
Medicaid eligibility and enrollment in Georgia
Partial Medicaid expansion, with a work requirement: Georgia forfeits enhanced federal funding, and covers far fewer people than full expansion.

Who is eligible for Medicaid in Georgia?
The criteria for enrollment in Georgia Medicaid are set at the following levels for non-disabled adults (note that these income limits include a built-in 5% income disregard that’s used for MAGI-based Medicaid eligibility determinations):1
- Children up to age 1 with family income up to 210% of federal poverty level (FPL)
- Children ages 1-5 with family income up to 154% of FPL
- Children ages 6-18 with family income up to 138% of FPL
- Pregnant women with family income up to 225% of FPL (coverage for the mother continues for 12 months after the baby is born)2
- Parents of minor children with family income up to 36% of FPL
- Adults with income under the poverty level can enroll in Medicaid if they comply with the state’s requirement to work at least 80 hours per month and report their work hours to the state.3
Georgia has not expanded Medicaid under the ACA, so non-disabled low-income adults without dependent children are only eligible for Medicaid if they have income under the poverty level and comply with the Georgia Pathways work requirement, including reporting the hours they work.3
for 2026 coverage
0.0%
of Federal Poverty Level
Apply for Medicaid in Georgia
Online at either Georgia Gateway or healthcare.gov; in person (Call 1-877-423-4746 for directions to a local office.) Submit a paper application by mail, fax or in person. (Contact your DFCS county office for an application.)
Eligibility: Children up to age 1 with family income up to 205% of FPL; children 1-5 with family income up to 149% of FPL; children 6-18 with family income up to 133% of FPL; pregnant women with family income up to 220% of FPL; parents with family income up to 35% of FPL; individuals who are elderly, blind and disabled (See income and resource limits.)



Has Georgia expanded Medicaid under the ACA?
No, Georgia has not implemented the ACA’s expansion of Medicaid. Legislation calling for Medicaid expansion was introduced in Georgia’s legislature in early 2025.4 Additional legislation was also introduced in early 2025 that would direct the state to seek a federal waiver to allow for a privatized version of Medicaid expansion, much like the approach that Arkansas uses.5
The private option legislation, if approved by state lawmakers and CMS, calls for adults with income up to 138% of the federal poverty level to be enrolled in private plans through the Georgia health insurance Marketplace (Georgia Access) using Medicaid funding.
Note that Georgia enacted a law in 2014 that requires legislative approval to expand Medicaid. So a governor in Georgia could not expand Medicaid on their own, without legislative approval.6
