Medicaid eligibility and enrollment in Colorado

Colorado’s net Medicaid enrollment percentage decrease during “unwinding” was the nation’s highest. Low-income undocumented pregnant people and children will be Medicaid-eligible as of 2025

Who is eligible for Medicaid in Colorado?
Since 2016, Colorado Medicaid has been called Health First Colorado. Colorado’s income limits for Medicaid eligibility are:
- Children up to age 18: Up to 147% of FPL to qualify for Medicaid
- Children up to age 18 who aren’t eligible for Medicaid can qualify for Child Health Plan Plus (CHP+; Colorado’s CHIP coverage) with household income up to 265% of FPL.
- Coverage is available to lawfully-present immigrant children. As of 2025, income-eligible children who are undocumented immigrants will also be eligible for Medicaid/CHP+.
- Pregnant women: Up to 200% of FPL to qualify for Medicaid. Coverage for pregnant women continues for a year after the birth
- Pregnant women who don’t qualify for Medicaid can qualify for CHP+ with family income up to 265% of FPL
- Coverage is available to lawfully present immigrants who are pregnant. As of 2025, this coverage will also be available to undocumented pregnant people who would otherwise qualify for Medicaid/CHP+ except for their immigration status;
- Adults under the age of 65 can enroll in Health First Colorado with household income up to 138% of FPL (this is Medicaid expansion under the ACA)
Note that “income” refers to an ACA-specific version of modified adjusted gross income (MAGI). All of the above income limits include a 5% income disregard that’s added to MAGI for the purposes of determining Medicaid/CHIP eligibility for children, pregnant women, and nonelderly adults.
Apply for Medicaid in Colorado
Pregnant women, as well as children from birth through age 18 with family income levels up to 265% of FPL; Nonelderly adults — with or without dependent children — with incomes up to 138% of FPL.
Eligibility: Children 0-18 with family incomes up to 147% of FPL; children with family incomes up to 265% of FPL qualify for Child Health Plan Plus (CHP+); pregnant women with family income up to 200% of FPL; (pregnant women with family income up to 265% of FPL qualify for CHP+); non-elderly adults with family income up to 138% of FPL; some individuals who are elderly or disabled.



ACA Medicaid eligibility expansion in Colorado
One of the Affordable Care Act’s primary strategies for reducing the uninsured rate is Medicaid expansion to cover low-income adults under the age of 65. (Eligibility rules did not change for adults age 65 or older; they are still subject to both income and asset limits for Medicaid eligibility. Here’s how that works in Colorado.)
Then-Governor John Hickenlooper signed the legislation authorizing Medicaid expansion in May 2013. As of 2022, Medicaid expansion (Group VIII) enrollment in Colorado was 547,571, accounting for more than a third of the state’s total Medicaid enrollment.
Medicaid enrollment in Colorado grew by 72% in the first two years of Medicaid expansion implementation. Medicaid enrollment growth had largely leveled off by 2016/2017, but it spiked again in 2020, due to the COVID pandemic, and grew for the next three years due to the pandemic-related rule that prevented states from disenrolling Medicaid members between March 2020 and March 2023. But by mid-2024, Colorado’s Medicaid enrollment had dropped back down to roughly pre-pandemic levels (see more details below).
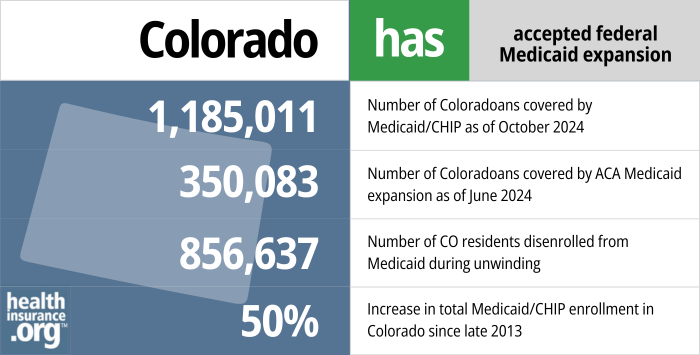
- 1,185,011 – Number of Coloradoans covered by Medicaid/CHIP as of October 20241
- 350,083 – Number of Coloradoans covered by ACA Medicaid expansion as of June 20242
- 856,637 – Number of CO residents disenrolled from Medicaid during unwinding3
- 50% – Increase in total Medicaid/CHIP enrollment in Colorado since late 20134
Explore our other comprehensive guides to coverage in Colorado

This guide is designed to help you understand your Colorado health insurance options and possible financial assistance available to you and your family — including federal subsidies and Colorado’s state-funded subsidies.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Colorado.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Colorado as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.

