Medicaid eligibility and enrollment in Vermont

Medicaid/CHIP enrollment in Vermont is lower now than it was pre-ACA. That’s because Vermont had already expanded Medicaid two decades before the ACA.

Who is eligible for Medicaid in Vermont?
Vermont’s Medicaid program is called Green Mountain Care, and the program for children and pregnant women is called Dr. Dynasaur. In Vermont, income-based Medicaid is available to the following populations (these limits include a built-in 5% income disregard that’s used for income-based Medicaid eligibility): 1
- Adults with incomes up to 138% of the federal poverty level (FPL)
- Children with household incomes up to 317% of FPL (combination of Medicaid and CHIP/Dr. Dynasaur; premiums are charged if household income is above 138% FPL;2 coverage is available through IHIP if the child would be eligible for Medicaid but isn’t due to immigration status)3
- Pregnant women with incomes up to 213% of FPL (coverage for the mother continues for 12 months after the baby is born;4 coverage is available through IHIP if the pregnant woman would be eligible for Medicaid except for immigration status)3
Legislation was considered in Vermont in 2024 that would have extended Dr. Dynasaur coverage to young adults up to age 26, and gradually expanded Medicaid for adults until it reached, by 2030, the income limits used for Dr. Dynasaur. It would have also increased the income limits for Vermont’s Medicare Savings Programs. The measure passed in Vermont’s House, but died in the Senate.5
Older adults or individuals who are blind or disabled may also qualify for Medicaid in Vermont. See the Medicaid for the Aged, Blind and Disabled (MABD) page on the Green Mountain Care website for more information.
Apply for Medicaid in Vermont
Apply for Green Mountain Care and Dr. Dynasaur through Vermont Health Connect.
Eligibility: Adults with incomes up to 138% of FPL; children with household incomes up to 312% of FPL; pregnant women with incomes up to 208% of FPL.



ACA’s Medicaid eligibility expansion in Vermont
Vermont has fully embraced the Affordable Care Act (ACA), including the expansion of Medicaid starting in 2014. But while the state’s uninsured rate is among the lowest in the country, Medicaid/CHIP enrollment was slightly lower in late 2024 than it had been in late 2013, before Medicaid expansion took effect (nationwide, Medicaid enrollment was up 38% at that point,6 after increasing sharply during the COVID pandemic and then declining once post-pandemic Medicaid disenrollments resumed).
This is because Vermont had already addressed the issue of health insurance for low-income residents, nearly two decades earlier. So although the state was quick to accept federal funding for Medicaid expansion as called for in the ACA, the uninsured rate among low-income residents was already well below the national average — only 7.2% according to U.S. Census data. By 2014, it had fallen to 5%, and by 2016, it had dropped even lower, to 3.7% — only Massachusetts and Hawaii had lower uninsured rates at that point.
In 1995, the Vermont legislature authorized the creation of Vermont Health Access Plan (VHAP) and Dr. Dynasaur, which is still utilized to provide coverage to children and pregnant women. In addition, the state created Catamount Health in 2006, which allowed residents with incomes up to 300% of poverty to purchase a Catamount plan (provided by either MVP Health or Blue Cross Blue Shield) at a subsidized rate.7
Catamount and VHAP were scheduled to end on December 31, 2013, with all the individuals they covered switching to either expanded Medicaid or a subsidized private plan through the exchange. But because of Vermont Health Connect’s rocky rollout, then-Governor Shumlin extended Catamount and VHAP until March 31, 2014 for any residents who were still enrolled in those plans.
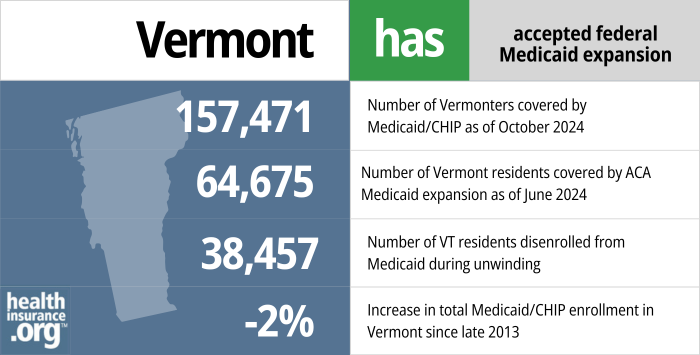
- 157,471 – Number of Vermonters covered by Medicaid/CHIP as of October 20248
- 64,675 – Number of Vermonters covered by ACA Medicaid expansion as of June 20249
- 38,457 – Number of VT residents disenrolled from Medicaid during unwinding10
- -2% – Increase in total Medicaid/CHIP enrollment in Vermont since late 201311
Explore our other comprehensive guides to coverage in Vermont

We’ve created this guide to help you understand the Vermont health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Vermont.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Vermont as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.

