Medicaid eligibility and enrollment in Illinois

Nearly 900,000 people are covered under the state’s expansion of Medicaid

Who is eligible for Medicaid in Illinois?
Federal law specifies mandatory and optional coverage groups for Medicaid. States must cover the mandatory groups to receive federal Medicaid funding, and they qualify for additional funding if they cover optional groups. The federal government specifies minimum thresholds for eligibility for the various groups, and states can set their requirements at or above the minimum threshold. Illinois has established requirements that are near national averages.
Illinois’ eligibility standards for Medicaid are:
- Children ages 0-18 qualify with family income levels up to 147% of the federal poverty level (FPL); the Children’s Health Insurance Program covers children with family income up to 318% of FPL
- Someone who is pregnant will qualify with family income up to 213% of FPL (coverage for the mother extends for 12 months after the baby is born; Illinois was the first state to implement this extended postpartum coverage, although most of the rest of the states have followed suit)
- Adults under age 65 qualify with family income up to 138% of FPL
Note that all of those limits include a built-in 5% income disregard, which is part of the MAGI-based eligibility rules used to determine Medicaid eligibility for Medicaid expansion, pregnant people, and children.
Apply for Medicaid in Illinois
Apply online, or fill out an application and return it by mail or fax. You can also apply in person at the nearest Family Community Resource Center.
Eligibility: Children ages 0-18 with family income levels up to 142% of FPL. Pregnant women with family income up to 208% of FPL. Adults with family income up to 138% of FPL.



ACA’s Medicaid eligibility expansion in Illinois
Medicaid is an important part of overall health insurance enrollment and coverage in Illinois, with Medicaid and CHIP covering about 30% of the state’s 12.8 million residents. 3.93 million people in Illinois had Medicaid as of September 2023, up from 2.6 million in 2013 and 2.9 million prior to the COVID pandemic. As discussed above, Medicaid enrollment surged during the pandemic, but is expected to decline over the 12-month period that began in July 2023.
Nearly a quarter of those covered are eligible for Medicaid due to the state’s expansion of Medicaid under the Affordable Care Act (ACA). As of September 2023, there were 896,755 people covered under ACA Medicaid expansion in Illinois (this page provides updated totals over time).
Total Medicaid enrollment includes people who are eligible under the ACA’s expansion of Medicaid to low-income adults, as well as people who were already in one of the traditional Medicaid groups (low-income people who are also either pregnant, children, parents of minor children, aged, blind, or disabled residents). Most Illinois Medicaid enrollees are in one of those traditional eligibility groups. And Illinois was the first state to extend postpartum Medicaid coverage to 12 months, so the mother’s coverage no longer ends 60 days after the baby is born. (Most of the rest of the states have since extended postpartum Medicaid coverage to 12 months.)
Illinois’ uninsured rate dropped from 12.7% in 2013 to 7.4% in 2019 (it had been even lower in 2016, at 6.5%, but has crept up since then, reaching 7% as of 2021), and Medicaid played a significant role in that. Medicaid also served as an essential safety net during the pandemic, preventing people from becoming uninsured amid the widespread job losses in 2020.
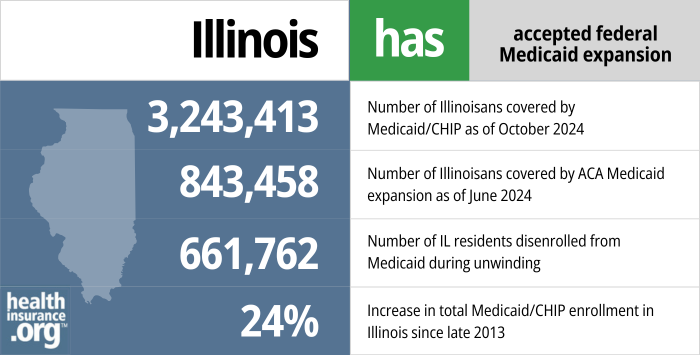
- 3,243,413 – Number of Illinoisans covered by Medicaid/CHIP as of October 20241
- 843,458 – Number of Illinoisans covered by ACA Medicaid expansion as of June 20242
- 661,762 – Number of IL residents disenrolled from Medicaid during unwinding3
- 29% – Increase in total Medicaid/CHIP enrollment in Illinois since January 20144
Explore our other comprehensive guides to coverage in Illinois

Illinois runs a partnership exchange with the federal government. The state operates Get Covered Illinois, which has a website, in-person help, and a help desk,1 but Illinois residents use the federally-run HealthCare.gov platform to enroll in Affordable Care Act (ACA) Marketplace health plans.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Illinois.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Illinois as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.

