Medicaid eligibility and enrollment in South Dakota

Medicaid expansion took effect July 1, 2023, due to 2022 ballot measure. In 2024, voters approved a work requirement that could be authorized by the legislature and the federal government.

Who is eligible for Medicaid in South Dakota?
Medicaid in South Dakota (also called the South Dakota Medical Assistance Program, which includes both Medicaid and CHIP) is available to eligible low-income households (note that all of these income limits include a built-in 5% income disregard that’s used for MAGI-based Medicaid eligibility):
- Pregnant women with household incomes up to 138% of the federal poverty level (FPL). Postpartum Medicaid coverage for new mothers continues for 12 months after the baby is born (instead of ending after 60 days as it did before mid-2023).1 But this is largely irrelevant now that Medicaid has been expanded to the same income level for all adults under age 65.
- Children aged 0 to 18 with household income up to 187% of FPL are eligible for Medicaid; Children with household incomes up to 209% of poverty are eligible for CHIP (Children’s Health Insurance Program).
- Adults under age 65 are eligible for Medicaid with income up to 138% of the poverty level. This took effect in July 2023, as a result of a ballot measure passed by voters in 2022. In 2024, South Dakota voters approved another ballot measure that will allow the state to impose a work requirement for this population, if allowed by the federal government (details below).
Apply for Medicaid in South Dakota
Apply year round through HealthCare.gov or by phone at 1-800-318-2596. Download applications for Medicaid and CHIP from the South Dakota Department of Social Services website; then mail, fax, or take the application in person to a local Social Services office. Have questions? Call (605) 773-3165.
Eligibility: Pregnant women with household incomes up to 133% of FPL; children with household incomes up to 204% of FPL (for CHIP); parents with dependent children are eligible with incomes up to 58% of FPL.



Medicaid eligibility expanded in July 2023
South Dakota’s legislature and governor rejected the ACA’s expansion of Medicaid for years. But the issue was put to the state’s voters in the 2022 election, and voters approved Medicaid expansion by a 56% to 44% margin. The measure called for the state to expand Medicaid eligibility on July 1, 2023.
South Dakota received federal approval to initiate expansion as of July 2023, and for the specific benefits package that the newly eligible population is receiving. Under the new eligibility guidelines, a single adult qualifies for Medicaid in South Dakota with an income of up to about $20,782 in 2024.2 (Here are the monthly income limits; the numbers increase a little each year to keep pace with the federal poverty level.)
An estimated 52,000 low-income South Dakota residents were initially expected to enroll in Medicaid under the expanded eligibility guidelines. By October 2024, almost a year and half after enrollment in expanded Medicaid began, almost 28,000 people had enrolled.3 This was well below the initial expectations, but the state has revised its projections and now expects about 40,000 Medicaid expansion enrollees by 2025.4 Enrollment in South Dakota
Over the next five years, South Dakota will receive nearly $1.35 billion in additional federal Medicaid funding due to the eligibility expansion.
Medicaid expansion via ballot measure has been successful in all of the states where voters have had an opportunity to directly decide whether the state should expand Medicaid. This includes Maine, Utah, Idaho, Nebraska, Oklahoma, and Missouri.
Voters approve work requirement ballot measure in 2024
In the 2024 election, South Dakota voters approved Amendment F by a 56-44 vote.5 This ballot measure allows the South Dakota legislature to impose a work requirement for the Medicaid expansion population. But a work requirement would also need federal approval, either in the form of federal legislation allowing any state to impose a work requirement, or approval of a state-specific 1115 waiver. During the first Tump administration, 13 states received federal approval for work requirements, although most of them were never implemented.
A typical work requirement would require Medicaid expansion enrollees to work 80 hours per month and report the details to the state in order to maintain eligibility for coverage. Patient advocates note that work requirements can result in people losing Medicaid — despite working the required number of hours — because they aren’t able to navigate the reporting system.
