
Medicaid eligibility and enrollment in Oklahoma
More than 330,000 Oklahomans are enrolled in expanded Medicaid

Who is eligible for Medicaid in Oklahoma?
Medicaid in Oklahoma is called SoonerCare. The following populations are eligible for SoonerCare Medicaid in Oklahoma (note that these limits include the built-in 5% income disregard that’s used with MAGI-based Medicaid eligibility determinations):
- Adults under age 65 with household income up to 138% of the poverty level (this is due to the fact that Oklahoma expanded Medicaid under the ACA starting in the summer of 2021)
- Pregnant women with household income up to 210% of the poverty level (this changed as of 2023; the limit used to be 138%). Coverage for the mother continues for 12 months after the baby is born. And the Soon-to-be-Sooners program provides pregnancy-related services to pregnant women who do not qualify for full-scope Medicaid due to their immigration status.
- Children in households with income up to 210% of the poverty level
- Adults age 65 and older, and people with disabilities: Eligibility depends on both income and assets
for 2026 coverage
0.0%
of Federal Poverty Level
Apply for Medicaid in Oklahoma
Online at HealthCare.gov or the SoonerCare Medicaid website. Or by phone at 1-800-318-2596. You can also get in-person help at an Oklahoma DHS Human Services Center or contact the SoonerCare Helpline at 1-800-987-7767
Eligibility: The aged, blind, and disabled. Also, parents with income up to 42% of poverty, pregnant women with income up to 138% of poverty level, and children under age 19 with income up to 205% of poverty. Insure Oklahoma helps cover the cost of private insurance for adults with income below poverty level.



ACA’s Medicaid eligibility expansion in Oklahoma
Oklahoma Medicaid (SoonerCare) was expanded (as called for in the ACA) as of July 2021, with coverage newly available to non-elderly adults earning up to 138% of the poverty level. More than 330,000 people have gained coverage as a result of Medicaid expansion in Oklahoma.
In June 2020, voters in Oklahoma passed a Medicaid expansion ballot initiative, paving the way for Medicaid expansion to take effect in Oklahoma. The measure passed by a slim margin, garnering 50.5% of the vote. Oklahoma joined several other states — Maine, Utah, Idaho, Nebraska, and Missouri —where voters approved Medicaid expansion ballot initiatives after state lawmakers or governors had rejected Medicaid expansion for several prior years. South Dakota is the latest state to take this approach, with a voter-approved Medicaid expansion measure that takes effect in July 2023.
Although Medicaid expansion had been in the works in Oklahoma since the summer of 2020, the state still benefited from the American Rescue Plan‘s two years of additional federal funding for states that newly expand Medicaid after March 2021. In Oklahoma’s case, this amounted to about $500 million in additional funding, on top of the 90% funding that the federal government will provide indefinitely for costs associated with the newly eligible population.