Frequently asked questions about Illinois Medicaid eligibility and enrollment
How do I enroll in Medicaid in Illinois?
You have several options to enroll in Medicaid in Illinois:
- Apply online using the Illinois website or Healthcare.gov (for non-disabled adults under age 65).
- Apply in person and get help from the Department of Human Services (DHS). Find the nearest Family Community Resource Center.
- Apply by mail or fax, or apply online or call at 1-800-843-6154 (TTY 1-800-447-6404) and ask DHS to mail you an application. Complete the application and mail or fax it back to the nearest Family Community Resource Center.
How does Medicaid provide assistance to Medicare beneficiaries in Illinois?
Many Medicare beneficiaries also receive assistance through Medicaid. This includes help with Medicare premiums, cost sharing, prescription drug costs, and services not covered by Medicare – such as long-term care expenses.
Our guide to financial resources for Medicare beneficiaries in Illinois describes these programs, including Medicare Savings Programs, Medicaid long-term care benefits, and guidelines for eligibility.
How is Illinois handling Medicaid renewals after the pandemic?
During the COVID pandemic, states were prohibited from disenrolling people from Medicaid, even if they no longer met the eligibility guidelines. This rule was in use for three years, from March 2020 through March 2023. But states have since resumed regular eligibility redeterminations and disenrollments.
States had some flexibility on the timing of the return to normal procedures, and Illinois opted to delay this as long as possible. The state began sending renewal notices in late April, for people whose Medicaid was due to renew in June. The first round of disenrollments came on July 1 — three months after the earliest possible date allowed by the federal government.
Total Medicaid enrollment in Illinois peaked in July, with 3,969,148 people covered. By September, total enrollment had dropped to 3,932,604, for a decline of 36,544 people (note that this does not represent the total number of people disenrolled, as new people join the Medicaid rolls each month too, and the Illinois enrollment page shows total enrollment).
Illinois is using enrollees’ regularly scheduled renewal date, which enrollees can find at abe.illinois.gov. Renewals are available via that website starting one month before they’re due, and enrollees can renew online once their renewal is available. The state will automatically renew benefits when they have enough information to do that (they expect to be able to auto-renew about a third of enrollees), but will otherwise notify the enrollee that their renewal needs to be completed, either online or with a paper form. The state is encouraging people to use the online renewal whenever possible.
Enrollment in Illinois Medicaid grew by about one million people during the pandemic, from 2.9 million to 3.9 million (as noted above, it peaked at about 3.97 million in July 2023). The state expects about 32,000 people to lose their coverage during each month of the 12-month “unwinding” period, with about 384,000 people losing coverage once all of the eligibility redeterminations are processed.
Most of these people will be eligible for employer-sponsored health coverage or for a subsidized plan through the Illinois exchange/marketplace (getcoveredillinois.gov, which uses the HealthCare.gov enrollment platform). Enrollment windows for employer-sponsored coverage are time-limited. And although HealthCare.gov is offering an extended 16-month enrollment window for people who lose Medicaid during the “unwinding” period, it’s still important to sign up prior to the date that Medicaid terminates, in order to avoid a gap in coverage. There is also a special enrollment period during which people can transition from Medicaid to Medicare without late enrollment penalties, if they’re now eligible for Medicare.
Legislation impacting Illinois Medicaid
Medicaid funding for enhanced mental health care
In September 2016, Illinois officials requested permission from the federal government to use existing Medicaid funds (with no changes to eligibility or funding) to test different approaches to treating Medicaid enrollees who need mental health and/or substance abuse treatment. The state had planned to implement the changes in July 2017, but CMS didn’t approve the waiver proposal until May 2018.
The idea is to focus more on preventive care, supportive housing services, and community-based care, rather than institutional care. The state notes that while 25% of Illinois Medicaid enrollees have mental health and/or substance abuse diagnoses, their treatment accounts for 56% of the Medicaid program’s total cost.
