Medicaid eligibility and enrollment in West Virginia

More than 208,000 people were disenrolled from WV Medicaid during the unwinding process

Who is eligible for Medicaid in West Virginia?
West Virginia Medicaid is available to the following legally present residents (there’s a five-year waiting period before new immigrants can enroll in Medicaid/CHIP), in addition to the aged, blind, and disabled (note that the following income limits include a built-in 5% income disregard that’s used for MAGI-based Medicaid eligibility determinations).1
- Infants aged 0 to 1 in households with income up to 163% of the federal poverty level (FPL)
- Children aged 1-5 in households with income up to 146% of FPL
- Children aged 6-18 in households with income up to 138% of FPL
- Children with household income above those levels, up to 300% FPL, are eligible for CHIP in West Virginia
- Pregnant women with income up to 190% of poverty (CHIP is available to pregnant women with income up to 300% of the poverty level). Postpartum Medicaid/CHIP for the mother continues for 12 months after the baby is born.
- Adults with incomes up to 138% of FPL (due to the ACA’s expansion of Medicaid)
- Pregnant women and children in households with up to 300% of FPL qualify for CHIP in West Virginia (different coverage levels are available depending on income).
Apply for Medicaid in West Virginia
Apply through HealthCare.gov or by calling 1-800-318-2596 (24 hours a day).
Eligibility: The aged, blind, and disabled. Also, adults with incomes up to 138% of FPL; children with household incomes up to 300% of FPL are eligible CHIP; pregnant women with incomes up to 158% of FPL.



ACA’s Medicaid eligibility expansion in West Virginia
West Virginia’s leaders opted to expand Medicaid under the Affordable Care Act (ACA) starting on January 1, 2014. Under the expanded eligibility guidelines, adults aged 19-64 are eligible for Medicaid with a household income up to 138% of the poverty level. For a single adult in 2025, that amounts to $21,597 in total annual income2 (Medicaid eligibility can also be determined based on current monthly income).
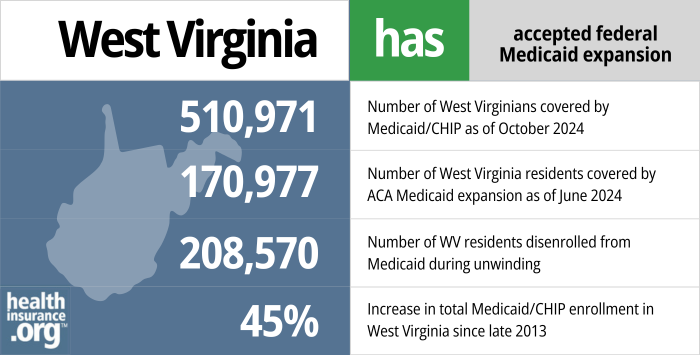
Between 2013 (before Medicaid expansion) and late 2024, West Virginia’s total Medicaid population grew by 44%3 (enrollment had been quite a bit higher during the pandemic, peaking in mid-2023, but declined during the “unwinding” of the pandemic-era continuous coverage rule; this is discussed in more detail below). More than 510,000 people were enrolled in Medicaid and CHIP in West Virginia as of late 2024.4
- 510,971 – Number of West Virginians covered by Medicaid/CHIP as of October 20245
- 170,977– Number of West Virginia residents covered by ACA Medicaid expansion as of June 20246
- 208,570 – Number of WV residents disenrolled from Medicaid during unwinding period7
- 45% – Increase in total Medicaid/CHIP enrollment in West Virginia since late 20138
Explore our other comprehensive guides to coverage in West Virginia

We’ve created this guide to help you understand the West Virginia health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.
Learn about health insurance coverage options in West Virginia.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in West Virginia.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in West Virginia as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.
Learn about short-term insurance regulations in West Virginia.