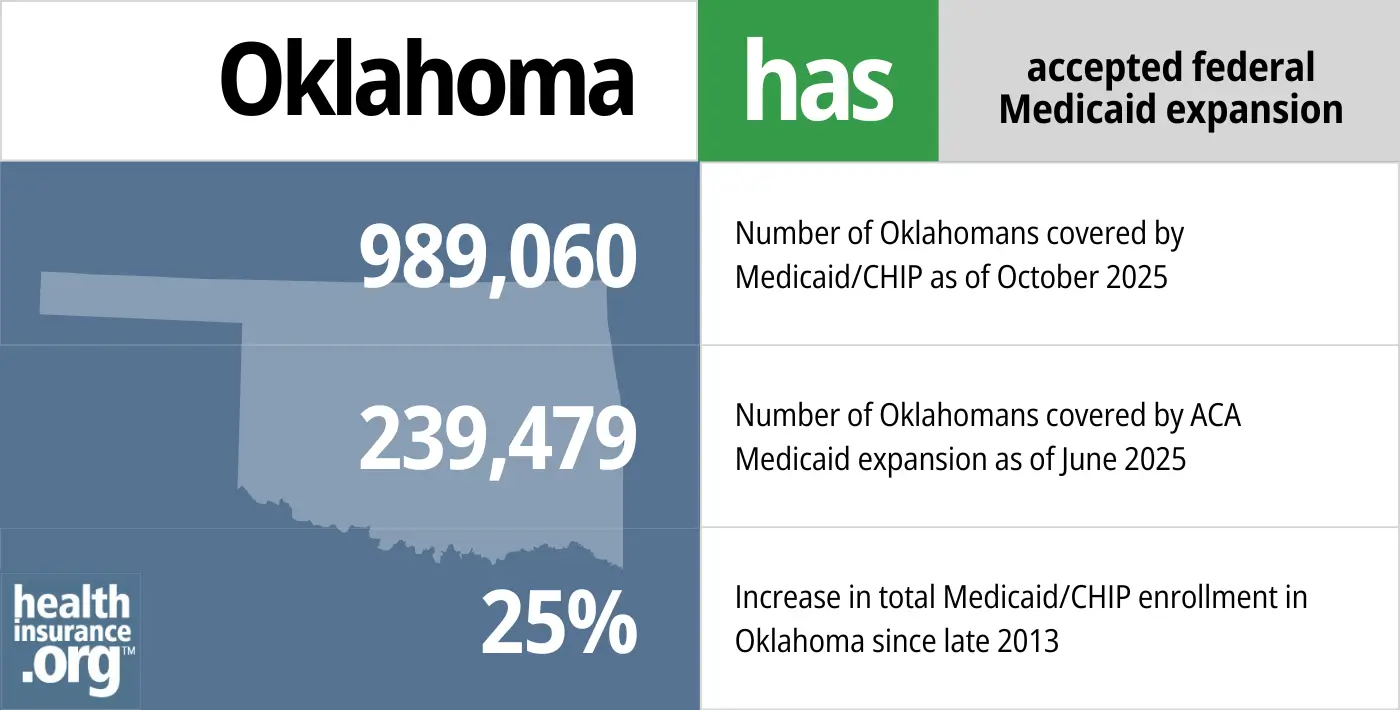
- 989,060 – Number of Oklahomans covered by Medicaid/CHIP as of October 20251
- 239,479 – Number of Oklahomans covered by ACA Medicaid expansion as of June 20252
- 25% – Increase in total Medicaid/CHIP enrollment in Oklahoma since late 20133
Explore our other comprehensive guides to coverage in Oklahoma

The ACA Marketplace allows individuals and families to shop for and enroll in ACA-compliant health insurance plans. Subsidies may be available based on household income to help lower costs.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Oklahoma.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Oklahoma as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.

Frequently asked questions about Oklahoma Medicaid
How do I apply for SoonerCare Medicaid in Oklahoma?
You can apply at HealthCare.gov or by phone at 1-800-318-2596. Applications can also be completed online through the SoonerCare enrollment portal. Medicaid enrollment is available year-round.
Assistance is also available by phone. The SoonerCare Helpline can be reached at 1-800-987-7767.
For applicants who are aged, blind, or disabled, enrollment can be completed at an Oklahoma DHS Human Services Center.
How does Medicaid provide financial assistance to Medicare beneficiaries in Oklahoma?
Many Medicare beneficiaries receive Medicaid’s help with paying for Medicare premiums, affording prescription drug costs, and covering expenses not reimbursed by Medicare – such as long-term care.
Our guide to financial assistance for Medicare enrollees in Oklahoma includes overviews of these benefits, including Medicare Savings Programs, long-term care coverage, and eligibility guidelines for assistance.
How is Oklahoma handling post-pandemic Medicaid renewals?
From March 2020 through March 2023, due to the COVID pandemic, states did not disenroll anyone from Medicaid, even if their circumstances changed and they were no longer eligible (disenrollments were only possible if the person died, moved out of state, or requested a coverage termination). But that rule ended March 31, 2023, and states have a 12-month period during which they must confirm eligibility for everyone enrolled in Medicaid.
For people no longer eligible for Medicaid federal rules allowed disenrollments to resume as early as April 1, 2023. But Oklahoma has opted to have SoonerCare disenrollments resume at the end of April. The state will take nine months to work through renewals for people enrolled in MAGI-based Medicaid (children, and adults under age 65) and a total of 12 months to work through renewals for older adults and those who are eligible due to blindness or a disability.
