Medicaid eligibility and enrollment in Connecticut

Connecticut was the first to accept ACA Medicaid expansion; Undocumented children up to age 12 can enroll in Connecticut Medicaid

Connecticut Medicaid structure
Connecticut’s Medicaid program is called HUSKY Health, and it is broken into several categories (enrollment and cost data based on a report published in 2021).
- HUSKY A covers low-income children, parents and other caregivers, and pregnant women (57% of enrollees; 29% of total costs).
- HUSKY B covers children with incomes too high for HUSKY A. HUSKY B is also called the Children’s Health Insurance Program, or CHIP.
- HUSKY C covers individuals who are aged, blind or disabled and who qualify based on income and asset levels, and MED-Connect is Medicaid for employees with disabilities (10% of enrollees; 38% of total costs). These are the non-MAGI populations, as eligibility includes both income and asset tests, rather than income alone.
- HUSKY D covers low-income adults who don’t have children (33% enrollees; 33% of total costs). This is the Medicaid expansion population; Connecticut implemented the ACA’s expansion of Medicaid starting in 2014.
In 2015, Arielle Levin Becker of the Connecticut Mirror published an excellent description of how the four parts of HUSKY work, who was enrolled, and how much the programs cost. The Connecticut Department of Social Services updated the data for 2020 in this report, which includes details about the impact of the COVID pandemic.
Who is eligible for Medicaid in Connecticut?
Depending on the reason for eligibility, Connecticut residents can qualify for Medicaid (HUSKY) based on income alone (MAGI), or a combination of income and assets (non-MAGI). For children, pregnant women, parents of minor children, and childless adults up to age 64, eligibility is based on income, with income limits that vary for each group. For the aged, blind, and disabled, eligibility rules are stricter, with both income limits and asset limits.
For the groups that qualify based on income alone, eligibility is determined as a percentage of the federal poverty level (FPL). You can see the FPL numbers here (new numbers are published each year by mid-late January, and are being used for Medicaid eligibility starting March 1).
For Connecticut Medicaid, the following income limits apply, although note that there’s a 5% income disregard added, making the effective income caps higher by 5 percentage points; that has been added in the percentage of income listed below for each category of coverage (see this chart for what each eligibility level amounts to in terms of dollars in 2024):
HUSKY A
- 201% of FPL for children, ages 0-18 (undocumented children age 12 or younger can enroll, and can stay enrolled until they turn 19. Legislation was introduced in 2023 that would have extended coverage to undocumented youth up to age 20 as of January 2024, and to age 25 by mid-2024, but it did not advance.)
- 263% of FPL for pregnant women (coverage for the mother continues for 12 months after the baby is born)
- 160% of FPL for parents of dependent children (more details below about how this program has evolved over time)
- Connecticut also has a state subsidy program that ensures free coverage and medical care to adults who aren’t eligible for Medicaid but whose household income doesn’t exceed 175% of the poverty level. But this program, called Covered Connecticut, utilizes private marketplace/exchange plans rather than Medicaid.
HUSKY B (CHIP)
- 323% of FPL for children
HUSKY C/MED-Connect
- See income and asset criteria for aged, blind and disabled beneficiaries. For Medicare beneficiaries in Connecticut who need financial assistance, learn more here about the available programs and the financial requirements for eligibility.
HUSKY D
- 138% of FPL for childless adults
Apply for Medicaid in Connecticut
For HUSKY A, B or D: online at accesshealthct.com, under Get Health Coverage; by mail (call 1-877-284-8759 to have application mailed to you); by phone at 1-855-805- 4325
Eligibility: HUSKY A: Children ages 0-18 with incomes up to 196% FPL; pregnant women with incomes up to 258% FPL; parents of dependent children with incomes up to 155% of FPL.