As discussed in more detail below, Georgia partially expanded Medicaid (up to the poverty level, instead of 138% of the poverty level as called for in the ACA) in 2023, but with a work requirement for eligibility. Enrollment in that program (Georgia Pathways) has remained very low, with only about 4,900 people enrolled as of late 2024.7 And most of the money spent on the program has been used for administration, as opposed to providing benefits to Georgia residents.8
However, the state’s proposed waiver extension for Georgia Pathways calls for the removal of the ongoing work reporting requirement, and would switch to an approach where compliance with the work requirement is verified only when a person applies and at their annual renewal.9
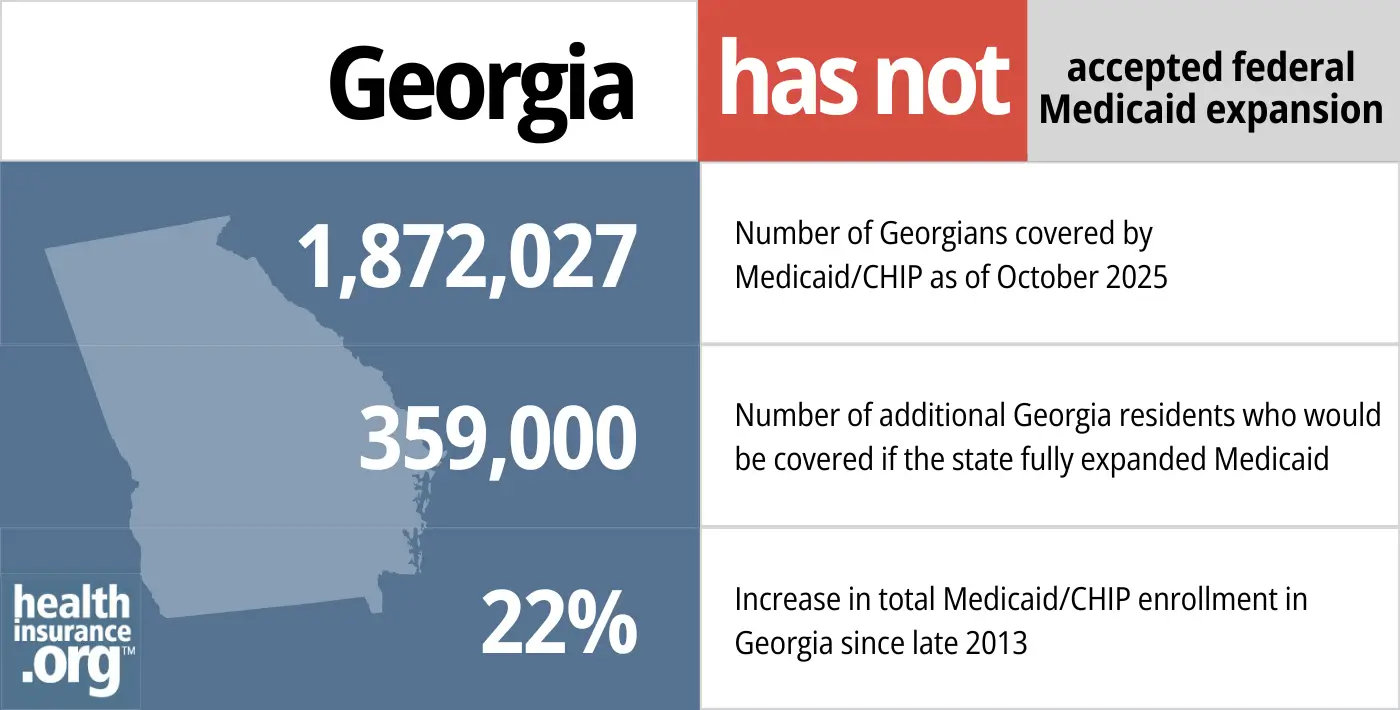
- 1,872,027 – Number of Georgians covered by Medicaid/CHIP as of October 202510
- 359,000 – Number of uninsured Georgia residents who would be covered if the state fully expanded Medicaid11
- 22% – Increase in total Medicaid/CHIP enrollment in Georgia since late 201312
Explore our other comprehensive guides to coverage in Georgia

The ACA Marketplace allows individuals and families to shop for and enroll in ACA-compliant health insurance plans. Subsidies may be available based on household income to help lower costs.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Georgia.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Georgia as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.

Frequently asked questions about Georgia Medicaid eligibility and enrollment
How can I enroll in Georgia Medicaid?
There are several ways you can apply for Medicaid in Georgia:
- Complete an online application at either Georgia Gateway or www.healthcare.gov.
- Call the Division of Family and Children Services (DFCS) information line at 1-877-423-4746. You will be directed to a local office that can help you.
- Complete a paper application. Contact your DFCS county office and ask them to mail you an application. You can return it by mail, fax, or in person.
How does Medicaid provide financial help to Medicare beneficiaries in Georgia?
Many Medicare beneficiaries receive assistance from Medicaid with Medicare premiums, prescription drug costs, and expenses not covered by Medicare – including long-term care.
Our guide to financial assistance for Medicare enrollees in Georgia includes overviews of these programs, including Medicaid nursing home benefits, Extra Help, and eligibility guidelines for assistance.
How many people were disenrolled from Georgia Medicaid after the pandemic?
Medicaid disenrollments were paused for three years during the COVID pandemic, meaning that people weren’t disenrolled from Medicaid even if their circumstances changed and they were no longer eligible. But that ended as of April 2023, and states resumed disenrolling people who are no longer eligible for Medicaid. Under federal rules, all Medicaid enrollees’ eligibility had to be redetermined at some point during a 14-month “unwinding” period that began in the spring of 2023.
