Medicaid eligibility and enrollment in New Jersey

NJ FamilyCare expanded to cover undocumented immigrant children as of 2023

Who is eligible for Medicaid in New Jersey?
In addition to the aged, blind, and disabled, the following New Jersey residents are eligible for Medicaid (NJ FamilyCare):
- Adults under age 65 with incomes up to 138% of poverty (due to the ACA’s expansion of Medicaid).
- Children with household incomes up to 350% of poverty are eligible for CHIP in New Jersey. This is one of the most generous thresholds in the country. And as of 2023, NJ FamilyCare no longer has an immigration status requirement for children; kids can enroll based on household income, regardless of their immigration status.1
- Pregnant women with incomes up to 200% of poverty (coverage for the mother continues for 12 months after the baby is born).2
Apply for Medicaid in New Jersey
Online at HealthCare.gov, or through the NJ Family Care online application. You can apply by phone at 1-800-318-2596 or contact NJ Family Care for assistance at 1-800-701-0710.
Eligibility: The aged, blind, and disabled. Also, adults with income up to 138% of poverty, and pregnant women with income up to 200% of poverty. Children are eligible for Medicaid or CHIP with income up to 350% of poverty.



Medicaid eligibility expansion in New Jersey
Medicaid/CHIP in New Jersey is called NJ FamilyCare. The state expanded Medicaid in accordance with the Affordable Care Act (ACA), utilizing federal funding to provide health insurance for the newly-eligible population starting in 2014.
As a result, total Medicaid enrollment in New Jersey increased by 78% – nearly a million people – between the fall of 2013 and July 2023. Total Medicaid/CHIP enrollment in New Jersey had reached 2.29 million people as of mid-2023.3
The enrollment growth stems mostly from Medicaid expansion as well as the pandemic-related rule that prevented states from disenrolling anyone from Medicaid between March 2020 and March 2023. (As noted above, New Jersey resumed Medicaid eligibility redeterminations in 2023, and disenrollments began in June 2023; enrollment had declined to 2.26 million people by August 2023.)3
New Jersey has also worked to expand access to NJ FamilyCare for children via the state’s Cover All Kids initiative that began in 2021. Under this program, CHIP premiums were eliminated in 2022, along with the 90-day waiting period for CHIP coverage to take effect. And starting in 2023, children in New Jersey are eligible for NJ FamilyCare if they meet the income guidelines, regardless of their immigration status.1 A few other states have also expanded their Medicaid programs to cover undocumented immigrant children, including Washington and California (California’s program also covers undocumented young adults).
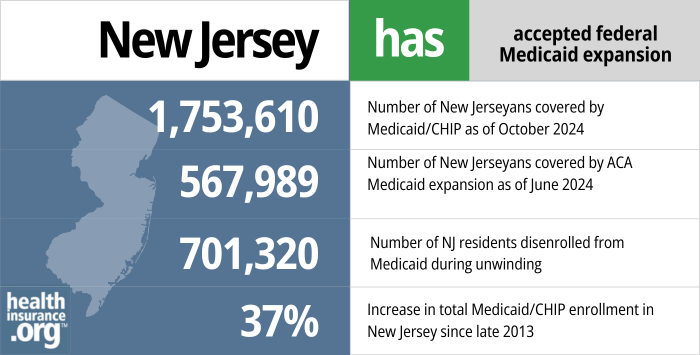
- 1,753,610 – Number of New Jerseyans covered by Medicaid/CHIP as of October 20244
- 567,989 – Number of New Jerseyans covered by ACA Medicaid expansion as of June 20245
- 701,320–Number of NJ residents disenrolled from Medicaid during unwinding6
- 37% – Increase in total Medicaid/CHIP enrollment in New Jersey since late 20137
Explore our other comprehensive guides to coverage in New Jersey

We’ve created this guide to help you understand the New Jersey health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.
Learn about health insurance coverage options in New Jersey.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in New Jersey.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in New Jersey as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.

