
Medicaid eligibility and enrollment in North Carolina
North Carolina Medicaid expansion took effect December 1, 2023, and 450,000 people had enrolled by May 2024

Who is eligible for Medicaid in North Carolina?
In addition to those with low incomes who are aged, blind, or disabled (receiving SSI benefits), the following populations are eligible for Medicaid in North Carolina (these income limits include a built-in 5% income disregard used with MAGI-based Medicaid eligibility determinations):
- Children aged 0-5: 215% of the federal poverty level (FPL)
- Children age 6-18: 138% of FPL
- Pregnant women: 201% of FPL (postpartum coverage for the mother now continues for 12 months after the birth)
- Adults caregivers of children or adult relatives: 45% of FPL
- Adults under age 65 with household income up to 138% of the poverty level (this is the ACA’s expansion of Medicaid)
North Carolina implemented the ACA’s Medicaid expansion starting in December 2023, under the terms of legislation the state enacted in 2023.1
for 2026 coverage
0.0%
of Federal Poverty Level
Apply for Medicaid in North Carolina
Online at HealthCare.gov or at ePass. You can enroll by phone at 1-800-318-2596. You can also apply in person at your local County Department of Social Services office or complete a paper application.
Eligibility: The aged, blind, and disabled. Also, parents with dependent children are eligible for Medicaid with a household income up to 45% of poverty level, and children are eligible for Medicaid or CHIP with incomes up to 211% of poverty; maternity-related coverage is available for pregnant women with incomes up to 196% of poverty.



Medicaid expansion now in effect in North Carolina
North Carolina expanded Medicaid under the Affordable Care Act (ACA) as of December 1, 2023. It’s estimated that more than 600,000 people in North Carolina are newly eligible for Medicaid under the expanded eligibility rules, and the state reported that more than 450,000 had enrolled by May 2024.2
Under the expanded eligibility guidelines, Medicaid is available in North Carolina to a single adult with annual income up to about $20,782 in 2024 (this is 138% of the federal poverty level), and to adults in a family of three with a household income up to about $35,631/year. (Children were already eligible for Medicaid with household income above the new limits for adults.)
State lawmakers passed Medicaid expansion legislation in 2023, and Governor Roy Cooper signed it into law in March 2023.
However, the expansion legislation did not include a specific date that eligibility rules would change, and it also made Medicaid expansion contingent on the passage of a budget for fiscal years 2023-25. The budget was ultimately approved by state lawmakers in September. Although Gov. Cooper noted that “overall this is a bad budget,” he did not veto it and instead let it become law without his signature, primarily so that Medicaid expansion could take effect. The state clarified that the eligibility rules would change on December 1, 2023.
It’s noteworthy that the American Rescue Plan allows states that newly expand Medicaid to receive additional federal Medicaid funding for their non-expansion population. Only three other states — Oklahoma, Missouri, and South Dakota have taken advantage of that. North Carolina joined them as of late 2023, and will receive the ARP’s additional Medicaid expansion funding for the first two years. For North Carolina, that additional funding will amount to $1.8 billion, on top of the billions of dollars the state will receive from the enhanced federal Medicaid funding that applies to Medicaid expansion.
North Carolina is the first state to pass Medicaid expansion legislation in several years. All of the other states that have recently expanded Medicaid have done so via voter-approved ballot measures rather than legislative support. North Carolina’s legislation passed on the 13th anniversary of the Affordable Care Act being signed into law by President Obama.
Learn how states that expanded Medicaid might reduce spending on Medicaid.