The first round of Medicaid disenrollment in Georgia came in May 2023. By the end of the unwinding period, more than 802,000 people in Georgia had been disenrolled from Medicaid, while coverage had been renewed for nearly 989,000 people.13
CMS reported that 265,606 people transitioned from Georgia Medicaid to Marketplace coverage during the unwinding process.14
Georgia created its own state-developed protocol for the return to regular Medicaid eligibility redeterminations. The state spread eligibility redeterminations over multiple months, targeting four metrics:
- Aligning Medicaid renewals (eligibility redeterminations) with SNAP or TANF renewals, when possible
- Ensuring no more than a 12% Medicaid denial rate per month (in line with federal requirements)
- Maintaining eligibility for the longest possible time for certain vulnerable populations (pregnant women, people who are eligible for both Medicare and Medicaid, children enrolled under the Katie Beckett waiver program, RevMax enrollees, and aged/blind/disabled enrollees)
- A level workload for the Medicaid staff, avoiding spikes in the monthly number of eligibility redeterminations in 2023 or future years.
Georgia Medicaid history and details
Enrollment remains very low in Georgia’s partial Medicaid expansion with a work requirement
In July 2023, Georgia began enrolling people in a partial Medicaid expansion (Georgia Pathways to Coverage), covering adults with household income below the poverty level as long as they work at least 80 hours per month. The coverage takes effect the month after a person’s enrollment is approved.
Georgia Pathways is a complicated, controversial program. Because Georgia hasn’t fully expanded Medicaid, the state is not receiving the enhanced federal funding they would get with full Medicaid expansion. And the bulk of the money that the state has spent on Georgia Pathways has gone to consultants and administrators.8
The Georgia Pathways program currently only has federal authorization through September 2025. The state is accepting public comments (through February 25, 2025) on a waiver extension proposal that would extend the program for another five years. Notably, it would also remove the monthly work reporting requirement for a person to remain covered by Georgia Pathways. It would instead call for the state to ensure that an applicant is working at least 80 hours per month when they initially apply, and at each annual renewal.9 If finalized, this would cut down on the red tape that currently prevents some eligible Georgia residents from obtaining and maintaining coverage under Georgia Pathways.
(The initial approval of the Georgia Pathways program clarifies that if an enrollee complies with the community engagement and reporting requirement for at least six consecutive months, they switch to only having to report changes, if applicable.)
By late 2024, only about 4,900 people were enrolled in Georgia Pathways coverage.7 This had potentially increased to about 6,500 by early 2025.15
But Georgia officials had initially projected that about 64,000 people would gain coverage under Georgia Pathways, which was itself a small fraction of the number who would be newly eligible if Georgia were to accept federal funding to fully expand Medicaid without any strings attached.16
The extremely low enrollment is attributed to the work requirement and associated paperwork, lack of publicity about the program, an enrollment portal that isn’t user-friendly, and staff members who are swamped with redeterminations for current enrollees (as described above).17
The implementation of Georgia’s partial Medicaid expansion has been a complicated legal and regulatory process, and Georgia is the only state in the country with a Medicaid work requirement. Here’s the story of how all of this came to be:
Georgia enacted legislation (SB106) in 2019 that allowed the state to seek federal permission to expand Medicaid, but only to people earning up to 100% of the poverty level (as opposed to 138%, as called for in the ACA).
In November 2019, the state unveiled an 1115 waiver proposal that called for partial Medicaid expansion, effective in July 2021, that would cover adults age 19-64 with income up to the poverty level, as long as they were working (or participating in other “community engagement” activities) at least 80 hours per month.
Georgia’s full proposal can be viewed here. The state sought public comments on the proposal in late 2019, and most who commented did not support it. The state submitted the proposal to CMS in late December 2019, and approval was granted in October 2020. The state’s partial expansion of Medicaid was initially slated to take effect July 1, 2021.
The approved waiver also allowed for Georgia Pathways enrollees with income above 50% of the poverty level to have cost-sharing and monthly premiums (ranging from $7 to $11/month, with a lower additional rate for a spouse, plus a tobacco surcharge if applicable).