Frequently asked questions about Vermont Medicaid
How do I apply for Medicaid in Vermont?
If you’re under 65 and don’t have Medicare, you can apply for Green Mountain Care or Dr. Dynasaur through the state-run health insurance exchange, Vermont Health Connect. If you’re 65 or older or have Medicare, use this website to apply for Medicaid.
If you have questions, you can call the Vermont Medicaid office for assistance at 1-800-250-8427.
How does Medicaid provide financial assistance to Medicare beneficiaries in Vermont?
Many Medicare beneficiaries receive Medicaid’s help with paying for Medicare premiums, affording prescription drug costs, and covering expenses not reimbursed by Medicare – such as long-term care.
Our guide to financial assistance for Medicare enrollees in Vermont includes overviews of these benefits, including Medicare Savings Programs, long-term care coverage, and eligibility guidelines for assistance.
How many Vermont residents were disenrolled from Medicaid after the pandemic?
Due to the COVID pandemic, Medicaid disenrollments were paused nationwide from March 2020 to March 2023. States had to resume regular eligibility redeterminations in February, March, or April 2023, and disenrollments could resume as early as April 1, 2023. States then had a one-year “unwinding” period during which they had to initiate eligibility redeterminations for everyone enrolled in Medicaid.
Vermont began the unwinding process in April 2023, and finished it in May 2024.12
38,457 Vermont residents were disenrolled from Medicaid/CHIP during the unwinding process.10
Some of these residents transitioned to an employer-sponsored health plan, and some likely became uninsured. But more than 5,700 transitioned to a private plan offered through Vermont Health Connect, the state’s health insurance Marketplace.13
In the initial months of the unwinding period, Vermont prioritized renewals for people who reported changes during the pandemic that would make them ineligible for Medicaid (for example, an increase in income) or who aged out of a coverage category (for example, turning 19 or 65). They also prioritized renewals for medically needy enrollees with spend-downs (ie, their income is too high for Medicaid eligibility, but they qualify when their medical bills are subtracted from their income).
Vermont Medicaid History
Why hasn't Medicaid enrollment grown in Vermont since ACA expansion took effect?
Vermont’s Medicaid enrollment grew by 11% from late 2013 to mid-2016 (and had peaked in early 2016), but enrollment declined after that, likely due to the state’s improved eligibility verification process.
As was the case nationwide, Medicaid enrollment grew in Vermont during the COVID pandemic, but declined after disenrollments resumed in mid-2023.
By late 2024, Medicaid/CHIP enrollment in Vermont stood at 157,471 people, which was 2% lower than it had been in 2013.11
Nationwide, Medicaid/CHIP enrollment was 38% higher in late 2024 than it had been in 2013, despite the millions of people who had been disenrolled after the pandemic emergency period ended.
The only other states where Medicaid/CHIP enrollment was lower in 2024 than it had been in 2013 were Wyoming, Mississippi, and Texas,11 none of which had expanded Medicaid under the ACA.
Although Vermont implemented the ACA’s Medicaid expansion — which covered nearly 65,000 residents as of mid-20249 — the reason it hasn’t resulted in enrollment growth is because Vermont had already expanded Medicaid (beyond the income limits the ACA later adopted) in the mid-90s.7 So although Vermont was able to start utilizing the ACA’s enhanced federal funding for adult coverage, those people were already eligible for Medicaid in Vermont before the ACA.
Vermont's All-Payer ACO Model
Vermont has long been a vanguard when it comes to healthcare reform. And although the state abandoned its push for a single-payer system in late 2014, officials moved forward with their plans for an all-payer model that would merge payments from Medicaid, Medicare, and commercial insurers, paying set rates to all providers in the state via what would essentially be one big accountable care organization.
In September 2016, Vermont received tentative approval from CMS for the waiver that would be needed to coordinate Medicare (which is a federal program) into the all-payer model. In 2017, the state began a pilot program in which 30,000 of Vermont’s 151,000 Medicaid enrollees were covered under the OneCare network of 2,000 providers, with the state paying $93 million to the network for the global care. In 2018, the state tested a program that includes Medicaid, Medicare, and commercially insured patients, with nine of the state’s 14 hospitals participating in the OneCare program, providing care for about 120,000 Vermont residents.
The All-Payer Accountable Care Organization Model Agreement was initially approved from 2018-2022. It is scheduled to sunset at the end of 2025.14
Medicaid spending drove budget shortfall in the teens; Eligibility redeterminations reduced Vermont Medicaid enrollment
Vermont’s budget was expected to have a $58.5 million shortfall in fiscal year (FY) 2017, which started in July 2016. That was the ninth year in a row that the state’s spending outpaced revenue, and the budget shortfall issue continued into FY 2019. In 2020, there was a hole of nearly $200 million in the year’s state budget, largely due to the COVID-19 pandemic. But the federal coronavirus relief money contributed to a positive budget address from Governor Scott in January 2021.