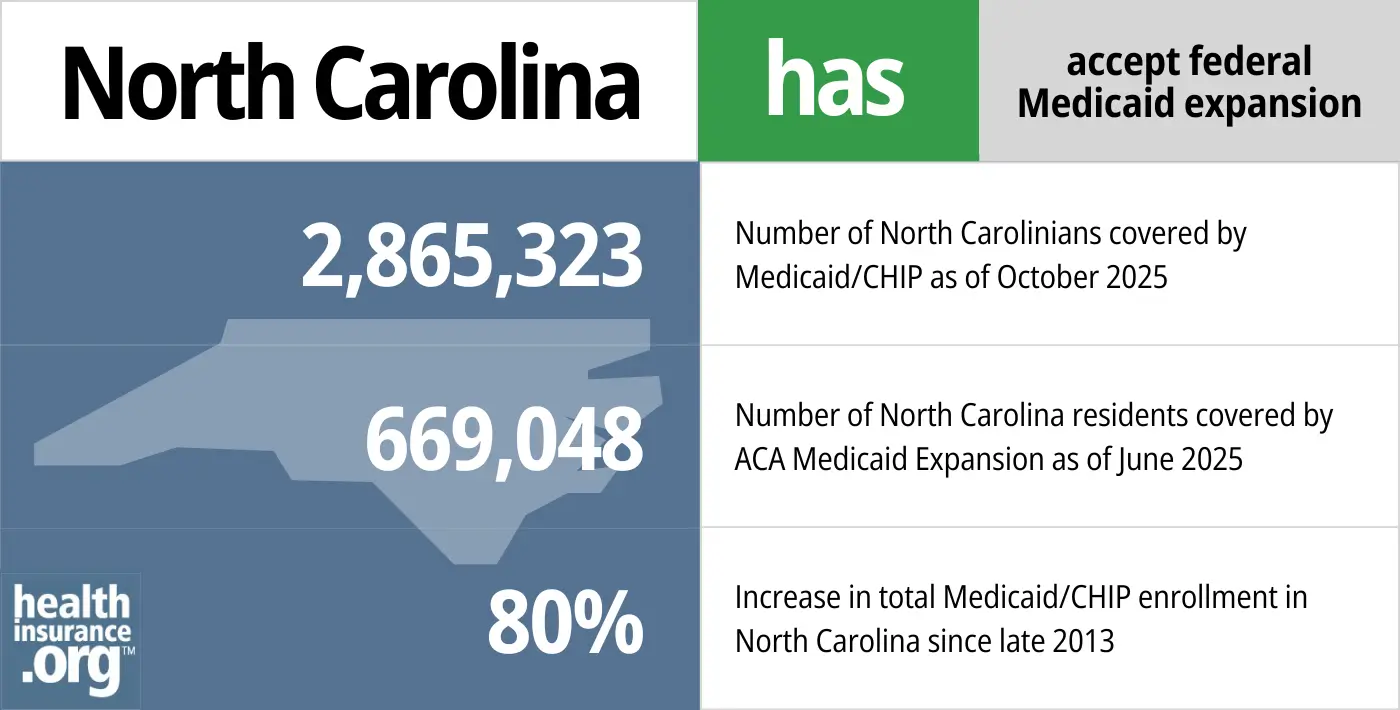
- 2,,865,323 – Number of North Carolinians covered by Medicaid/CHIP as of October 20253
- 669,048 – Number of North Carolina residents covered by ACA Medicaid expansion as of June 20254
- 80% – Increase in total Medicaid/CHIP enrollment in North Carolina since late 20135
Explore our other comprehensive guides to coverage in North Carolina

The ACA Marketplace allows individuals and families to shop for and enroll in ACA-compliant health insurance plans. Subsidies may be available based on household income to help lower costs.
Learn about the health insurance Marketplace in North Carolina.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in North Carolina.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in North Carolina as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.
Learn about short-term insurance regulations in North Carolina.

Frequently asked questions about North Carolina Medicaid
How do I enroll in Medicaid in North Carolina?
- You can apply online at ePass, a website run by the North Carolina Department of Health and Human Services (this is the recommended application option).
- You can also apply in person at the County Department of Social Services office in your home county. DHHS provides a list of documents that you’ll need to take with you if you go to a county office to apply for Medicaid.
- You can print the paper application, complete it, and then mail it to your county’s Department of Social Services office.
- You can apply online through HealthCare.gov or call them at 1-800-318-2596 to apply over the phone (use this option if you’re under 65 and don’t have Medicare)
Medicaid enrollment is available year-round.
How does Medicaid provide financial assistance to Medicare beneficiaries in North Carolina?