Frequently asked questions about West Virginia Medicaid
How do I enroll in Medicaid in West Virginia?
You can apply for West Virginia Medicaid online via a West Virginia website that can also provide SNAP and cash assistance programs for eligible residents.
You can also begin the application process through the federally-run exchange by visiting HealthCare.gov or calling 1-800-318-2596 24 hours a day. If it appears that you’re eligible for Medicaid, HealthCare.gov will send your information to West Virginia Medicaid and they will contact you about enrollment.[efn_note]”Medicaid & CHIP” HealthCare.gov. Accessed June 26, 2024[/efn_note]
Medicaid enrollment is year-round. There is no specific time frame during which applications must be completed.
How does Medicaid provide financial help to Medicare beneficiaries in West Virginia?
Many Medicare beneficiaries receive assistance from Medicaid with Medicare premiums, prescription drug costs, and expenses not covered by Medicare – including long-term care.
Our guide to financial assistance for Medicare enrollees in West Virginia includes overviews of these benefits, including Medicaid long-term care coverage, Medicare Savings Programs, and eligibility guidelines for assistance.
How many West Virginia residents were disenrolled from Medicaid after the pandemic?
The federal COVID-related continuous coverage rule for Medicaid was in effect for three years, from March 2020 through March 2023. This ended March 31, 2023, and states began disenrolling people from Medicaid at that point, during a process referred to as “unwinding.”
West Virginia’s first round of disenrollments came in April 2023. In April 2024, West Virginia reported that they had completed the unwinding process. At that point, coverage had been renewed for 279,952 people, while 207,674 people had been disenrolled.7
Most of the people who lost Medicaid are eligible for employer-sponsored health coverage or for a subsidized plan through the West Virginia exchange/marketplace (HealthCare.gov). CMS reported that nearly 29,000 West Virginia residents transitioned from Medicaid to a Marketplace plan during the unwinding period.9
West Virginia officials also noted that CHIP enrollment increased during the unwinding period, due to more than 6,000 children transitioning from Medicaid to CHIP.7
(West Virginia continued to process eligibility redeterminations throughout the pandemic, but did not disenroll anyone who was no longer eligible or who didn’t respond to the renewal notice. So the renewal notices that went out starting in February 2023 were the first that could result in disenrollment since before the pandemic.)
West Virginia Medicaid details and history
West Virginia lawmakers continue to reject Medicaid buy-in and Basic Health Program
In 2023 and again in 2024, legislation was introduced in West Virginia to create a Basic Health Program (available to people ineligible for Medicaid but with income up to 200% of the poverty level) and possibly a Medicaid buy-in program that would allow people to purchase Medicaid coverage if they don’t meet the income guidelines for the program.
But the legislation did not succeed. The 2023 bills were H.B.3274, which passed in the House but did not advance in the Senate, and S.B.610. The 2024 legislation was H.B.5580, which did not advance.
West Virginia CHIP expanded to include pregnant women; postpartum Medicaid/CHIP coverage extended to 12 months
SB564 was signed into law in West Virginia in 2019. The legislation called for CHIP coverage in West Virginia to be expanded to include pregnant women. CHIP eligibility for kids in West Virginia already extended to households with income up to 300% of the poverty level, and that’s the same level that now applies to pregnant women as well. The new CHIP coverage for pregnant women took effect on July 1, 2019 in West Virginia.
Only five other states (Colorado, Missouri, New Jersey, Rhode Island, and Virginia) provide CHIP coverage to pregnant women, but there are numerous states with fairly high income limits for pregnant women to qualify for Medicaid (for example, Medicaid coverage is available to pregnant women in Iowa with household income as high as 375% of the poverty level; in DC, it’s 318%).1
And starting in 2022, West Virginia extended postpartum Medicaid/CHIP coverage to 12 months, so a person who is pregnant and covered under Medicaid or CHIP can keep that coverage for 12 months after giving birth, instead of having their coverage end 60 days post-birth. The American Rescue Plan provided additional federal funding for states to extend postpartum Medicaid coverage to 12 months (that was temporary, but the Consolidated Appropriations Act enacted in late 2022 made it permanent) and most states have chosen to do so.10
West Virginia considered a Medicaid work requirement
As of late 2017, West Virginia’s Department of Health and Human Resources was considering the possibility of seeking a waiver from the federal government in order to implement a work requirement for the state’s Medicaid expansion population. Legislation (HB3136) to create a work requirement was considered in the 2019 legislative session, but it was criticized by consumer advocates and did not advance to a vote.
Although work requirements were a non-starter with the Obama administration, the first Trump administration approved them in several states. But the work requirements were either overturned by judges or suspended due to the COVID pandemic, and all of the approved work requirement waivers were revoked by the Biden administration.