ACA Medicaid eligibility expansion in Connecticut
Through a well-functioning state-run health insurance marketplace and a generous Medicaid program, Connecticut has shown commitment to helping its residents obtain affordable health insurance. In 2010, Connecticut was the first state to adopt the ACA’s Medicaid expansion for low-income adults under age 65, and the state has incrementally expanded eligibility for Medicaid for other populations in the years since then.
Most recently, Connecticut extended Medicaid/CHIP eligibility to undocumented immigrant children age 12 and younger, and extended postpartum Medicaid coverage so that it continues for 12 months instead of just 60 days.
As of February 2024, more than 950,000 people were covered by Medicaid (HUSKY Health) in Connecticut. In 2013, before the ACA’s Medicaid expansion was implemented, there were 634,518 people enrolled in Medicaid coverage. So enrollment had grown significantly, with Medicaid expansion being the primary driver of the growth. (Enrollment had been even higher, at about 1.04 million people, in early 2023. But it began to decline in the spring of 2023 when the pandemic-era continuous coverage rule ended and disenrollments resumed; this is discussed in more detail below.)
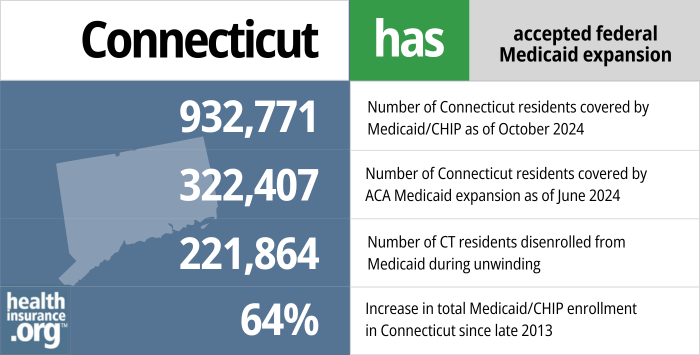
- 945,931 – Number of CT residents covered by Medicaid/CHIP as of October 20241
- 322,407 – Number of Connecticut residents covered by ACA Medicaid expansion as of June 20242
- 221,864 – Number of CT residents disenrolled from Medicaid during unwinding3
- 64% – Increase in total Medicaid/CHIP enrollment in Connecticut since late 20134
Explore our other comprehensive guides to coverage in Connecticut

This guide can help you find the right health plan in Connecticut for you and your family. For many, an Affordable Care Act (ACA) Marketplace/exchange plan, also called Obamacare, can be an affordable and robust coverage solution.
Learn about health insurance coverage options in Connecticut.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Connecticut.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Connecticut as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.
Learn about short-term insurance regulations in Connecticut.

Frequently asked questions about Connecticut Medicaid eligibility and enrollment
How do I enroll in Connecticut Medicaid?
To apply for HUSKY A, B, or D:
- Online at www.accesshealthct.com, under Get Health Coverage
- By mail: call 1-877-284-8759 to have an application mailed to you
- By phone at 1-855-805- 4325 (Access Health CT call center)
To apply for HUSKY C and Medicaid for Employees with Disabilities:
- Online at www.connect.ct.gov, under Apply for Benefits
- By mail: print an application in English or Spanish and mail it to DSS ConneCT Scanning Center, P.O. Box 1320, Manchester, Connecticut 06045-1320. For help completing the form, call 1-855-626-6632.
- For long-term care benefits, complete an application in English or Spanish and submit it to the Long-Term Care Application Center for your county.
How does Medicaid provide financial assistance to Medicare beneficiaries in Connecticut?
Many Medicare beneficiaries receive Medicaid financial assistance that can help them with Medicare premiums, lower prescription drug costs, and pay for expenses not covered by Medicare – including long-term care.
Our guide to financial assistance for Medicare enrollees in Connecticut includes overviews of these programs, including Medicaid long-term care benefits, Extra Help, and eligibility guidelines for assistance.
How is Connecticut handling post-pandemic Medicaid renewals?