Although the Trump administration was open to states’ Medicaid work requirement proposals (and approved Georgia’s), the Biden administration noted that work requirements do not mesh with the overall mission of Medicaid, which is to provide health coverage to low-income Americans. So CMS notified Georgia in February 2021 that the work requirement approval was being reconsidered (CMS sent a similar letter to every state where Medicaid work requirements had been approved by the Trump administration).
In March 2021, Georgia officials replied, explaining that they believe the work requirement is an essential part of their plan to partially expand Medicaid. Shortly thereafter, Georgia also notified CMS that the partial expansion of Medicaid was being delayed until at least the end of 2021, while Georgia and CMS officials worked out the details.
In late 2021, CMS notified Georgia officials that the approval for the work requirement provision had officially been revoked, along with the premium requirement that Georgia had been included in the Georgia Pathways program. At that point, the partial expansion of Medicaid was still allowed to move forward, but without a work requirement or a premium requirement for participants. (The Biden administration also revoked Medicaid work requirement approvals in all of the other states where the Trump administration had approved them.)
In January 2022, the state of Georgia filed a lawsuit against CMS/HHS, alleging an “unlawful regulatory bait and switch” and asking a judge to allow the state to proceed with the Georgia Pathways program as it was initially approved in 2020. In August 2022, a judge sided with Georgia, clearing the way for the state to move forward with the Georgia Pathways program. The Biden administration did not appeal that decision.
Implementation of the state’s partial Medicaid expansion was paused while the lawsuit made its way through the court system. But by late 2022, Georgia Governor Brian Kemp announced that the Pathways program would begin in July 2023. The program, including the work requirement, is being administered via the state’s existing Georgia Gateway website for social services benefits.
The initially approved 1115 waiver for Georgia Pathways was valid through September 2025. Georgia asked the Biden administration to extend this for another three years due to the implementation delays, but CMS notified Georgia in late 2023 that they would not extend the Georgia Pathways demonstration, which is still set to expire at the end of September 202518 (as noted above, Georgia is working towards obtaining a five-year extension in 2025). This was the agency’s second rejection of Georgia’s request to extend the demonstration through 2028.
In February 2024, the state of Georgia filed a lawsuit against CMS over the extension request. The state’s goal with the lawsuit was to obtain an extension to the Georgia Pathways 1115 waiver, allowing it to continue through September 2028.19 But that case was dismissed by a judge, so in early 2025 Georgia was working on an extension proposal that includes some changes to how Georgia Pathways works, including a removal of the monthly work reporting requirement.9
Georgia Pathways: Costly for the state and complicated for enrollees
As part of the waiver proposal, Georgia asked CMS to provide the state with full Medicaid expansion funding (i.e., covering 90% of the cost), even though the state would only be implementing a partial expansion of Medicaid.
A similar request from Utah was rejected by the Trump administration in 2019, and CMS followed the same process for Georgia: The federal government is not providing the 90% funding match for Georgia’s partial Medicaid expansion. Instead, Georgia is continuing to receive its normal federal matching rate of 67%.
This means it’s costing Georgia more to cover the partially expanded Medicaid population than it would if the state were to simply expand Medicaid fully, as called for in the ACA. (But as noted above, enrollment has been exceedingly low thus far.)
In addition to the enhanced federal funding for Medicaid expansion, the American Rescue Plan provides states that newly expand Medicaid with two years of boosted federal Medicaid funding. Georgia would be eligible to receive that if the state were to fully expand Medicaid.
Under the Georgia Pathways program, enrollees must report their community engagement every month. However, the waiver terms note that if they comply with the community engagement requirement (including reporting) for at least six consecutive months, they’ll be exempt from the reporting requirement and will only have to report changes, if applicable. Eligibility will continue to be redetermined annually.