Frequently asked questions about New Jersey Medicaid
How do I enroll in Medicaid in New Jersey?
Medicaid enrollment is available year-round. New Jersey Medicaid enrollment is handled by NJ Family Care or GetCoveredNJ (the state-run health insurance Marketplace).The NJ Family Care website also has paper applications that can be downloaded, although they strongly encourage online applications. They can be reached by phone at 1-800-701-0710 if applicants need assistance.
How does Medicaid provide financial assistance to Medicare beneficiaries in New Jersey?
Many Medicare beneficiaries receive Medicaid financial assistance that can help them with Medicare premiums, lower prescription drug costs, and pay for expenses not covered by Medicare – such as long-term care.
Our guide to financial assistance for Medicare enrollees in New Jersey includes overviews of these benefits, including Medicare Savings Programs, Medicaid long-term care coverage, and eligibility guidelines for assistance.
How is New Jersey handling Medicaid renewals after the pandemic?
Although states were not allowed to disenroll anyone from Medicaid between March 2020 and March 2023, that rule ended on March 31, 2023. States are once again disenrolling people who are no longer eligible for Medicaid and people who don’t respond to information requests during their renewal/eligibility redetermination.
By August 2023, more than 128,000 people had been disenrolled from NJ FamilyCare (mostly for proceural reasons, meaning their renewal paperwork was not completed or not returned to the state).8
States were allowed to start disenrolling people from Medicaid as early as April 1, 2023, but New Jersey waited until April 1, 2023 to resume eligibility redeterminations, and their first round of disenrollments came two months later, in June 2023.9
All NJ FamilyCare enrollees — more than 2.2 million people — will have their eligibility checked at some point in the 12-month period that began in April 2023 (by August 2023, renewals had been initiated for more than 837,000 enrollees).8 Some members’ coverage is being automatically renewed, if the state has enough information in its database to make the eligibility redetermination. Otherwise, NJ FamilyCare sends a renewal packet to the enrollee, and it’s important for members to promptly complete and return those packets in order to retain their coverage.
New Jersey’s “unwinding” plan notes that people who were determined eligible for Medicaid between April 2022 and March 2023 (either via a new application or a completed renewal) will keep their existing renewal date. The rest of the state’s Medicaid population — ie, people whose coverage has been continued due to the pandemic, but who are not up-to-date on renewals — will have their renewals spread out over the 12-month unwinding period, with a focus on prioritizing renewals for those whose eligibility determinations have been pended the longest. The state plans to initiate roughly 186,000 renewals per month, from April 2023 through March 2024.
Those who are no longer eligible for NJ FamilyCare have a special enrollment period when they can transition to other coverage, either from an employer, through GetCoveredNJ (the state-run health insurance exchange), or Medicare, for those who have become eligible for that coverage. Out of NJ FamilyCare’s more than 2.2 million members, the number of people expected to lose Medicaid during the “unwinding” of the pandemic-era continuous coverage rules is estimated at between 230,000 and 350,000 (as noted above, disenrollments had reached more than 128,000 by August 2023, which was only the third month of disenrollments).
New Jersey lawmakers are considering legislation (S.3607 and A.5273) in 2023 that would require GetCoveredNJ to automatically enroll people who lose Medicaid into a plan through the exchange, if they’re not eligible for an employer’s plan or Medicare. Both bills were still in committee as of November 2023. If enacted, the legislation would direct the exchange to automatically enroll the person in a plan prior to the end of their Medicaid coverage, to ensure seamless coverage. And the first premium would not be due until the end of the first month of coverage under the new plan. The legislation also directs the exchange to select the lowest-cost silver plan if the person’s household income is under 200% of the poverty level, in order to take advantage of cost-sharing reductions that are available on silver-level plans. (Rhode Island and California have protocols that allow them to automatically transition some people from Medicaid to exchange plans).
Legislation impacting New Jersey Medicaid
New Jersey Medicaid enrollment numbers
New Jersey has a population of more than 9 million people. As of mid-2023, there were more than 2.2 million people enrolled NJ FamilyCare,8 up from 1.3 million in 2013 and amounting to nearly a quarter of the state’s population.
According to NJ FamilyCare’s August 2023 enrollment report, about 317,000 of those enrollees were aged, blind, or disabled (those enrollees are subject to both asset and income limits), while more than 927,000 were children and nearly 769,000 were adults eligible due to the ACA’s expansion of Medicaid.8
History of New Jersey Medicaid expansion
New Jersey was one of five states that opted to partially expand Medicaid well ahead of the 2014 start date that most states used. In New Jersey, childless adults with incomes up to 23% of poverty were able to start enrolling in Medicaid in April 2011.
This was still a very low income limit, but was more generous than average: The majority of the states provided no health coverage assistance at all to low-income adults without children prior to 2014, and there are nine states as of late 2023 that still provide no assistance to childless adults living in poverty (that does not count North Carolina, as Medicaid expansion takes effect there in December 2023).
In February 2013, then-Governor Chris Christie agreed to accept federal funding for full Medicaid expansion, and later that year he signed a budget that included $227 million in federal Medicaid expansion funds.
But Christie’s acceptance of Medicaid expansion hinged on a provision that the state would only continue to offer expanded Medicaid as long as the federal government maintains its promise to always pay at least 90% of the cost of covering the population eligible under the expansion guidelines.
In June 2013, Christie vetoed a state bill (S2644) that would have made Medicaid expansion permanent regardless of any future changes in the federal funding rate, and NJ’s Medicaid expansion is still contingent on continued federal funding. Many other states have adopted similar provisions in their Medicaid expansion agreements.
In early 2014, Governor Christie said that he was “proud” of the state’s decision to expand Medicaid, but emphasized that more needed to be done to control costs in the $12 billion New Jersey Medicaid program.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in New Jersey?
Explore more resources for options in New Jersey including ACA coverage, short-term health insurance, dental insurance and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- Governor Highlights Expanded Eligibility for NJ FamilyCare Health Care Coverage as Administration Continues Efforts to Cover All Kids. State of New Jersey, Governor Phil Murphy. January 2023. ⤶ ⤶
- CMS Extends Medicaid Postpartum Coverage in New Jersey for Over 8,000 People. Centers for Medicare and Medicaid Services. October 2021. ⤶
- Medicaid Monthly Renewal Report; August 2023 Report. New Jersey Human Services. Accessed November 2023. ⤶ ⤶
- ”October 2024 Medicaid & CHIP Enrollment Data Highlights” Medicaid.gov, Accessed January 2025 ⤶
- Medicaid Enrollment – New Adult Group. Medicaid.gov, Accessed January 2025 ⤶
- Renewal Data Reports. State of New Jersey, Department of Human Services., Accessed January 2025 ⤶
- Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment. KFF.org, Accessed February 2025 ⤶
- Renewal Data Reports. State of New Jersey, Department of Human Services. August 2023 Report, accessed November 2023. ⤶ ⤶ ⤶ ⤶
- Medicaid and CHIP National Summary of Renewal Outcomes – March through July 2023. Centers for Medicare and Medicaid Services. October 2023. ⤶