Oklahoma is prioritizing renewals for people whose income is now above the SoonerCare eligibility limits, who have no children under age 5, and who have already obtained other health coverage (eg, from an employer, with coverage that’s taken effect since the pandemic-related pause on Medicaid disenrollments began). They will then prioritize people who no longer meet the income limits, have no children under age 5, and who have no recent SoonerCare claims on file (indicating that they may have obtained other coverage and are no longer utilizing SoonerCare).
This approach is an effort to ensure that people who need the benefits provided by SoonerCare can keep it for the longest possible amount of time, as the state’s initial disenrollments will prioritize people who have already obtained other coverage and/or are no longer using SoonerCare benefits. But eventually, the entire SoonerCare population will have their eligibility rechecked, and people who are no longer eligible (or who don’t respond to a renewal notification) will be disenrolled from the program. The state expects that up to 300,000 people could lose SoonerCare coverage during the 12-month “unwinding” period that begins in the spring of 2023.
A person who loses SoonerCare will have an opportunity to transition to an employer’s coverage (if available), Medicare (if eligible), or a plan obtained through the Marketplace (HealthCare.gov). There are special enrollment opportunities for each types of coverage, but it’s important to sign up before the date that Medicaid ends, in order to have seamless coverage under the new plan that takes effect the first of the month after SoonerCare ends. So for example, a person whose SoonerCare is ending April 30 would need to sign up for a Marketplace plan or an employer’s plan by April 30 in order to have the new coverage in place as of May 1.
Legislation impacting Oklahoma Medicaid
Medicaid eligibility expansion initiative approved by voters, took effect July 2021
Oklahoma Medicaid (SoonerCare) was expanded (as called for in the ACA) as of July 2021, with coverage newly available to non-elderly adults earning up to 138% of the poverty level. More than 330,000 people have gained coverage as a result of Medicaid expansion in Oklahoma.
In June 2020, voters in Oklahoma passed a Medicaid expansion ballot initiative, paving the way for Medicaid expansion to take effect in Oklahoma. The measure passed by a slim margin, garnering 50.5% of the vote. Oklahoma joined several other states — Maine, Utah, Idaho, Nebraska, and Missouri —where voters approved Medicaid expansion ballot initiatives after state lawmakers or governors had rejected Medicaid expansion for several prior years. South Dakota is the latest state to take this approach, with a voter-approved Medicaid expansion measure that takes effect in July 2023.
Although Medicaid expansion had been in the works in Oklahoma since the summer of 2020, the state still benefited from the American Rescue Plan‘s two years of additional federal funding for states that newly expand Medicaid after March 2021. In Oklahoma’s case, this amounted to about $500 million in additional funding, on top of the 90% funding that the federal government will provide indefinitely for costs associated with the newly eligible population.
Oklahoma's SoonerCare Medicaid enrollment
As of February 2023, there were 1,357,723 Oklahoma residents enrolled in SoonerCare, the state’s Medicaid program. Fifty-two percent of them were children.
For perspective, SoonerCare enrollment stood at 790,051 at the end of 2013, and had been at just under 808,000 as of April 2020. But Medicaid programs all across the country have seen ballooning enrollment since 2020, amid the COVID-19 pandemic, and this was true even in states that hadn’t expanded Medicaid under the ACA.
The increased enrollment was partially due to the widespread job losses during the early days of the pandemic. But continued enrollment growth has been driven largely by the Families First Coronavirus Response Act. Under that legislation, all states are receiving additional federal Medicaid funding — but on the condition that they not disenroll anyone from Medicaid until the end of the COVID public health emergency. That end date was subsequently reset to March 31, 2023, meaning that Medicaid disenrollments were paused for a full three years, resulting in nationwide record-high Medicaid enrollment.
Oklahoma’s Medicaid enrollment growth has also been driven by the state’s expansion of Medicaid, which covered more than 330,000 people as of early 2023.
Transition to Medicaid managed care coming in 2024
SoonerCare was set to transition to a managed care system (SoonerSelect) in October 2021, but the Oklahoma Supreme Court ruled in June 2021 that the program was “invalid under Oklahoma law” (because it hadn’t been approved by the legislature) and implementation was suspended. But it’s back on track now, after the state enacted legislation to make the transition. The SoonerSelect Medicaid managed care program is expected to be up and running by the spring of 2024, and enrollees will be able to select from among two dental plans and a variety of medical plans.
