Medicaid eligibility and enrollment in Pennsylvania

3.2 million Pennsylvanians enrolled in Medical Assistance, down from 3.7 million in April 2023.

Who is eligible for Medicaid in Pennsylvania?
Pennsylvania Medicaid, which is called Medical Assistance, is available to the following populations (these limits all include a built-in 5% income disregard that’s added to the official eligibility limits):
- Children aged 0-1: 220% of the federal poverty level (FPL)
- Children aged 1-5: 162% of FPL
- Children age 6-18: 138% of FPL
- Children who aren’t eligible for Medical Assistance can enroll in CHIP with household income up to 319% of FPL
- Someone who is pregnant: 220% of FPL (coverage for the mother continues for a year after the birth1)
- Adults under age 65: 138% of FPL (this is the Medicaid expansion population)
Apply for Medicaid in Pennsylvania
Online, at COMPASS.state.pa.us; by phone, at 1-866-550-4355; or in person or with a paper application at local County Assistance Offices.
Eligibility: Adults with income up to 138% of FPL are eligible for Medicaid. Children in households with incomes up to 319% of FPL are eligible for Medicaid or CHIP.



ACA’s Medicaid eligibility expansion in Pennsylvania
Pennsylvania expanded Medicaid as of January 1, 2015, a year after coverage expansion first became available under the ACA. By 2023, more than 1.1 million Pennsylvanians were covered under Medicaid expansion (this is the Group VIII population in enrollment reports). This was quite a bit higher than the state initially projected, but that’s because the COVID pandemic pushed Medicaid enrollment much higher nationwide, due to an extended pause on disenrollments.
Initially, Pennsylvania took a modified approach to Medicaid expansion. The program was called Healthy Pennsylvania and utilized an 1115 waiver. But Governor Tom Wolf took office in January 2015, and almost immediately began transitioning Pennsylvania to an unmodified version of Medicaid expansion. The Healthy Pennsylvania waiver was terminated, and Medicaid expansion has been in place in Pennsylvania, without modification, ever since.
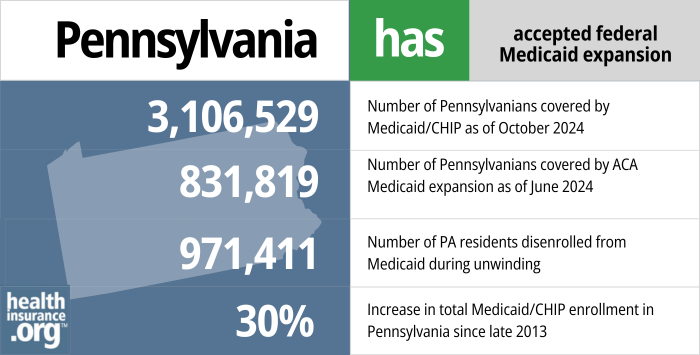
- 3,106,529 – Number of Pennsylvanians covered by Medicaid/CHIP as of October 20242
- 831,819 – Number of Pennsylvanians covered by ACA Medicaid expansion as of June 20243
- 971,411 – Number of PA residents disenrolled from Medicaid during unwinding4
- 30% – Increase in total Medicaid/CHIP enrollment in Pennsylvania since late 20135
Explore our other comprehensive guides to coverage in Pennsylvania

We’ve created this guide to help you understand the Pennsylvania health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.
Learn about health insurance coverage options in Pennsylvania.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Pennsylvania.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Pennsylvania as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.
Learn about short-term insurance regulations in Pennsylvania.