Under the terms of the approved waiver, Illinois is running ten pilot projects that provide coverage for services that weren’t previously covered by Medicaid, including short-term inpatient substance abuse treatment, services to help people manage withdrawals during substance abuse recovery, home health visits for new babies and for children born to opioid-addicted mothers, and job coaching and transportation services designed to help people obtain and keep employment.
Hepatitis C drug coverage expanded in stages, now available to anyone with the disease
Drugs that can cure Hepatitis C burst onto the medical scene several years ago, heralded as miracles. But they can also be a strain on budgets, as the pill initially could cost more than $1,000 per day, and the treatment course lasts 12 weeks. Medicaid programs across the country grappled with how to handle the situation, and Illinois announced in September 2016 that they would loosen their guidelines in terms of when Hepatitis C drugs would be covered.
Rather than restricting coverage only to the sickest patients, Illinois Medicaid began to cover Hepatitis C drugs for people with stage 3 and 4 liver scarring, rather than just 4. Advocates cheered the new rules, but cautioned that there was still no coverage for treatment in people with chronic Hepatitis C that hadn’t progressed as far as stage 3 liver scarring, and urged the state to continue to consider the issue.
By 2018, the price of Hepatitis C medications had declined, and a generic version was set to hit the market in early 2019, priced at $24,000 for the full treatment course (as opposed to $90,000 in the early years that the drug was available). And in October 2018, Illinois eliminated the restrictions on access to Hepatitis C drugs, allowing several thousand Illinois residents to obtain Hepatitis C medication through Medicaid, regardless of the stage of their disease and without having to prove sobriety.
Illinois Medicaid history
Medicaid was implemented in the state of Illinois in January 1966.
Individuals covered by Medicaid in Illinois can choose either a fee-for-service plan or a managed care plan.
Illinois has been slower than many other states in moving beneficiaries to managed care plans. However, the state did pass a law in 2011 that required expanding managed care to at least half the state’s Medicaid beneficiaries by Jan. 1, 2015. As of 2022, more than 80% of Illinois Medicaid enrollees were covered under Medicaid managed care plans.
In June 2014, then-Governor Pat Quinn signed a Medicaid reform bill. The law restored adult dental care and podiatry services, aligns Illinois law with federal law to provide Medicaid coverage to children who have been without private insurance for three months, streamlines hospital and nursing-home reimbursement, and more.
Illinois opted to expand Medicaid eligibility, as allowed by the ACA, in July 2013 for a January 1, 2014 effective date. Making Medicaid available to low-income, non-elderly adults is a key part of the Affordable Care Act’s strategy to reduce the nation’s uninsured rate. However, a Supreme Court ruling made Medicaid expansion optional, and as of the fall of 2023, there were still 11 states that had not expanded Medicaid (North Carolina will expand Medicaid in December 2023, reducing the number of non-expansion states to ten).
At the time Medicaid expansion was approved, Illinois officials estimated that 342,000 Illinois residents would qualify. But according to the Chicago Tribune, about 350,000 new enrollees were approved in just the first several months, by June 2014. And a little over a year later, by August 2016, total enrollment in the state’s Medicaid expansion program had exceeded 646,000. But enrollment had dropped to 606,670 people as of July 2018, and remained at a very similar level (607,404) as of April 2020. That was still far higher than the state had initially projected, but lower than it had been a few years earlier.
However, the COVID pandemic pushed Medicaid enrollment (including Medicaid expansion enrollment) much higher in Illinois, as was the case nationwide. By July 2023 (when total Medicaid enrollment peaked in Illinois, before starting to decline due to post-pandemic disenrollments), there were nearly 906,000 people covered under Medicaid expansion in Illinois. That number is expected to decrease somewhat through mid-2024, due to the return to normal eligibility redeterminations and disenrollments after the pandemic (details above).
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Illinois?
Explore more resources for options in Illinois including ACA coverage, short-term health insurance, dental insurance and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”October 2024 Medicaid & CHIP Enrollment Data Highlights“, Medicaid.gov, Accessed January 2025 ⤶
- “Medicaid Enrollment – New Adult Group”, Medicaid.gov, Accessed February 2025 ⤶
- “Illinois Department of Healthcare and Family Services” , hfs.illinois.gov, Accessed January 2025 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed February 2025 ⤶