Some backstory on this: In 1995, Oklahoma contracted with private insurers in a capitated managed care program to serve Medicaid enrollees in the Tulsa, Oklahoma City, and Lawton areas. But by 2004, the state had pulled the plug on the managed care system after too many providers dropped out.
In 2015, in an effort to reign in Medicaid spending growth, lawmakers in Oklahoma began considering the possibility of reviving the managed care model for the state’s Medicaid enrollees. Some advocates for Medicaid patients were opposed to the possibility, noting that it would result in disabled, blind, and elderly residents needing to switch to new doctors and new treatment plans. But supporters of privatization noted that there had been many advances in Medicaid managed care programs in the last two decades.
In May 2015, lawmakers in Oklahoma passed HB1566, which directed the state to implement a pilot program to evaluate the managed care model for Medicaid enrollees, and gather proposals from private insurers. Twenty-three “outside parties,” including Blue Cross Blue Shield of Oklahoma, provided proposals to the state. Blue Cross Blue Shield indicated that their recommendations could cut total Medicaid spending in Oklahoma (including federal and state spending) by up to $450 million over five years. But in mid-2017, Oklahoma canceled the Request for Proposals for Medicaid managed care organizations.
As of 2020, according to Kaiser Family Foundation data, Oklahoma was one of only 11 states that didn’t have any managed care organizations contracted with their Medicaid program.
That was set to change in 2021, with the scheduled transition to SoonerSelect. The state had contracted with four private health insurers and three private dental insurers contracting with the state to provide Medicaid benefits to eligible enrollees. But the Oklahoma Supreme Court overturned this plan in June 2022, noting that lawmakers would need to vote on it in order to implement it. The legislature passed Medicaid delivery reform legislation in 2022, and Governor Stitt signed it into law, paving the way for the SoonerSelect program to take effect.
Medicaid expansion in Oklahoma: The backstory
The process of getting a Medicaid expansion measure on the ballot and approved by voters took a substantial amount of work. Medicaid expansion supporters in Oklahoma gathered signatures in 2019 for Question 802, which called for Medicaid expansion under the terms outlined in the ACA (i.e., to anyone earning up to 133% of the poverty level, plus the built-in 5% income disregard). They needed 177,958 valid signatures by October 28, 2019, and reportedly submitted 313,000 — the most signatures that had ever been collected for a ballot initiative in the state. In January 2020, Oklahoma’s Secretary of State confirmed that the measure would appear on the ballot in 2020.
However, it was up to Gov. Kevin Stitt — a Republican who opposed Medicaid expansion and had expressed opposition to the ballot initiative — to determine whether the Medicaid expansion question should be on the primary ballot in June, or on the general election ballot in November. Stitt ultimately determined that the measure would appear on the June 30, 2020, primary ballot. It’s rare for a governor to opt to put a ballot initiative on the primary ballot, although former Gov. Mary Fallin did so with a medical marijuana initiative in 2018.
Stitt had previously said that he would not sign legislation calling for unaltered Medicaid expansion as outlined in the ACA, and he did not support the ballot initiative as it also called for the ACA’s expansion of Medicaid, without any modifications. But the Stitt administration had also proposed an alternative approach to Medicaid expansion — dubbed SoonerCare 2.0 — that would have eventually included premiums, a work requirement, and a per-capita spending cap. And as described below, Oklahoma was also awaiting CMS approval for a proposed Medicaid work requirement for the state’s existing Medicaid population, although the Biden administration ultimately rescinded all of the Medicaid work requirement waivers that had been approved in other states, and did not approve any that were still pending after the Trump administration left office.
SoonerCare 2.0 is described below in more detail, but Ballotpedia has a useful comparison of SoonerCare 2.0 and the ballot initiative (Question 802). As voters approved Question 802, Medicaid expansion took effect in Oklahoma as of July 2021, with no strings attached. SoonerCare 2.0 called for Medicaid expansion a year earlier — on July 1, 2020 (just one day after voters cast their ballots regarding Question 802) — but various restrictions would have then been added to the program a year later, assuming they had been approved by the Trump administration and left intact by the Biden administration.