Frequently asked questions about Pennsylvania Medicaid
How do I apply for Medicaid in Pennsylvania?
Medicaid is called Medical Assistance in Pennsylvania. You can apply online, by phone, or by mail, fax, or in person.
- Online: Visit the COMPASS website
- Phone: Call the Consumer Service Center for Health Care Coverage at 1-866-550-4355.
- Mail/Fax/In Person: Download an application and submit it to your local county assistance office (CAO) by mail or fax, or drop it off in person.
How does Medicaid provide financial assistance to Medicare beneficiaries in Pennsylvania?
Many Medicare beneficiaries receive Medicaid’s help with paying for Medicare premiums, affording prescription drug costs, and covering expenses not reimbursed by Medicare – such as long-term care.
Our guide to financial assistance for Medicare enrollees in Pennsylvania includes overviews of these benefits, including Medicare Savings Programs, long-term care coverage, and eligibility guidelines for assistance.
How is Pennsylvania handling Medicaid renewals after the pandemic?
Between March 2020 and March 2023, states could not disenroll people from Medicaid, even if they were no longer eligible or didn’t respond to a renewal notice. That rule ended March 31, 2023, and states could resume disenrollments as early as April 1.
In Pennsylvania, the first round of disenrollments for Medical Assistance and CHIP came at the end of April 2023. Eligibility redeterminations and disenrollments have continued each month since then. Total enrollment in Pennsylvania Medicaid/CHIP has dropped from 3.7 million people in April 2023 to less than 3.2 million in March 2024.6
By March 2024, a total of 848,421 people had been disenrolled from Pennsylvania Medicaid, while coverage had been renewed for 2,016,588 enrollees.7
This webinar and this webinar are both good resources with helpful information about the unwinding process in Pennsylvania and the return to normal eligibility protocols.
Pennsylvania continued to send out renewal notices throughout the pandemic, and many people completed those and had up-to-date information on file. Out of more than 3.6 million Medical Assistance/CHIP enrollees, Pennsylvania officials noted in early 2023 that they had received information from 617,000 enrollees indicating that they were no longer eligible for the coverage (presumably most of these individuals have since been disenrolled). And they had another 577,000 enrollees who did not respond to a renewal notice during the pandemic — meaning that the state didn’t know whether those people were still eligible or not.
Of the people disenrolled from Pennsylvania Medicaid by march 2024, 53% were disenrolled because the state didn’t have enough information to determine whether they were still eligible, while the other 47% completed the renewal paperwork but were deemed ineligible.7
When a person is no longer eligible for Medical Assistance or CHIP, they have the option to enroll in an employer’s plan (if available), Medicare (if they’ve become eligible for Medicare during the Medicaid continuous coverage period and thus didn’t sign up for Medicare when they were first eligible), or an individual/family plan obtained via Pennie, the state-run exchange/marketplace in Pennsylvania.
By January 2024, a total of 67,488 Pennsylvania residents had transitioned from Medicaid to a private health plan obtained via Pennie.8
Pennie is offering a 120-day special enrollment period for people who lose Medical Assistance coverage during the unwinding period9 (this is longer than the normal 60-day window, but much shorter than the 20-month window that’s being offered in the states that rely on the federally-run exchange, HealthCare.gov). But it’s important to note that Pennie is allowing retroactive seamless coverage if the person chooses a new plan within 60 days of the Medical Assistance termination date. In most states, you have to sign up for the new plan before Medicaid ends in order to avoid a gap in coverage, but that’s not the case in Pennsylvania.
If a person completes their Medical Assistance renewal packet and are found to no longer be eligible, their information is automatically transferred to Pennie, with an account created in their name and their financial assistance determined based on the information they provided in their Medicaid renewal form. Pennie will then contact them and provide them with a code they can use to access their new account, and all they’ll need to do is pick a new plan within 120 days (preferably within 60 days, as that will ensure there’s no gap in coverage).
If a person does not return their Medical Assistance renewal packet and thus loses coverage because the state can’t determine whether they’re eligible or not, their information will also be forwarded to Pennie. But Pennie won’t have the pertinent details to create an account and determine eligibility for financial assistance, so the person will need to set that up and provide the necessary information to move forward with getting coverage. They will still have the same 120-day special enrollment period and 60-day window for retroactive coverage.
Legislation impacting Pennsylvania Medicaid
Lawmakers passed work requirement bill in 2018, but Governor Wolf vetoed it
Medicaid work requirements gained traction in 2018, with the Trump administration granting approval for five states’ proposed work requirements, and several more waiting in the wings. In general, the process began with a state enacting legislation calling for a work requirement, and then the state submitting a proposal to CMS, seeking federal approval to implement the work requirement. (The Biden administration revoked federal approval for work requirements in all of the states where the Trump administration had granted it.)
In Pennsylvania, lawmakers passed H.B.2138 in 2018, which would have directed the state to seek federal permission to require non-exempt Medicaid enrollees to work at least 20 hours per week (or complete at least 12 job-training activities each week) in order to maintain eligibility for the program. But Governor Wolf vetoed the legislation.
Wolf had vetoed similar legislation in 2017, and was steadfast in his opposition to Medicaid work requirements. Although work requirements appeal to conservative lawmakers, they do not further the mission of Medicaid, which is to promote health coverage and access to medical treatment. Instead, they simply result in more people joining the ranks of the uninsured.