After being paused for three years due to the pandemic, Medicaid disenrollments resumed in Connecticut at the end of April 2023. According to Connecticut data, more than 176,000 people had been disenrolled from Medicaid by December 2023.5 Most of those disenrollments — more than 132,000 — were procedural, meaning that the state didn’t have enough information to determine whether the person was still eligible.
Connecticut had reported in 2022 that roughly 42% of its MAGI-based Medicaid population was covered under the pandemic-related continuous coverage rules, meaning that their coverage had been extended beyond its normal renewal date due at some point since March 2020. (MAGI-based means eligibility based solely on income, which includes adults under 65, children, and pregnant women).
Connecticut has been using a time-based approach to processing the renewals, meaning that they began the process by conducting renewals that had been pending for the longest time and are working their way forward, spreading this out as evenly as possible over the 12-month “unwinding” period.
HUSKY Health enrollees should make sure that the Medicaid office has their current contact information, and should respond promptly to any requests for updated information.
People who are disenrolled from HUSKY can transition to an employer’s plan, if available (the deadline to enroll is 60 days after Medicaid terminates), or to a policy offered through Access Health CT, the state-run health insurance Marketplace (the deadline to enroll is 120 days after your HUSKY coverage ends;6 this is specific to Connecticut, as other states can have shorter enrollment windows).
Through November 2023, CMS reported that 10,630 Connecticut residents had transitioned from HUSKY to an Access Health CT plan by that point in the unwinding period.7
Legislation impacting Connecticut Medicaid
Changes to Connecticut Medicaid eligibility guidelines for parents
In 2014, childless adults became eligible for Medicaid coverage (HUSKY D) as a result of the ACA’s expansion of Medicaid. The federal government initially paid the full cost for this newly-eligible population, although the states began paying a portion of the cost in 2017, and now pay 10% of the cost (the 90/10 federal/state funding split will remain in place going forward). This program — Medicaid expansion under the ACA — is not changing.
But HUSKY A eligibility guidelines have changed for parents with dependent children. In an effort to trim costs, the state reduced the upper income limit for HUSKY A (only for parents) from 201% of the poverty level to 155% of the poverty level (effectively 160%, with the 5% income disregard). For new enrollees, the change was effective August 1, 2015. For existing enrollees, the change became effective August 31, 2015 if they did not have earned income from a job. For those who did have earned income from a job, the new eligibility guidelines became effective August 1, 2016.
The state noted that parents who were dropped from the HUSKY A rolls had access to subsidized coverage through Access Health CT, but advocates pointed out that there are considerably higher out-of-pocket costs for private plans in the exchange than there are with Medicaid (Connecticut has since created a new state subsidy program that covers the premiums and out-of-pocket costs for marketplace coverage for adults with income up to 175% of the poverty level). The Connecticut Mirror reported that as of September 11, 2015, only 140 out of 800 people who had lost coverage at the end of August had enrolled in new coverage through Access Health CT.
In May 2016, Access Health CT, the state-run exchange, announced that they were partnering with other state agencies to reach out to people who were going to lose access to HUSKY A on August 1, in an effort to get them signed up for new coverage (including, in some cases, other “Medicaid-funded assistance”). About 14,000 people were slated to lose coverage as of August 1, and by mid-July, only about 26% of them had enrolled in plans through Access Health CT. As of 2018, the estimate was that roughly 80% of the people who lost HUSKY A coverage as a result of the lower income cap had ended up uninsured.
In 2017, legislation was enacted to again reduce the income cap for HUSKY A eligibility, to 138% of the poverty level (the same as the income cap for Medicaid eligibility for childless, non-elderly adults under the ACA’s Medicaid expansion). This change took effect in January 2018, but people with income from employment (ie, most enrollees) had one extra year of coverage, so the new rules weren’t slated to take effect for most enrollees until January 2019.