But the future of SoonerCare 2.0 was upended after Governor Stitt unexpectedly vetoed a bill that would have provided funding for the program. Stitt had proposed the SoonerCare 2.0 program before the COVID-19 pandemic began, but noted that the widespread unemployment due to the pandemic has resulted in far more people who would be eligible for coverage under expanded Medicaid, at a financial cost that would be significantly higher than the state had initially projected. Once Stitt vetoed the funding bill, the state withdrew its expansion state plan amendment. So Medicaid was not expanded as of July 2020 under SoonerCare 2.0.
A month later, voters in Oklahoma approved ballot Question 802, paving the way for full (no strings attached) Medicaid expansion to take effect in the state as of July 2021.
Gov. Stitt’s alternative to a Medicaid expansion ballot initiative: SoonerCare 2.0 — expansion, but with strings attached (this never took effect)
As described below, Oklahoma submitted a waiver proposal to CMS in December 2018, seeking permission to implement a Medicaid work requirement. But Governor Stitt’s administration had also been working on a new approach, called SoonerCare 2.0. Instead of the straight Medicaid expansion called for in the ballot initiative that was ultimately approved by voters in 2020, Stitt’s proposal was significantly more complicated.
In early 2020, the Stitt administration expressed support for the Trump administration’s Healthy Adult Opportunity Medicaid waiver approach, and rolled out a proposal designed to take advantage of the new flexibility the federal government is offering states.
SoonerCare 2.0 called for Medicaid expansion as of July 2020, although as noted above, that was canceled as a result of the COVID-19 pandemic. But the second phase of the program, which would have required federal approval and would have taken effect in July 2021, called for premiums for people eligible due to Medicaid expansion, a per-capita spending cap, a waiver of retroactive coverage, and a Medicaid work requirement.
As described above, Stitt surprised lawmakers in May 2020 when he vetoed the bill they had passed that would have provided funding for the SoonerCare 2.0 program that Stitt had proposed. And the state soon withdrew the state plan amendment that called for Medicaid expansion to take effect in July 2020.
Although Medicaid expansion in July 2020 would have significantly improved access to health coverage in the state, consumer advocates worried that the various restrictions in the proposed SoonerCare 2.0 plan would have subsequently reduced the number of people covered under the program. And the proposed per-capita spending cap would have hampered the program’s ability to cope during an economic downturn.
Oklahoma sought federal approval for a Medicaid work requirement in 2018, but it was never approved
Oklahoma had long sought federal permission to impose a work requirement on its Medicaid population — despite rejecting Medicaid expansion until voters authorized it themselves. The work requirement proposal was based on the executive order signed by then-Governor Mary Fallin in March 2018, and HB2932, enacted in May 2018, both of which directed the Oklahoma Health Care Authority to seek federal permission to implement a Medicaid work requirement.
Throughout the summer of 2018, the Oklahoma Health Care Authority received 1,000 comments from the public on the proposed work requirement. The state submitted its proposed SoonerCare amendment in December 2018 (the proposal was still pending federal approval when the Biden administration took office, and was never approved). The state’s proposed amendment would have:
- Required non-exempt SoonerCare enrollees, age 19-50, to work at least 20 hours per week (or participate in various community engagement activities, including community service, job training, etc. for a total of 20 hours per week).
- Allowed the state to waive retroactive eligibility (except for blind, elderly, and disabled population, and Tax Equity and Fiscal Responsibility population).
Various populations would have been exempt from the work requirement, but the state estimated that out of 102,000 SoonerCare enrollees who were aged 19 to 50, roughly 6,000 would be subject to the work requirement, as the rest would be exempt (again, this was based on pre-Medicaid expansion numbers, when the vast majority of enrollees were either children or elderly).
If a non-exempt person did not comply with the work requirement, their Medicaid coverage would have been suspended. After at least one month of suspension, the person would have been allowed to re-apply for Medicaid, but would have been required to demonstrate that they were in compliance with the work requirement.