During the 2018 governor’s race in Pennsylvania, Wolf’s GOP challenger, Scott Wagner, criticized Wolf’s veto of the work requirement legislation, and noted that he would sign such a bill if he were governor. Wolf won the election, but Pennsylvania’s legislature maintained a Republican majority. Under the Biden administration, however, Medicaid work requirements are a non-starter, even if a state does enact legislation calling for a work requirement.
Medicaid expansion in 2015 with a waiver, but soon replaced by straight expansion
Former Governor Corbett originally announced that the state would not move forward with Medicaid expansion, but reversed his course in late summer 2013, saying that the state was negotiating with the federal government to create its own version of Medicaid expansion (Healthy Pennsylvania). That version used federal funds to subsidize private health insurance for low-income residents instead of enrolling them in Medicaid, and added restrictions that would remove some people from Medicaid or charge them a “modest monthly premium.”
Corbett’s plan was very controversial in Pennsylvania, among lawmakers and residents alike. On March 5, 2014, a letter from Corbett to then-Secretary of HHS, Kathleen Sebelius, outlined his loosening of the requirement that Medicaid recipients be actively searching for work, but his proposal did still include a work requirement. Ultimately, the work requirement was dropped from the Healthy Pennsylvania program, but the state established a voluntary job training and career coaching program (dubbed Encouraging Employment) that could let participating enrollees have lower cost-sharing (the Trump Administration did approve Medicaid work requirements, but the Obama administration never did, and Corbett’s waiver was being considered during the Obama Administration).
Under Corbett’s plan, no premiums would be charged for Healthy Pennsylvania in 2015, but starting in 2016 the program would have charged up to 2% of income for enrollees with incomes between 100% and 138% of the poverty level (enrollees would have been able to qualify for premium reductions if they completed an annual wellness exam and paid required co-payments in a timely manner). In addition, Healthy PA had three different plan designs depending on health status and eligibility, as opposed to a single Medicaid system for all enrollees.
In June 2014, the Corbett Administration had received a strong response from insurance carriers interested in participating in his Healthy PA program: For some regions of the state, as many as six insurers had placed bids, while the Administration had been hoping for at least two per region. In all, nine insurers were approved by the state to participate in the Healthy PA program that was approved by HHS in late August 2014.
Through these private insurers, newly-eligible Healthy Pennsylvania enrollees were covered under a private, managed care Medicaid program — very similar to what Pennsylvania and many other states already used for existing Medicaid coverage. Although by early October, there were some indications that the carriers providing managed care Medicaid coverage in Pennsylvania were having difficulty getting enough providers to participate in their networks because of the relatively low reimbursement rates compared with commercial plans.
But the complicated waiver-sanctioned Medicaid expansion program in Pennsylvania was short-lived, and the process of dismantling it began almost as soon as Healthy PA coverage started to become effective. When Governor Wolf took office in 2015, he began the process of switching the state to the much less complicated Medicaid expansion program outlined in the ACA — no waivers required.
Transition to HealthChoices
Governor Wolf wasted no time in starting the process of switching to a more simplified version of Medicaid expansion. By April 2015, the transition had begun, and the first round of enrollees had their coverage switched to HealthChoices as of June 1 (HealthyChoices is the name of Pennsylvania’s Medicaid managed care program). This included everyone who was already covered by Pennsylvania Medicaid prior to January, as well as new applicants who enrolled after the end of April. The remaining enrollees switched to HealthChoices on September 1, 2015.
In the transition to HealthChoices, people who enrolled in a managed care plan through Healthy Pennsylvania’s Private Coverage Option were given a choice of managed care providers in the HealthChoices program. But while Healthy PA had three different plan designs, HealthChoices provides all enrollees with the same benefits in an effort to reduce confusion in the state’s Medicaid system.
The state created a 60-second video clip explaining the transition from Healthy PA to HealthChoices.
New eligibility guidelines took effect in 2015
Since January 1, 2015, all legally present adults under age 65 in the Commonwealth of Pennsylvania – parents or not – are eligible for Medicaid with household incomes up to 138% of poverty, as long as they meet Medicaid’s immigration requirements. Children are still eligible for Medicaid or CHIP if their household income doesn’t exceed 319% of the poverty level.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Pennsylvania?
Explore more resources for options in Pennsylvania including ACA coverage, short-term health insurance, dental insurance and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”Pennsylvania Medical Assistance Bulletin” Pennsylvania Department of Human Services. Mar. 31, 2022 ⤶
- “October 2024 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed January 2025 ⤶
- “Medicaid Enrollment – New Adult Group”, Medicaid.gov, Accessed February 2025 ⤶
- ”Federal Unwinding Reports“, Pa.gov, Accessed January 2025 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed February 2025 ⤶
- “Monthly Enrollment Status Changes” Pennsylvania Department of Human Services. Accessed May 8, 2024 ⤶
- ”Medicaid Continuous Coverage Unwinding Data“, Pennsylvania Department of Human Services, Accessed May 8, 2024 ⤶ ⤶
- ”State-based Marketplace (SBM) Medicaid Unwinding Report” Centers for Medicare & Medicaid Services. Data through January 2024. ⤶
- ”Special Enrollment Period Quick Reference Guide” Pennie. January 1, 2024 ⤶