But in May 2018, the state enacted a budget that reversed the HUSKY A eligibility cuts. As of July 2018, the HUSKY A income cap for parents was restored to 155% of the poverty level (160% with the income disregard). Parents who had lost coverage as of January were eligible to re-enroll, although most parents had income from employment and thus hadn’t yet lost coverage.
For perspective, 138% of the poverty level for a household of three is $35,631 in 2024. And 160% of the poverty level is $41,312 for a household of three. So parents earning a few extra thousand dollars no longer need to worry that they’re going to lose their health insurance. And the new Covered Connecticut program ensures that even with income a little above 160% of the poverty level, adults in Connecticut have access to zero-cost health coverage and medical care.
Connecticut a frontrunner in Medicaid expansion
Connecticut is one of 40 states and DC that have expanded Medicaid coverage to childless adults through an optional component of the Affordable Care Act. (Medicaid expansion was initially intended to be mandatory, but the Supreme Court ruled in 2012 that federal Medicaid funding could not be withheld from states that didn’t expand Medicaid, essentially making Medicaid expansion optional for states).
Connecticut took a two-step approach to expansion. In 2010, the state launched its HUSKY D program by transitioning very low-income adults from the State Administered General Assistance (SAGA) medical program into Medicaid. In 2014, it further expanded coverage for childless adults by raising the income limit to 138% of FPL, utilizing federal funding from the ACA to increase the eligibility threshold.
In January 2014, the Kaiser Family Foundation estimated that about 286,000 people in Connecticut were uninsured. KFF also estimated that, with Medicaid expansion, about 38% of those 286,000 would qualify for either Medicaid or CHIP. In an October 2014 press release, Access Health CT (the state-run marketplace) estimated that 147,000 Connecticut residents were still uninsured.
As of November 2023, more than 983,000 people were covered by HUSKY Health, up from 634,518 total enrollees in 2013. As noted above, this growth was driven primarily by Medicaid expansion coupled with the pandemic-era rules that prevented states from disenrolling anyone from Medicaid. This rule lasted from March 2020 through March 2023, and resulted in a steady increase in the number of people covered by Medicaid nationwide (enrollment has since declined due to the disenrollments that resumed in early/mid-2023).
Connecticut Medicaid history
Connecticut implemented Medicaid in July 1966, one year after the program was enacted at the federal level through Title XIX of the Social Security Act.
Unlike many states that are increasingly using Medicaid managed care to provide health coverage to low-income beneficiaries, Connecticut dropped its managed care contracts in 2012. Ellen Andrews, executive director of the Connecticut Health Policy Project, credits the change with increasing access for beneficiaries, improving quality, and reducing costs.
Connecticut is one of only four states with zero percent of the Medicaid population enrolled in managed care plans. Instead, Connecticut uses a self-insured fee-for-service approach to Medicaid. The state notes that administrative costs for HUSKY Health are just 4.5%, and estimates that they would be 10% if the state were to use a managed care approach to Medicaid. Although the program is self-insured, the state contracts with four administrative services organizations to administer HUSKY Health. Compared with national averages, HUSKY Health has had considerable success in controlling costs and reducing per-enrollee spending in Medicaid.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Connecticut?
Explore more resources for options in Connecticut including ACA coverage, short-term health insurance, dental insurance and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- “October 2024 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed February 2025 ⤶
- “Medicaid Enrollment – New Adult Group”, Medicaid.gov, Accessed February 2025 ⤶
- ”Medicaid Enrollment and Unwinding Tracker“, KFF.org, Accessed January 2025 ⤶
- “Medicaid Enrollment” KFF, and “May 2024 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed March 18, 2024 ⤶
- “Public Health Emergency (PHE) Unwinding – Renewal Outcomes” , Connecticut State Department of Social Services, Accessed March 20, 2024. ⤶
- ”Special Enrollment Periods” Access Health CT. Accessed March 20, 2024. ⤶
- ”State-based Marketplace (SBM) Medicaid Unwinding Report” Centers for Medicare & Medicaid Services. Data through November 2023. ⤶