Many Medicare beneficiaries receive help through Medicaid with the cost of Medicare premiums, prescription drug expenses, and costs that aren’t covered by Medicare – such as long-term care.
Our guide to financial assistance for Medicare enrollees in North Carolina includes overviews of these benefits, including Medicare Savings Programs, long-term care coverage, and eligibility guidelines for assistance.
How is North Carolina handling Medicaid renewals after the pandemic?
Throughout the COVID pandemic, states received additional federal Medicaid funding but were also prohibited from disenrolling people from Medicaid. That continuous coverage requirement ended on March 31, 2023, and states could begin disenrolling people from Medicaid as early as April 1, 2023. In North Carolina, the first round of disenrollments started on July 1, 2023. By March 2024, a total of 235,039 people had been disenrolled from North Carolina Medicaid.6
But because Medicaid expansion took effect in December 2023, total enrollment in North Carolina Medicaid increased from 2,931,557 in June 2023 to 2,964,237 in May 2024.7
North Carolina Medicaid officials continued to conduct regular renewals and eligibility redeterminations throughout the pandemic, but did not terminate coverage if a person was no longer eligible or failed to respond to a request for information during an eligibility redetermination review. That has now changed, and residents could find that they lose their Medicaid coverage if they’re no longer eligible or if they fail to respond to a renewal packet.
As described above, Medicaid expansion took effect in North Carolina in December 2023. So some people who lost Medicaid starting in the summer of 2023 may find that they’re now eligible again, depending on their circumstances.
According to North Carolina’s “unwinding” plan, the state conducted renewals in the month they’re due, without prioritizing any particular populations.
People who lose Medicaid and aren’t eligible for Medicare or an employer’s plan will need to obtain their own replacement coverage. For most people in that situation, the exchange/Marketplace (HealthCare.gov) will be the best way to obtain coverage, as significant financial subsidies are available to most enrollees. And HealthCare.gov is offering an extended enrollment opportunity, from March 31, 2023 through November 30, 2024, for anyone who loses Medicaid at any time during that window.8
North Carolina Medicaid history and legislation
North Carolina Medicaid enrollment numbers
Total enrollment in North Carolina’s Medicaid and CHIP programs was 61% higher in January 2024 than it had been in 2013.
As of may 2024, Nedicaid enrollment in North Carolina was 2,964,237 (note that the CMS enrollment tracker shows fewer enrollees, with nearly 2.6 million as of January 2024, but Medicaid expansion has added a significant number of enrollees in the first few months of 2024, and the state’s numbers also include people who are eligible for partial benefits, and).
North Carolina Medicaid history
North Carolina was one of the last states to adopt the Medicaid program: Only two states took longer to implement original Medicaid coverage. The first states to provide Medicaid did so in January 1966, and North Carolina’s program didn’t become effective until January 1970.
Move to Managed Medicaid
here had been repeated efforts to move North Carolina Medicaid enrollees to managed care plans as well as expand Medicaid eligibility in North Carolina as allowed under the Affordable Care Act. The move to managed care – called the “Medicaid transformation project” was delayed, but moved ahead as of July 2021, with 1.6 million North Carolina Medicaid enrollees now covered under managed care plans (this means that private insurers administer the coverage, rather than the state paying medical providers directly). Here’s an overview of how this process unfolded in North Carolina:
On September 22, 2015, North Carolina lawmakers passed House Bill 372, known as the Medicaid Transformation and Reorganization Act, to privatize the state’s Medicaid system; then-Governor Pat McCrory signed it into law the next day. Most states were already using Medicaid managed care systems for the majority of their enrollees, but the idea remains controversial.
H.372 called for the privatization of Medicaid in North Carolina, switching to a model that involves the state contracting with for-profit managed care companies. These managed care organizations, called Prepaid Health Plans (PHPs), will receive a per-patient payment from the state Medicaid system, and will be responsible for any cost over-runs beyond what they receive up-front from the Medicaid system. This provision is designed to encourage innovation on the part of carriers and providers, in order to keep patients healthy and reduce overall healthcare costs (as opposed to the traditional fee-for-service model that pays providers each time a service is provided, regardless of overall health outcomes or costs).