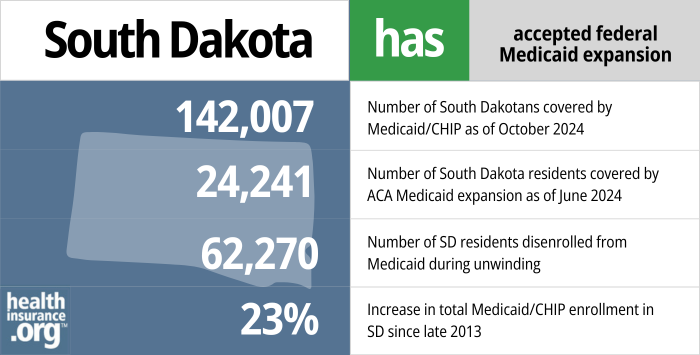
- 142,007 – Number of South Dakotans covered by Medicaid/CHIP as of Oct. 20246
- 24,241 – Number of South Dakota residents covered by ACA Medicaid expansion as of June 20247
- 62,270 – Number of SD residents disenrolled from Medicaid during unwinding8
- 23% – Increase in total Medicaid/CHIP enrollment in SD since late 20139
Explore our other comprehensive guides to coverage in South Dakota

We’ve created this guide to help you understand the South Dakota health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.
Learn about health insurance coverage options in South Dakota.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in South Dakota.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in South Dakota as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.
Learn about short-term insurance regulations in South Dakota.

Frequently asked questions about South Dakota Medicaid
How do I apply for Medicaid in South Dakota?
Medicaid enrollment is open year-round. You can apply for South Dakota Medicaid online, over the phone, or by submitting a paper application. If you have questions, you can reach the SD Department of Social Services at 1-605-773-3165.
- Online: Visit HealthCare.gov to begin the process, or South Dakota DSS online
- By phone: Call HealthCare.gov at 1-800-318-2596 to begin the process (if it looks like you’re eligible for Medicaid, your information will be transferred to South Dakota Medicaid).
- Paper applications: Download an application for Medicaid or CHIP from the South Dakota Department of Social Services website. The application must then be mailed, faxed, or taken in person to a local Social Services office.
How does Medicaid provide financial assistance to Medicare beneficiaries in South Dakota?
Many Medicare beneficiaries receive Medicaid’s help with paying for Medicare premiums, affording prescription drug costs, and covering expenses not covered by Medicare – such as long-term care.
Our guide to financial assistance for Medicare enrollees in South Dakota includes overviews of these benefits, including Medicare Savings Programs, long-term care coverage, and eligibility guidelines for assistance.
How did South Dakota handle Medicaid renewals after the pandemic?
Throughout the COVID pandemic, from March 2020 through March 2023, states were not allowed to disenroll anyone from Medicaid, even if they no longer met the eligibility criteria (some states chose to apply this continuous coverage rule to their CHIP populations as well, but South Dakota did not).
The federal continuous coverage requirement ended March 31, 2023, and states could resume routine disenrollments as early as April 2023. The process of redetermining eligibility for everyone enrolled in Medicaid was referred to as “unwinding,” and it continued until mid-2024. After that, states were back to their normal protocols of redetermining eligibility for each enrollee at least once per year.
South Dakota opted to begin the return to normal eligibility redeterminations and disenrollments as soon as allowed under federal rules, with renewal processing beginning in February 2023 and disenrollments possible as of April 1 (only four other states opted to have their initial round of disenrollments effective in April).
According to South Dakota’s enrollment data page and the KFF unwinding tracker, almost 63,000 people were disenrolled from Medicaid in South Dakota during the unwinding process. Enrollment had stood at just under 135,000 in March 2023. It dropped as low as 121,000 in mid-2023, but then started to climb again once Medicaid expansion took effect in July 2023. By late 2024, there were almost 147,000 people enrolled in South Dakota Medicaid.10
South Dakota was in a unique position during the unwinding process, as Medicaid expansion took effect in the state in July 2023, just three months after the first round of disenrollments due to the end of the COVID-related continuous coverage rule. Some people who lost Medicaid in April, May, or June 2023 found that they were once again eligible for Medicaid starting in July, under the new expansion rules (for those whose renewal date is July or later, they would not lose coverage in that case, but would simply transition to the Medicaid expansion eligibility category). So for those individuals, the state was screening for potential eligibility under the expansion guidelines and letting the person know that they should reapply starting in June (for coverage effective July 1). Reminder notices about this were sent to these individuals in June 2023.
