 for Oregon’s individual/family market health insurers, amounting to an overall average proposed rate increase of 8.3%. The overall average increase was slightly lower than insurers had initially proposed.3
Oregon’s ACA Marketplace Plan 2025 APPROVED Average Rate Increases by Insurance Company |
|
|---|---|
| Issuer | Percent Increase |
| BridgeSpan Health Company | 9% |
| Kaiser Foundation Healthplan of the NW | 5% |
| Moda Health Plan, Inc. | 8.1% |
| PacificSource Health Plans | 11.1% |
| Providence Health Plan | 9.5% |
| Regence BlueCross BlueShield of Oregon | 8.1% |
Source: Oregon Division of Financial Regulation3
Average approved rate changes apply to full-price premiums. However, about 81% of Oregonians who enrolled in ACA plans received subsidies in 2024 – which means they did not pay the full rate.30
In addition, subsidy amounts are adjusted each year based on the cost of the second-lowest-priced Silver plan. So, as coverage costs increase, subsidies may also grow to offset part of the change.
If your plan’s rates are increasing next year, consider exploring other options on the ACA Marketplace. You may find a more affordable plan that still meets your coverage needs.
For perspective, here’s a summary of how average full-price (unsubsidized) premiums have changed in Oregon’s individual market over the years:
- 2015: Average decrease of 5%.31
- 2016: Average increase of 24.2%.32
- 2017: Average increase of 26.5%.33
- 2018: Average increase of 15.7%.34 (reinsurance took effect;24 Federal CSR funding eliminated35)
- 2019: Average increase of 7.3%36
- 2020: Average increase of 1.5%.37
- 2021: Average increase of 2.1%.38
- 2022: Average increase of 1.5%.39
- 2023: Average increase of 6.7%.40
- 2024: Average increase of 6.2%.41
How many people are insured through Oregon’s Marketplace?
During the 2024 open enrollment period, 145,509 people signed up for individual/family health coverage through the Oregon Marketplace/exchange.20
Although nationwide Marketplace enrollment has grown to significant record highs in recent years, Oregon’s enrollment has hovered around the same level for many years.
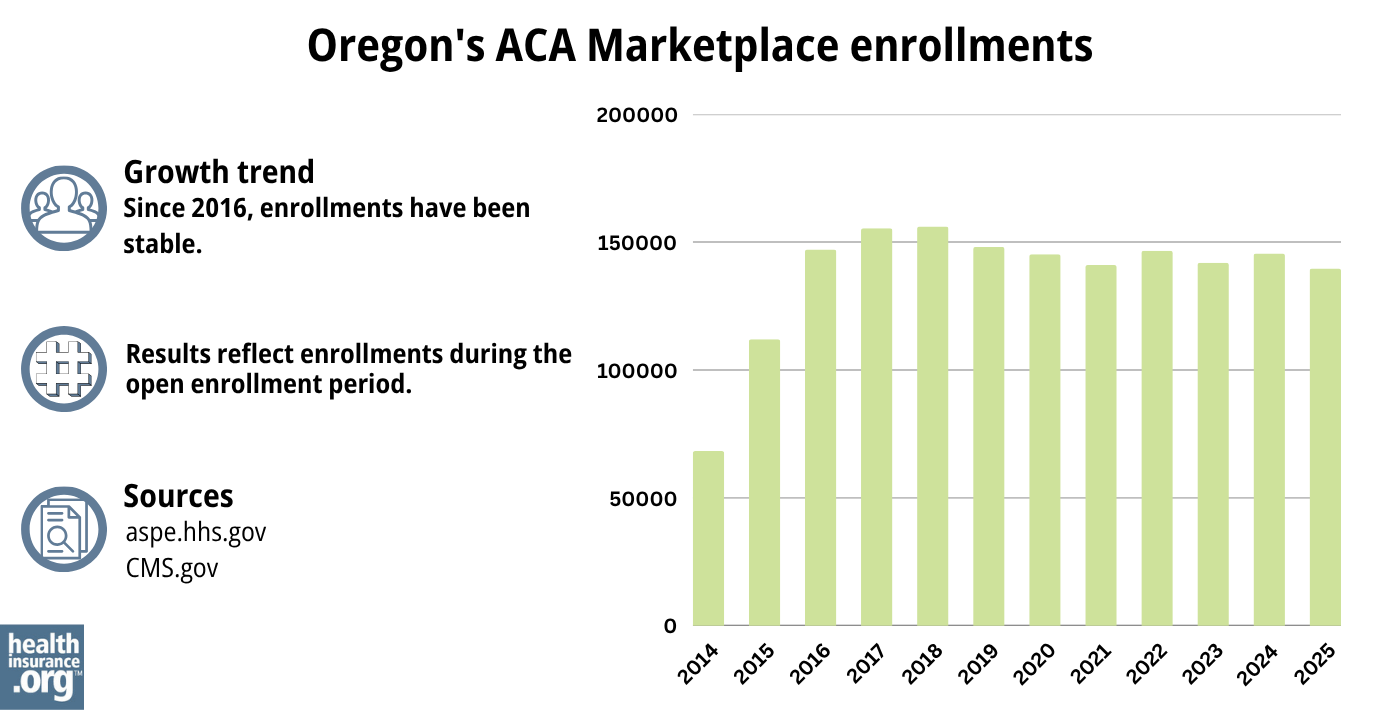
Source: 2014,42 2015,43 2016,44 2017,45 2018,46 2019,47 2020,48 2021,49 2022,50 2023,51 2024,52 202553
What health insurance resources are available to Oregon residents?
OregonHealthCare.gov
A state-run service that connects Oregon residents with health coverage options.
HealthCare.gov
The Marketplace for individuals and families buying their own health coverage; premium subsidies and cost-sharing reductions are available for eligible enrollees who use the Marketplace.
Oregon Division of Financial Regulation
Licenses and regulates health insurance companies in Oregon, as well as agents and brokers. Can address consumer questions and complaints about regulated entities.
Medicare Rights Center