The bill was contentious, and votes were divided mostly along party lines, with most Republicans supporting the measure and most Democrats opposing it. Opposition to the legislation primarily revolved around the introduction of private, for-profit health insurance carriers to the NC Medicaid system. Opponents predicted that change would result in higher administrative costs and could incentivize carriers to withhold care from Medicaid patients in order to curtail costs. They also decried the bill for its focus on privatization of the existing system, without an effort to expand Medicaid under the ACA.
Governor Roy Cooper, who was North Carolina’s Attorney General at the time, said that “turning to MCOs is a risky move.”
Medicaid managed care repeatedly delayed; took effect in mid-2021
Since the federal government funds about two-thirds of North Carolina’s Medicaid system, CMS had to approve the details of H.372 before it could be implemented. The state sent its 1115 waiver proposal to CMS in June 2016, and the approval process was expected to be lengthy. The state amended the proposal in September 2017, seeking to add a variety of changes, including a potential expansion of Medicaid, with a work requirement, if lawmakers were to approve the “Carolina Cares” Medicaid expansion proposal that was introduced in the 2017 legislative session. (The 2017 legislation was not successful, but a similar bill was introduced in April 2019 (House Bill 655); ultimately, Medicaid work requirements are no longer approved in any state under the Biden administration.)
North Carolina’s waiver proposal was approved in October 2018, and is effective from 2019 through 2024. Initially, it was to take effect in January 2019, but that was delayed quite a bit.
The state had originally planned to have the managed care transition take effect in November 2019, with a phased-in transition (Regions 2 and 4 switching to managed care in November 2019 – with enrollment beginning in July 2019 – and the rest of the state joining them in February 2020, with enrollment beginning in October 2019).
The rollout was further delayed over the budget standoff described below, and the earlier enrollment window and November 2019 effective date were scrapped, with the whole state scheduled to transition to Medicaid managed care in February 2020 instead.
And, then the February 2020 transition was nixed when Gov. McCrory and the legislature failed to agree on a budget during the 2019 General Assembly session. Implementation and open enrollment in the managed Medicaid plans was halted following an announcement of the indefinite delay.
In June 2020, North Carolina legislators again authorized the transition from fee-for-service to managed Medicaid. They set a new effective date of July 1, 2021.
North Carolina did transition to NC Managed Medicaid Care on July 1, 2021. You can find more information about this transition here. The selection of insurers to serve as managed care providers was contentious, and involved a lawsuit by insurers who did not win contracts. That was eventually settled by early 2022 when the insurers dropped their appeals.
History of Medicaid Expansion
Expansion of Medicaid in North Carolina had long been a topic of debate by the state’s politicians, policymakers, and advocacy groups. As noted above, an agreement was finally reached in 2023, and Medicaid expansion took effect in North Carolina in December 2023. But this was a decade in the making:
Expansion discussion during McCrory administration
Former Governor McCrory said that he was open to the idea of Medicaid expansion, but only after they “fix the current system.” This was a reference to the legislature’s Medicaid reform efforts, primarily aimed at transitioning to Medicaid managed care. McCrory made it clear that he would want some sort of work requirement tied to Medicaid eligibility for able-bodied adults, but at that point, no states had successfully petitioned the Obama administration to allow a work requirement and still receive federal funding for Medicaid expansion. (This changed under the Trump administration, which approved Medicaid work requirements for several states. But all of those approvals were revoked by the Biden administration.)
In January 2015, Brad Wilson, President and CEO of Blue Cross Blue Shield of North Carolina, threw his weight behind the push for Medicaid expansion, noting that “expanding Medicaid is the right thing to do for North Carolinians.”
Thom Tillis, who was sworn in as US Senator for North Carolina in January 2015, used to be strongly opposed to Medicaid expansion. But in October 2014, just two weeks before the election, he noted that “we’re trending in a direction where we should consider potential expansion… I would encourage the state legislature and the governor to consider it.” (Tillis defeated incumbent Democrat Kay Hagan in the 2014 election; Hagan supported Medicaid expansion).