Frequently asked questions about Colorado Medicaid eligibility and enrollment
How do I enroll in Medicaid in Colorado?
If you think you may qualify for Health First Colorado Medicaid, you can apply a number of ways:
- Online at Colorado PEAK. (PEAK stands for Program Eligibility and Application Kit.) Colorado PEAK is a website for applying for food, cash, and medical assistance programs. Colorado’s state-run health insurance exchange (Connect for Health Colorado) connects with PEAK, so you’ll be able to enroll in Medicaid or CHIP if you start at the exchange website, too.
- In person at your county office.
- By telephone: 1-800-221-3943 (TDD: 1-800-659-2656).
- By mail: print an application, fill it out, and mail it to the address included on the application form. You can also get a form at your county office or an application assistance site.
How does Medicaid provide financial assistance to Medicare beneficiaries in Colorado?
Many Medicare beneficiaries receive Medicaid financial assistance that can help them with Medicare premiums, lower prescription drug costs, and pay for expenses not covered by Medicare – including long-term care.
Our guide to financial assistance for Medicare enrollees in Colorado includes overviews of these programs, including Medicaid nursing home benefits, Extra Help, and eligibility guidelines for assistance.
How did Colorado handle Medicaid renewals after the pandemic?
As is the case in every state, Medicaid disenrollments were paused in Colorado from March 2020 through March 2023. The Medicaid continuous coverage requirement ended March 31, 2023, and disenrollments for people who are no longer eligible could resume as early as April 1, 2023.
Health First Colorado (Colorado Medicaid) began the first round of eligibility redeterminations in mid-March 2023, sending renewal packets to enrollees whose coverage was due to renew in May. The first round of coverage terminations (for people who were no longer eligible or who didn’t respond to the state’s request for eligibility verification) came at the end of May 2023, and Colorado wrapped up the “unwinding” process in April 2024.5
Colorado had about 1.7 million people enrolled in Medicaid/CHIP (CHP+) as of early 2023 (peak enrollment came in May 2023, with 1.8 million people6). Of those enrollees, approximately 768,000 were enrolled due to the pandemic-related continuous coverage requirement, which meant that the state either had information indicating that they were no longer eligible, or the state had not been able to verify their ongoing eligibility.
Ultimately, Health First Colorado Medicaid enrollment dropped back to pre-pandemic levels by the end of the unwinding period. There had been 1.25 million enrollees as of March 2020, and enrollment had dropped to about 1.26 million by mid-2024, after peaking at 1.8 million in mid-2023.6
The unwinding process has not been without controversy in Colorado. The Colorado Medicaid program has said that it makes sense that enrollment has returned to pre-pandemic levels.7 But it’s noteworthy that Colorado’s overall percentage drop in net Medicaid enrollment (through April 2024) was higher than every other state: 31.8%, versus a national average of 13.9%.8
Colorado Medicaid history and details
Medicaid expanded to cover undocumented pregnant people as of 2025
In June 2022, Colorado Gov. Jared Polis signed HB1289 into law (details here). Under the terms of the new law, Medicaid and CHIP coverage will be available, starting in 2025, to undocumented pregnant people and children who would otherwise be eligible except for their immigration status.
Colorado was already one of the states that provided Medicaid/CHIP coverage to lawfully present immigrant children and pregnant women who hadn’t yet been in the U.S. for five years (there is normally a five-year wait before a lawfully present immigrant can obtain Medicaid or CHIP, but states can opt to waive that waiting period).
But starting in 2025, Colorado will join several other states that are using state funds to provide Medicaid/CHIP coverage to undocumented children and undocumented pregnant people who would otherwise qualify based on their income. And postpartum Medicaid coverage will continue for a year after the baby is born, helping to improve maternal health in Colorado.
Colorado Medicaid history
The federal legislation establishing Medicaid was enacted in 1965, and Colorado authorized its program in 1969. Milestones in Colorado’s Medicaid and Child CHP+ programs, as well as federal Medicaid legislation, are detailed on the Colorado Center on Law & Policy website.
Medicaid expansion in Colorado went into effect Jan. 1, 2014, and Colorado Medicaid enrollment is 50% higher in 2024 than it had been in 2013.9 The growth includes both those who were newly eligible under Medicaid expansion as well those who qualified under existing eligibility criteria but had not previously enrolled.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Colorado?
Explore more resources for options in Colorado including ACA coverage, short-term health insurance, dental insurance and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”October 2024 Medicaid & CHIP Enrollment Data Highlights” Medicaid.gov, Accessed January 2025 ⤶
- “Medicaid Enrollment – New Adult Group”, Medicaid.gov, Accessed February 2025 ⤶
- “Continuous Coverage Unwind Reports” hcpf.colorado.gov, Accessed January 2025 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed February 2025 ⤶
- ”Continuous Coverage Unwind Data Reporting — Executive Summary” Colorado Department of Health Care Policy and Financing. Accessed Aug. 27, 2024 ⤶
- ”Continuous Coverage Unwind Data Reporting — Where Are We Now? Returning to Prepandemic Enrollment Levels” Colorado Department of Health Care Policy and Financing. Accessed Aug. 27, 2024 ⤶ ⤶
- ”Colorado dropped Medicaid enrollees as red states have, alarming advocates for the poor” Rocky Mountain PBS. July 14, 2024 ⤶
- ”Medicaid Enrollment and Unwinding Tracker” KFF. Aug. 23, 2024. ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed May 2024 ⤶