However, the second Trump administration and Congressional Republicans have rekindled the idea of Medicaid work requirements. So they could start to be approved again on a state-by-state basis, or potentially implemented at the federal level.11
Medicaid expansion helping to combat opioid crisis
The opioid crisis has hit West Virginia particularly hard, and the state has the nation’s highest drug overdose death rate. About 22,000 people covered under expanded Medicaid had received treatment for mental health and substance abuse disorders by early 2017. Without Medicaid expansion, most of those people would have been uninsured and unable to access treatment.12
Previous and current governor support Medicaid expansion
West Virginia’s former Governor, Earl Ray Tomblin, was instrumental in West Virginia’s acceptance of Medicaid expansion but was term-limited and could not seek re-election in 2016.
Governor Jim Justice took office in January 2017. He campaigned and was elected as a Democrat, but in the summer of 2017, during his first year in office, he switched to the Republican party. Justice reiterated his support for Medicaid expansion in the weeks leading up to his party switch, stating in late June 2017 that it would be “beyond catastrophic” if the people who had gained coverage under Medicaid expansion were to lose it. But Justice also vetoed a supplemental appropriation for the state’s Medicaid program in 2019, saying that the Medicaid program already had enough funding.
Substantial impact on uninsured rate
Expansion of Medicaid has played a primary role in West Virginia’s sharp reduction in the uninsured rate. According to a 2014 Gallup survey, West Virginia had the sixth-highest drop in uninsured rate during the first half of 2014, due primarily to Medicaid expansion.
According to U.S. Census data, the state’s uninsured rate was 14% in 2013, and had fallen to 5.3% by 2016. It had increased to 6.7% by 2019, however, mirroring the nationwide trend of increasing uninsured rates under the first Trump administration.
But the uninsured rate began to decrease again in subsequent years,13 and was under 6% by 2022.14
West Virginia’s uninsured rate had been similar to the U.S. average (14.5%) in 2013, but the state’s uninsured rate has since been consistently below the national average. West Virginia’s better-than-average performance in reducing the uninsured rate was due in large part to the expansion of Medicaid.
West Virginia Medicaid enrollment numbers
As of mid-2024, about 522,000 people were enrolled in Medicaid in West Virginia, including almost 171,000 people who were covered due to the ACA’s expansion of Medicaid.6
Uncompensated care costs decline sharply
According to data compiled by West Virginians for Affordable Health Care, hospitals in West Virginia saw a 40% decline in uncompensated care costs from 2013 to 2014, thanks in large part to Medicaid expansion that resulted in far fewer uninsured residents in the state.
But although the hospitals acknowledge that their uncompensated care and charity care costs have declined significantly, some also note that Medicaid reimbursements are less than the cost of providing care, and that their losses on Medicaid volume are offsetting the improvements they’ve seen in uncompensated care.
West Virginia’s Medicaid expansion history
West Virginia had initially considered setting up a state-run exchange/Marketplace, but later opted for a partnership exchange, citing cost as one of the reasons for avoiding a fully state-run exchange.
State leaders have said that given the choice between a state-run exchange and Medicaid expansion, the latter seemed like it would provide more bang for the buck.
In May 2013, then-Governor Earl Ray Tomblin announced that West Virginia would proceed with Medicaid expansion. Enrollment for newly-eligible residents began on October 1, 2013, with coverage effective January 1, 2014.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in West Virginia?
Explore more resources for options in West Virginia including ACA coverage, short-term health insurance, dental insurance and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”Medicaid, Children’s Health Insurance Program, & Basic Health Program Eligibility Levels” Centers for Medicare & Medicaid Services. December 2023. ⤶ ⤶
- ”2025 Poverty Guidelines: 48 Contiguous States” U.S. Department of Health and Human Services, Assistant Secretary for Planning and Evaluation. Accessed June 26, 2024 ⤶
- ”Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment” KFF.org. Accessed June 26, 2024. ⤶
- “October 2024 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed Feb. 12, 2025 ⤶
- “October 2024 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed January 2025 ⤶
- “Medicaid Enrollment – New Adult Group”, data.medicaid.gov, Accessed February 2025 ⤶ ⤶
- ”West Virginia Department of Human Services Provides Update on Completion of Medicaid Unwinding” West Virginia Department of Health. April 23, 2024 ⤶ ⤶ ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed January 2025 ⤶
- ”HealthCare.gov Marketplace Medicaid Unwinding Report” Centers for Medicare & Medicaid Services. Data through November 2023. ⤶
- ”Medicaid Postpartum Coverage Extension Tracker” KFF.org. May 10, 2024 ⤶
- ”Medicaid Work Requirements Could Put 36 Million People at Risk of Losing Health Coverage” Center on Budget and Policy Priorities. Feb. 5, 2025 ⤶
- ”A Public Health Emergency:
West Virginia’s Efforts to Curb the Opioid Crisis” Congress.gov. Jan. 14, 2020 ⤶ - ”Health Insurance Coverage Status and Type by Geography: 2021 and 2022” U.S. Census Bureau. Sep. 14, 2023 ⤶
- ”West Virginia, Sources of Insurance Coverage” Georgetown University Center on Health Insurance Reforms. 2022 data. ⤶