People who are no longer eligible for Medicaid will generally find that they can either enroll in an employer’s plan (if available), or sign up for a plan through the South Dakota Marketplace/exchange. Most exchange enrollees qualify for substantial income-based subsidies to offset the cost of their coverage (and in some cases, their out-of-pocket costs).
HealthCare.gov offered an extended special enrollment period for people who lost Medicaid during the unwinding period; it continues through November 30, 2024.11
Does South Dakota have a Medicaid work requirement?
No, although that could change in the future.
As noted above, South Dakota voters approved Amendment F in the 2024 election, which would allow the state legislature to create a work requirement for the Medicaid expansion population.5 This would also require federal approval. And although the Biden administration has rescinded previously-approved Medicaid work requirements, the first Tump administration approved Medicaid work requirement waivers in 13 states. So the second Trump administration is likely to be more open to work requirement proposals than the Biden administration was.
In 2018, long before Medicaid was expanded in South Dakota, the state sought federal approval for a pilot program work requirement for low-income parents in the existing Medicaid program (the pilot program would have applied in just two counties initially).
Former Governor Dennis Daugaard laid out the details of the work requirement in his State of the State address in January 2018, and the state published the proposed waiver application in May 2018. The waiver proposal has been pending CMS approval since 2018, but the Biden administration notified states in 2021 that Medicaid work requirements were essentially a non-starter; all of the previously approved work requirements were revoked by the Biden administration in 2021, and no pending work requirement proposals have been approved. South Dakota began voluntary enrollment in the Career Connector program in July 2018.
South Dakota Medicaid history and details
South Dakota Medicaid history
South Dakota’s Medicaid program became effective in October 1967, nearly two years after Medicaid was created.
For many states, 2014 represented a significant shift in eligibility, particularly for childless adults. However, South Dakota Medicaid eligibility guidelines did not change under the ACA until mid-2023, when the ACA’s Medicaid expansion took effect following voter approval of a ballot measure to do so.
South Dakota Medicaid expansion history
South Dakota expanded Medicaid in July 2023, nearly a decade after Medicaid expansion took effect in many other states. Former Governor Dennis Daugaard supported Medicaid expansion by 2015 (after initially opposing it), but the issue did not have lawmakers’ support.
Current Governor Kristi Noem was opposed to Medicaid expansion, and the legislature had repeatedly rejected Medicaid expansion. But as has been the case in every other state where voters got to weigh in directly on the issue, South Dakota voters approved a constitutional amendment (Amendment D) to expand Medicaid eligibility as called for in the ACA.
South Dakota officials announced in September 2015 that their proposal to expand Medicaid had received “an initial go-ahead” from HHS. then-Governor Dennis Daugaard’s senior advisor Kim Malsam-Rysdon noted that the plan was still preliminary, but it appeared promising and would have expanded eligibility to far more people than the state’s 2014 proposal, which would only have expanded coverage to residents with incomes below the poverty level (HHS rejected that proposal, as Medicaid expansion capped at the poverty level — but with the enhanced federal Medicaid expansion funding match — was a non-starter under the Obama administration, and was also rejected by the Trump administration when proposed by Utah and Georgia).
Although states that expanded Medicaid are paying 10% of the cost, Daugaard noted that his proposal would have ended up being a financial net positive for the state. That’s because he was working with the federal government and Native American tribal leaders to use Medicaid funding for Native Americans who would become eligible for expanded Medicaid and who receive treatment outside of Indian Health Services (IHS) facilities. Those costs are covered in part by the state, and Daugaard said that South Dakota would save more there than it would spend on its portion of the Medicaid expansion costs. Daugaard said that he wouldn’t continue his push for Medicaid expansion if it ended up needing additional money from the state’s general fund.
In December 2015, Governor Daugaard explained the details of his $4.8 billion budget proposal, including his proposal to expand Medicaid to cover 55,000 people who weren’t currently eligible. Daugaard said that the state should “seize the opportunity” to use federal funding to expand coverage, if possible.