By late July 2015, McCrory still had not revealed his proposal for Medicaid expansion, and advocates had begun to tire of waiting, pushing the Governor to reveal his plan or admit that he didn’t have one. And State Rep. Ken Goodman (D, Richmond) — a Medicaid expansion supporter — questioned whether McCrory would have the political clout to expand coverage anyway, given S.B.4 (which prevents the governor from unilaterally expanded Medicaid) and the fact that the majority of the state legislature was opposed to Medicaid expansion.
In September 2015, the NC Justice Center introduced radio and digital advertising calling on Gov. McCrory to reveal his plan for Medicaid expansion, noting that he said the holdup was the unknowns surrounding King v. Burwell earlier in the year (the outcome of that case was decided in June 2015, with the Supreme Court ruling that ACA subsidies were legal in every state, and paving the way for states to utilize private health plans for their Medicaid-eligible population).
By late 2015, however, McCrory had mostly walked back his support for Medicaid expansion, explaining that any expansion proposal would have to wait at least three years, while other Medicaid reforms are made in the state (see details above, regarding the transition to Medicaid managed care that eventually took effect in 2021). McCrory and President Obama had “irreconcilable differences” regarding expansion, and McCrory basically tabled the idea for the remainder of his time in office.
The governor’s race in North Carolina was one of the tightest in the country in 2016, and Cooper won by a razor-thin margin that was contested for weeks by McCrory. McCrory eventually conceded in early December.
Medicaid expansion discussion during Cooper administration
On January 4, 2017, Gov. Cooper announced his intention to file an amendment to North Carolina’s Medicaid plan by the end of the week, expanding coverage as called for in the ACA. On Friday, January 6, he notified CMS that his proposal was posted on the North Carolina Department of Health and Human Services website for a required ten-day public comment period.
Cooper’s plan was to file an amendment to the 1115 waiver proposal that North Carolina submitted to CMS in June 2016 to overhaul Medicaid without expanding it (as described above, that proposal was ultimately approved in the fall of 2018, albeit without Medicaid expansion). Once filed, Cooper’s amendment would have to have been approved by CMS, and the state would have had to secure the funding to cover its portion of the cost of expansion.
Cooper was asking North Carolina hospitals to contribute the funds that would have been necessary to cover the state’s portion of the cost of expansion (states began paying 5% of the cost of Medicaid expansion in 2017, and that gradually increased until it reached 10% in 2020, where it will remain going forward).
Ultimately, Cooper never filed his proposed amendment with CMS. But Republican lawmakers in North Carolina reacted swiftly to condemn Cooper’s announcement, noting that the state enacted legislation (S.B.4) in 2013 that prevents the governor from expanding Medicaid unilaterally (the legislation blocks any “department, agency, or institution” of North Carolina from expanding Medicaid without the consent of the General Assembly).
In a letter to CMS, Republican leadership from North Carolina’s House and Senate asked CMS to reject Governor Cooper’s proposal on the grounds that it was illegal under S.B.4.
Cooper had said that he didn’t believe S.B.4 applied in this case, as it impeded “the core executive authority of the governor to accept federal funds to look out for the health of the people.” That argument was a long shot, but the stakes were high and Cooper was doing as much as he could to secure coverage for more than half a million of the state’s poorest residents.
A week after Cooper announced his intention to expand Medicaid by amending the pending 1115 waiver, North Carolina House Speaker, Tim Moore and Senate President Pro Tem, Phil Berger, filed a federal lawsuit (naming the NC and federal departments of Health and Human Services as defendants) to block Cooper’s efforts to expand Medicaid without legislative approval. Moore and Berger said that Cooper’s “unconstitutional Obamacare expansion scheme” necessitated “swift legal action.”
Medicaid expansion proponents noted that the lawsuit filed by Moore and Berger was an overreach, and that Cooper’s efforts to expand Medicaid did not require a temporary restraining order, nor were they an issue for a federal court.
However, on January 14, 2017, the day after Moore and Berger filed their suit, a federal judge issued an order blocking CMS from approving Cooper’s proposal for the time being.