About $53 million of the projected FY 2017 shortfall was attributed to Medicaid spending, and $36 million of the 2016 fiscal year’s $40 million shortfall was due to Medicaid spending. The federal government paid the full cost of expansion through the end of 2016, but the state had to begin paying 5% of the cost of covering the newly eligible population starting in 2017, and 6% in 2018. In addition, the outreach and enrollment efforts in every state have resulted in people enrolling for the first time in Medicaid despite the fact that they already qualified under the pre-ACA eligibility guidelines. For this population, the states are on the hook for their normal funding split with the federal government.
Former Governor Shumlin proposed a payroll tax in January 2015 (0.7%) to provide additional funding for Medicaid, but lawmakers balked at the idea.
In an effort to rein in spending, Vermont’s Medicaid program began going through eligibility redeterminations for existing enrollees starting in October 2015. Roughly a third of Vermont’s population was on Medicaid, and officials believed that some were not actually eligible for the coverage. As a result of the eligibility redeterminations, the state determined that some young adults had been incorrectly enrolled in Dr. Dynasaur rather than expanded Medicaid (which was fully funded by the federal government through 2016 and 90% funded by the federal government in 2020 and future years) or individual market coverage with subsidies through the exchange.
Eligibility redeterminations played a key role in shrinking total Medicaid/CHIP enrollment back to nearly what it was before Medicaid expansion took effect. Total enrollment was only 1% higher at the end of 2017 than it had been at the end of 2013 (nationwide, it was up 29% at that point). As of October 2024, after the post-pandemic Medicaid unwinding period was over, Vermont’s Medicaid enrollment was only 7% higher than it had been in 2013. Nationwide, Medicaid enrollment was 49% higher at that p% lower than it had been in 2013.15
Vermont Medicaid enrollment numbers
According to CMS, there were 157,471 Vermont residents enrolled in Medicaid/CHIP as of October 2024.16
Throughout 2014 and 2015, technical problems with Vermont Health Connect, the state’s exchange, made it impossible to accurately verify eligibility when renewing Medicaid coverage. So the state obtained a waiver from the federal government that allowed them to automatically renew Medicaid coverage without verifying eligibility. But by 2016, the state was able to accurately verify eligibility for Medicaid and stopped automatically reenrolling people
By the end of 2017, total Medicaid/CHIP enrollment in Vermont stood at 162,593, following more than a year of eligibility redeterminations to verify that everyone in the program was eligible to remain in it. This was only 1% higher than enrollment had been in late 2013, before Medicaid expansion took effect.
Total Vermont Medicaid enrollment (including CHIP) had grown to more than 192,000 as of late 2022. That was a 19% increase from 2013, due primarily to the COVID pandemic and the resulting pause on eligibility redeterminations nationwide. But by late 2024, after the unwinding process was completed, Medicaid/CHIP enrollment in Vermont was slightly lower than it had been in 2013.17
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Vermont?
Explore more resources for options in Vermont including ACA coverage, short-term health insurance, dental insurance and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”Medicaid, Children’s Health Insurance Program, & Basic Health Program Eligibility Levels” Centers for Medicare & Medicaid Services. December 2023. ⤶
- ”Medicaid and Dr. Dynasaur” Department of Vermont Health Access. Accessed March 19, 2024. ⤶
- ”Immigrant Health Insurance Plan (IHIP)” Department of Vermont Health Access. Accessed March 19, 2024. ⤶ ⤶
- ”Vermont Medicaid Postpartum Eligibility Expansion” State of Vermont, Agency of Human Services. Mar. 27, 2023 ⤶
- ”Vermont H721” BillTrack50. Dead, May 10, 2024. ⤶
- ”Total October 2024 Medicaid & CHIP Enrollment and Pre-ACA Enrollment” KFF. Accessed March 19, 2023. ⤶
- ”Global Commitment to Health, Annual Report” State of Vermont, Agency of Human Services. Apr. 1, 2015. Accessed Feb. 11, 2025 ⤶ ⤶
- “October 2024 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed Feb. 11, 2025 ⤶
- “Medicaid Enrollment – New Adult Group” Medicaid.gov. Dec. 11, 2024 ⤶ ⤶
- ”Medicaid Enrollment and Unwinding Tracker — Archived Vermont data” KFF.org. Jan. 31, 2025 ⤶ ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed Feb. 11, 2025 ⤶ ⤶ ⤶
- ”Medicaid Renewals Restart” Department of Vermont Health Access. Accessed Feb. 11, 2025 ⤶
- ”State-based Marketplace (SBM) Medicaid Unwinding Report” Centers for Medicare & Medicaid Services. Accessed Feb. 11, 2025 ⤶
- ”Vermont All-Payer ACO Model” CMS.gov. Accessed Feb. 11, 2025 ⤶
- “Total October 2024 Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed Feb. 11, 2025 ⤶
- “October 2024 Medicaid & CHIP Enrollment Data Highlights” Medicaid.gov, Accessed Feb. 11, 2025 ⤶
- “Total November 2023 Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed March 19, 2024. ⤶