The initially approved Georgia Pathways waiver allowed the state to charge premiums for enrollees with income above 50% of the poverty level. This approval was withdrawn by the Biden administration (along with the work requirement approval), but the state sued and won the right to implement the program as initially approved. The premium payments were slated to take effect in 2024, but the state had not started collecting them by late 2024, and had not indicated any plans to start doing so.20
People deemed eligible for Georgia Pathways who also have access to employer-sponsored health coverage will be required to enroll in the employer-sponsored plan, with financial assistance from the Georgia Medicaid program, if this option is deemed cost-effective for the state.21
For non-disabled, non-pregnant adults who can’t comply with the Georgia Pathways work requirement (and associated reporting requirements), Georgia Medicaid is only available if they are caring for a minor child and have a household income that doesn’t exceed roughly 26% of the poverty level. (Note that this percentage decreases each year as the federal poverty level increases, unless Georgia increases its eligibility limit. This is because Georgia is one of the states that use a flat dollar limit, rather than a percentage of the poverty level, to determine Medicaid eligibility for parents.) For a household of three in 2024 and early 2025, this amounted to about $551 in monthly income.
KFF estimates that 175,000 people in Georgia are in the Medicaid coverage gap,22 which means their household incomes are below the poverty level (so they’re not eligible for subsidies in the exchange) and yet they are not eligible for Medicaid under the state’s current rules.
The state of Georgia only expected about 50,000 people to gain coverage under Georgia Pathways, or possibly as many as 100,000 (and as noted above, enrollment hadn’t even reached 5,000 people by late 2024). But in general, it’s expected that the majority of the people currently in the coverage gap wouldn’t be able to comply with the premiums and/or the work requirement and administrative reporting.
It’s also noteworthy that if Georgia were to fully expand Medicaid as called for in the ACA, the state would be guaranteed to receive 90% federal funding (i.e., no waiver approval necessary), and more than 350,000 people would gain coverage.11
Instead, the state opted to cover only a fraction of those individuals, and they’re forfeiting the enhanced federal funding match that would be provided if they fully expanded Medicaid. Georgia is also forfeiting the American Rescue Plan’s (ARP) two years of additional federal funding for states that newly expand Medicaid, which would amount to $1.3 billion in additional federal funding.
Georgia can reverse course on this at any time. If Medicaid is fully expanded (including under the proposed private option legislation introduced in Georgia’s legislature in January 20255), the enhanced federal funding and the extra ARP funding would be provided by the federal government.
Georgia's history with Medicaid expansion
As of May 2020, 23% of Georgia residents were uninsured — the state had the fourth-highest uninsured rate in the U.S. at that point. Georgia is leaving billions of dollars on the table and hundreds of thousands of people without Medicaid coverage by passing up federal funding to expand Medicaid.
Two laws designed to make expansion difficult were enacted during the 2014 legislative session in Georgia. HB 990 prohibits Medicaid expansion without legislative approval (the 2019 legislation that triggered the Georgia Pathways proposal expressly allows for Medicaid expansion for those earning up to the poverty level), while HB 943 prohibits state and local employees from advocating for Medicaid expansion.
By the spring of 2016, Medicaid expansion began to seem within reach in Georgia, fueled in part by support from hospitals facing severe financial challenges. The state has raised Medicaid reimbursement rates for providers, including OB-GYNs in the state, to keep providers solvent and able to accept Medicaid patients. And Republican lawmakers began indicating that they might be open to a privatized version of Medicaid expansion, like the model used in Arkansas.
Although then-Governor Nathan Deal had long been opposed to Medicaid expansion, he began to express a willingness to consider a modified version of expansion, as did more GOP lawmakers in Georgia. In June 2016, talking about the possibility of Medicaid expansion during the 2017 legislative session, Deal said “I still have the same concerns. And you won’t see anyone advocating a wholesale Medicaid expansion. But I do think there will be variations that will be discussed, and I look forward to talking to members of the General Assembly.”
However, there was no real progress on Medicaid expansion in Georgia until the partial expansion proposal was announced in 2019. Governor Brian Kemp, who took office in 2019, has been steadfastly opposed to full Medicaid expansion, although he views the Georgia Pathways program as a conservative compromise aimed at helping people who are working but not able to afford health coverage.
As of October 2024, total Medicaid/CHIP enrollment in Georgia was 29% higher than it had been in 2013, even though the state has not expanded Medicaid.23 Enrollment had been far higher in early 2023, but hundreds of thousands of Georgia residents were disenrolled from Medicaid during the year-long “unwinding” process after the pandemic emergency period ended.