A nationwide resource that can answer questions about Medicare and provide information that beneficiaries need.
Oregon Senior Health Insurance Benefits Assistance
A local service that can provide assistance, information, and enrollment counseling to Medicare beneficiaries and their caregivers.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Oregon?
Explore more resources for options in Oregon including short-term health insurance, dental insurance, Medicaid and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”2025 OEP State-Level Public Use File (ZIP)” Centers for Medicare & Medicaid Services, Accessed May 13, 2025 ⤶ ⤶
- ”Rate Review Submissions” RateReview.HealthCare.gov. Accessed Jan. 7, 2025 ⤶
- ”Oregon Division of Financial Regulation issues final health rates for 2025; five insurance companies now statewide in individual market” Oregon Division of Financial Regulation. Sep. 5, 2024 ⤶ ⤶ ⤶ ⤶
- ”Oregon Health Plan (OHP) Bridge” and ”Oregon Health Plan (OHP) Bridge — Frequently Asked Questions” Oregon Health Authority. Accessed July 11, 2024 ⤶ ⤶
- Oregon Senate Bill 972. BillTrack50. Enacted August 2023. ⤶
- Oregon decides to ditch its online health exchange for federal site. PBS News Hour. April 2014. ⤶
- “Explore your coverage and savings options” OregonHealthCare.gov, Accessed September 2023 ⤶
- “Are you eligible to use the Marketplace?” HealthCare.gov, 2023 ⤶
- Medicare and the Marketplace, Master FAQ. Centers for Medicare and Medicaid Services. Accessed November 2023. ⤶
- Premium Tax Credit — The Basics. Internal Revenue Service. Accessed January 12, 2024. ⤶
- Premium Tax Credit — The Basics. Internal Revenue Service. Accessed MONTH. ⤶
- Updates to frequently asked questions about the Premium Tax Credit. Internal Revenue Service. February 2024. ⤶
- “Enroll in or change 2023 plans – only with a Special Enrollment Period” HealthCare.gov, 2023 ⤶
- A state-based health insurance exchange in Oregon would protect access to coverage. Korbulic, Heather. Oregon Capital Chronicle. October 2023. ⤶
- ”Temporary Special Enrollment Period (SEP) for Consumers Losing Medicaid or Children’s Health Insurance Program (CHIP) Coverage Due to Unwinding of the Medicaid Continuous Enrollment Condition Operations for Plan Year 2024”Centers for Medicare & Medicaid Services. March 28, 2024 ⤶
- ”Oregon Health Plan (OHP) Bridge — Frequently Asked Questions” Oregon Health Authority. May 3, 2024 ⤶ ⤶
- “Explore your coverage and savings options” OregonHealthCare.gov, Accessed September 2023 ⤶
- “Find Local Help” OregonHealthCare.gov, Accessed September 2023 ⤶
- “Entities Approved to Use Enhanced Direct Enrollment” CMS.gov, April 28, 2023 ⤶
- “2024 Marketplace Open Enrollment Period Public Use Files” CMS.gov, March 22, 2024 ⤶ ⤶
- “2025 Marketplace Open Enrollment Period Public Use Files” CMS.gov, May 2025 ⤶