Since Cooper never filed his proposed 1115 waiver amendment to expand Medicaid, Moore and Berger dropped their lawsuit in July 2017.
H.655, introduced in North Carolina’s House of Representatives in April 2019, called for the expansion of Medicaid, albeit with a work requirement as well as premiums equal to 2% of household income. H.655 also included mandatory participation in wellness programs/preventive care. H.655 advanced out of the House Health Committee, but was not taken up by the full House (and thus was not considered by the Senate).
Governor Roy Cooper had made it clear that he was prioritizing Medicaid expansion in 2019, and included it in his budget proposal. Republican lawmakers continued their long history of opposition to Medicaid expansion, and Cooper vetoed their budget in June when it didn’t include Medicaid expansion.
Cooper had vetoed budgets before, but Republicans had a supermajority and were able to override his veto. They no longer had a supermajority in 2019, but House Republicans overrode the veto in a surprise vote when most of the Democratic representatives were at a September 11 memorial ceremony and had been told no voting would take place. The Senate did not act on the override before the end of the 2019 legislative session.
Democratic legislators again pushed for Medicaid expansion in 2020, citing increased health risks and the rising number of people who have lost employment-related insurance coverage due to the Covid-19 pandemic. However, expansion was yet again rejected.
The issue continued to be a point of conflict between Cooper and the GOP-dominated legislature. But Cooper ultimately did sign a budget in late 2021. It didn’t include Medicaid expansion, but instead called for a joint legislative committee to study the issue of Medicaid expansion and make recommendations to the legislature.
Both chambers of the legislature did strongly support Medicaid expansion in the 2022 session. But they could not come to an agreement on the specifics, largely due to questions about whether to change the state’s Certificate of Need regulations (the North Carolina Hospital Association, which has always supported Medicaid expansion, did not support the Senate’s version of H.149 due to the Certificate of Need changes it called for, which would have reduced hospital revenue).
The legislation that ultimately passed in 2023 does eliminate the Certificate of Need review for certain types of medical facilities and equipment. But it took several more months for lawmakers to agree on a budget, which was a crucial element of Medicaid expansion implementation.
Gov. Cooper noted that his preference would be for expansion to take effect as soon as possible, but the effective date was delayed due to lawmakers’ failure to agree on a budget. Cooper’s administration had tentatively established October 1, 2023 as a start date for Medicaid expansion. But that was contingent on the legislature allocating funding by September 1, and the administration acknowledged in late August that the October 1 start date was no longer feasible, given that lawmakers were not going to allocate funding by September 1.
The budget was ultimately approved by state lawmakers in September, and took effect without Cooper’s signature, allowing Medicaid expansion to take effect starting in December 2023.
In addition to the 600,000 people expected to gain coverage as a result of expansion (450,000 had enrolled by May 2024), North Carolina hospitals will also see a sharp decrease in the amount of uncompensated care they provide. Cooper has also noted that expanding Medicaid would create 40,000 jobs in North Carolina.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in North carolina?
Explore more resources for options in NC including ACA coverage, short-term health insurance, dental and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”Questions and Answers about Medicaid Expansion” North Carolina Medicaid Division of Health Benefits. April 11, 2024 ⤶
- ”NC Medicaid Expansion hits 450,000 Enrollees in Just Five Months” North Carolina Governor Roy Cooper. May 9, 2024 ⤶
- ”October 2025 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed February 2026 ⤶
- ”Medicaid Enrollment – New Adult Group“, Medicaid.gov, Accessed February 2026 ⤶
- ”Total Monthly Medicaid & CHIP Enrollment and Pre- ACA Enrollment”, KFF.org, Accessed February 2026 ⤶
- ”NC Medicaid Continuous Coverage Unwinding Dashboard”, NCDHHS, Accessed May 13, 2024 ⤶
- Enrollment Dashboard. North Carolina DHHS, NC Medicaid Division of Health Benefits. Accessed May 13, 2024. ⤶
- ”HHS Takes Additional Actions to Help People Stay Covered During Medicaid and CHIP Renewals” CMS Newsroom. Mar. 28, 2024 ⤶