Georgia Medicaid history
The federal legislation authorizing Medicaid was enacted in 1965, and Georgia implemented its program in October of 1967. The Georgia Medicaid program is managed by the Georgia Department of Community Health (DCH).
A major trend in state Medicaid programs has been the move from fee-for-service to managed care arrangements. In fee-for-service, the doctor, hospital or clinic is reimbursed for each visit, test or procedure performed. In managed care, the health care provider gets a set fee each month for each person covered, regardless of the actual services provided.
Georgia Medicaid first adopted managed care in 1993 and transitioned to a statewide Medicaid managed care system called Georgia Families in 2006. Nearly all Medicaid beneficiaries — including low-income adults and children, foster care children, and pregnant women —must enroll in Georgia Families. However, individuals with disabilities or long-term care needs do not receive services through Georgia Families.
Although Georgia has not expanded Medicaid, enrollment in Medicaid/CHIP in Georgia was still 29% higher in the fall of 2024 than it had been in 2013.23
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Georgia?
Explore more resources for options in GA including ACA coverage, short-term health insurance, dental and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”Medicaid, Children’s Health Insurance Program, & Basic Health Program Eligibility Levels” Centers for Medicare & Medicaid Services. Accessed Feb. 4, 2025 ⤶
- Medicaid, PeachCare for Kids® Postpartum Medical Services Extended. Georgia Department of Community Health. November 2022. ⤶
- Georgia Pathways to coverage. Georgia Department of Community Health. Accessed January 2024. ⤶ ⤶
- ”Georgia HB258” BillTrack50. Accessed Feb. 4, 2025 ⤶
- ”Georgia HB97” and “Georgia SB50” BillTrack50. Accessed Feb. 4, 2025 ⤶ ⤶
- ”GA Code § 49-4-142.2 (2022)” Justia Law. Accessed Feb. 4, 2025 ⤶
- Pathways Monitoring Reports, October 2024. Georgia Department of Community Health. Accessed Feb. 4, 2025 ⤶ ⤶
- ”Georgia’s Much Vaunted Medicaid Waiver “Pathways to Coverage” Has Turned Into “Pathways to Profit” for Consultants” Georgetown University Center for Children and Families. Oct. 30, 2024 ⤶ ⤶
- ”Georgia Pathways to Coverage 1115 Demonstration Waiver Extension Notice” Georgia Department of Community Health. Accessed Feb. 4, 2025 ⤶ ⤶ ⤶
- ”October 2025 Medicaid & CHIP Enrollment Data Highlights” Medicaid.gov, Accessed February 2026 ⤶
- “How Many Uninsured Are in the Coverage Gap and How Many Could be Eligible if All States Adopted the Medicaid Expansion?” KFF.org, Accessed Feb. 4, 2025 ⤶ ⤶
- Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment, KFF.org, Accessed February 2026 ⤶
- Medicaid Enrollment and Unwinding Tracker. KFF. Accessed Feb. 4, 2025 ⤶
- HealthCare.gov Marketplace Medicaid Unwinding Report. Centers for Medicare and Medicaid Services. Data through April 2024. Accessed Feb. 4, 2025 ⤶
- ”Georgia Pathways Data Tracker” Jan. 2, 2025 ⤶
- Medicaid Work Requirements are Back on the Agenda. KFF. April 2023. ⤶
- Georgia offered Medicaid with a work requirement. Few have signed up. Politico. December 2023. ⤶
- Letter from CMS to Georgia. December 2023. ⤶
- State of Georgia vs. CMS. Filed February 2, 2024. ⤶
- ”Georgia’s Pathways to Coverage Program: The First Year in Review” Georgia Budget & Policy Institute. Oct. 29, 2024 ⤶
- ”Georgia Pathways HIPP” Georgia Pathways to Coverage. Accessed Feb. 4, 2025 ⤶
- ”How Many Uninsured Are in the Coverage Gap and How Many Could be Eligible if All States Adopted the Medicaid Expansion?” KFF. Feb. 26, 2024. ⤶
- ”Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment” KFF. October 2024. Accessed Feb. 4, 2025 ⤶ ⤶