- “Federal Poverty Level (FPL)” HealthCare.gov, 2023 ⤶
- APTC and CSR Basics. Centers for Medicare and Medicaid Services. June 2023. ⤶
- Section 1332: State Innovation Waivers-Oregon. Centers for Medicare and Medicaid Services. Accessed November 2023. ⤶ ⤶
- Reproductive Health Equity Act FAQs. Planned Parenthood. Accessed November 2023. ⤶
- Oregon Health Plan. Oregon Health Authority. Accessed November 2023. ⤶
- ”Approval letter for Oregon’s Basic Health Program (BHP) Blueprint” U.S. Department of Health & Human Services. June 7, 2024 ⤶
- ACA-Compliant Plans 2024 Health Insurance Rate Requests Oregon.gov, 2023. ⤶
- Oregon finalizes 2024 health rates for individual, small group markets; sees robust options in all counties. Oregon.gov, September 2023. ⤶
- ”Effectuated Enrollment: Early 2024 Snapshot and Full Year 2023 Average” CMS.gov, July 2, 2024 ⤶
- Analysis Finds No Nationwide Increase in Health Insurance Marketplace Premiums. The Commonwealth Fund. December 2014. ⤶
- Oregon: Final 2016 Rate Hikes Approved…24.2% Weighted Average Increase, But… ACA Signups. July 2015. ⤶
- Avg. UNSUBSIDIZED Indy Mkt Rate Hikes: 25% (49 States + DC). ACA Signups. October 2016. ⤶
- 2018 Rate Hikes. ACA Signups. October 2017. ⤶
- State announcement regarding Trump administration discontinuation of cost-sharing reduction payments. Oregon.gov. October 2017. ⤶
- 2019 Rate Hikes. ACA Signups. October 2018. ⤶
- Final health insurance rate decisions lower 2020 premiums by $44 million. Oregon.gov. July 2019. ⤶
- Oregon: Final Avg. 2021 ACA Rate Change: +2.1%; +3.7% For Sm. Group. ACA Signups. October 2020. ⤶
- ACA-Compliant Plans 2022 Health Insurance Rate Requests. Oregon Department of Financial Regulation. September 2021. ⤶
- ACA-Compliant Plans 2023 Health Insurance Rate Requests. Oregon Department of Financial Regulation. September 2022. ⤶
- Oregon finalizes 2024 health rates for individual, small group markets; sees robust options in all counties. Oregon.gov, September 2023. ⤶
- “ASPE Issue Brief (2014)” ASPE, 2015 ⤶
- “Health Insurance Marketplaces 2015 Open Enrollment Period: March Enrollment Report”, HHS.gov, 2015 ⤶
- “HEALTH INSURANCE MARKETPLACES 2016 OPEN ENROLLMENT PERIOD: FINAL ENROLLMENT REPORT” HHS.gov, 2016 ⤶
- “2017 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2017 ⤶
- “2018 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2018 ⤶
- “2019 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2019 ⤶
- “2020 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2020 ⤶
- “2021 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2021 ⤶
- “2022 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2022 ⤶
- “Health Insurance Marketplaces 2023 Open Enrollment Report” CMS.gov, 2023 ⤶
- ”HEALTH INSURANCE MARKETPLACES 2024 OPEN ENROLLMENT REPORT” CMS.gov, 2024 ⤶
- “2025 Marketplace Open Enrollment Period Public Use Files” CMS.gov, May 2025 ⤶