In February 2016, HHS agreed to establish arrangements under which non-IHS providers could enter into “care coordination agreements” with IHS facilities, and Native Americans enrolled in Medicaid would be able to receive care at those non-IHS facilities and the full cost would be covered by federal Medicaid funds (as opposed to the state paying a portion and the federal government paying a portion). But Daugaard noted that the practical implementation of the new HHS provision could be complicated, and that there was still work to be done to determine whether the savings from the new IHS rule would save enough money to make Medicaid expansion budget-neutral in South Dakota.
A few days later, Daugaard said that it was too late in the 2016 legislative session to get the ball rolling on Medicaid expansion, and said that he would remove Medicaid expansion from his proposed budget. He indicated that a special session was a possibility, but that waiting until the 2017 legislative session was also a possibility. In June 2016, Daugaard confirmed that the issue would have to wait until the 2017 legislative session, as he was opting not to call a special session in 2016.
In early 2017, in his State of the State address, Daugaard noted that he was optimistic about working with the Trump administration to ensure that the federal government would begin to fully fund medical care for Native Americans, regardless of where the care was provided, without requiring “health care providers to jump through several hoops,” as he believed the Obama-era arrangement did. He did not mention Medicaid expansion in that address.
The issue of Medicaid expansion was essentially off the table in South Dakota as of early 2017. The coalition tasked with recommending how the state should expand coverage updated their conclusions in December 2016 to note that Governor Daugaard was no longer recommending Medicaid expansion for 2017, in light of the incoming Trump administration’s plans to overhaul Medicaid nationwide with block grants or per-capita allotments. Ultimately, that did not come to pass at the federal level, but no progress was made toward Medicaid expansion in South Dakota in the meantime.
Kristi Noem took office as governor in 2019, and opposed Medicaid expansion. But voters in the state had an opportunity to decide the matter for themselves on the 2022 ballot, and they approved Medicaid expansion. Most of the states that have expanded Medicaid have done so via legislation, but South Dakota is one of several where the issue has been decided by voters instead.
To get the measure on the ballot, Medicaid expansion supporters in South Dakota gathered more than 38,000 signatures. There were concerns that the measure might need 60% approval to pass, as voters also had the opportunity to vote on South Dakota Constitutional Amendment C in the June 2022 primary election. That measure was defeated, but if it had been approved it would have required 60% voter approval for future ballot measures that increased taxes or require the state to appropriate more than $10 million. If voters had approved Amendment C, Amendment D would have needed to be approved by at least 60% of voters to pass. But since Amendment C did not pass, Amendment D only needed a simple majority to pass (it ultimately got 56% of the vote).
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in South Dakota?
Explore more resources for options in South Dakota including ACA coverage, short-term health insurance, dental insurance and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”Medicaid After Pregnancy: State-Level Implications of Extending Postpartum Coverage (2023 Update) ” ASPE. Apr. 7, 2023 ⤶
- ”2024 Poverty Guidelines” U.S. Department of Health & Human Services. Accessed July 16, 2024 ⤶
- ”DSS Statistical Information” (Expansion population accounts for 19% of 146,921 total enrollees). South Dakota Department of Social Services. Nov. 8, 2024 ⤶
- ”Medicaid expansion enrollment ‘slow & steady’ as state launches application portal” South Dakota Searchlight. April 17, 2024 ⤶
- ”South Dakota Constitutional Amendment F, Medicaid Work Requirement Amendment (2024)” BallotPedia. Accessed Nov. 22, 2024 ⤶ ⤶
- ”October 2024 Medicaid & CHIP Enrollment Data Highlights” Medicaid.gov, Accessed January 2025 ⤶
- ”Medicaid expansion enrollment ‘slow & steady’ as state launches application portal” Medicaid.gov, Accessed February 2025 ⤶
- “Medicaid Enrollment and Unwinding Tracker”, KFF.org, Accessed January 2025 ⤶
- ”Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment” KFF.org, Accessed February 2025 ⤶
- ”DSS Statistical Information” South Dakota Department of Social Services. Accessed Nov. 22, 2024 ⤶
- ”HHS Takes Additional Actions to Help People Stay Covered During Medicaid and CHIP Renewals” CMS Newsroom. Mar. 28, 2024 ⤶