The draft proposal noted that non-elderly adult Medicaid enrollment in Oklahoma had been relatively flat since 2014, but “is expected to decline as members move from public assistance to community engagement by becoming gainfully employed as a result of the education and training initiatives under this demonstration.” In other words, they expected people to lose their Medicaid coverage — which could happen because a person works enough that their income exceeds the Medicaid eligibility cap, or because they failed to comply with the work requirement (which can happen for a variety of reasons including lack of understanding of the reporting requirements, even for people who are working).
The impact of delaying Medicaid expansion by seven years
Oklahoma’s Medicaid expansion took effect on July 1, 2021 — seven and a half years after federal funding for Medicaid expansion first became available under the Affordable Care Act.
Due in large part to lack of Medicaid expansion prior to that, Oklahoma was one of only two states where the uninsured rate was still above 14% in 2019. According to US Census data, 14.3% of Oklahoma residents were uninsured in 2019. Texas was the only state with a higher uninsured rate (Texas still has not expanded Medicaid as of 2022). Nationwide, the average uninsured rate was 9.2% in 2019.
Democrats in Oklahoma’s legislature had been pushing for Medicaid expansion for years. But Republicans hold a substantial majority in both chambers of the state’s legislature, and Governor Kevin Stitt continued former Governor Mary Fallin’s opposition to Medicaid. After years of lawmakers rejecting Medicaid expansion, a ballot initiative ultimately took the issue directly to the state’s residents, and they approved it.
Oklahoma commissioned the Leavitt Report, which found that expansion of Medicaid would directly cost the state $850 million over a ten-year period, but would ultimately result in a net savings of $464 million for Oklahoma over the same time period, when other factors were taken into consideration. Despite that finding, the state legislature was not receptive to expansion of Medicaid. Lawmakers and the Governor had concerns over the amount that the state was currently spending to provide care for the existing Medicaid population, and they expressed concerns about the sustainability of adding more people to the state’s Medicaid program.
Failed attempt to cut Medicaid eligibility for parents
Despite not expanding Medicaid under the ACA, Oklahoma lawmakers also attempted to go one step further than that, and tighten already-stringent eligibility rules even more.
Amid a budget shortfall of $1.3 billion, lawmakers in the Oklahoma House of Representatives passed HB2665 in March 2016. HB2665 called for eliminating Medicaid eligibility for non-pregnant, able-bodied adults under age 65. All 30 Democrats in the Oklahoma House opposed the bill, and were joined by four Republicans.
But the Senate did not pass HB2665, so Medicaid eligibility for parents in Oklahoma remained unchanged.
As background, the only non-pregnant, able-bodied adults under age 65 who qualified for Medicaid prior to July 2021 were those with household incomes up to 43% of the poverty level, and who also had dependent children.
Most able-bodied adults with dependent children weren’t able to qualify for Medicaid in Oklahoma because their incomes weren’t low enough. And able-bodied adults without dependent children weren’t eligible for Medicaid at all in Oklahoma, regardless of their income, because the state had not (as of that point) accepted federal funding to expand Medicaid.
If HB2665 had been passed by the Senate and signed into law, it would have cut about 111,000 people from SoonerCare (Oklahoma Medicaid), effective November 2016. The measure was expected to save the state about $130 million a year, but the state would have also missed out on $203 million a year in matching funds if they had eliminated the state funding.
The federal government would have had to approve a waiver in order for Oklahoma to be able to cut Medicaid eligibility for low-income, able-bodied parents. Representative Doug Cox (R-Grove) authored HB2665. He has also said that he was “working with some folks to design something” in terms of legislation to expand Medicaid in Oklahoma under the ACA.
Other low-income health programs in Oklahoma
In addition to SoonerCare Medicaid, the state also operates SoonerPlan, which is a state-funded program to provide family planning services to men and women with incomes that do not exceed 133% of poverty level, and who are not enrolled in SoonerCare Medicaid.
Another state-run program, Insure Oklahoma, predates the ACA by several years and subsidizes private health insurance for residents with incomes up to the poverty level. Prior to 2014, the upper income limit for Insure Oklahoma was 200% of poverty level, but the limit was lowered in January 2014 because enrollees with incomes above 100% of poverty became eligible to receive federal tax credits to offset the cost of private plans purchased through the exchange.
Insure Oklahoma offers assistance to people who obtain employer-sponsored insurance from one of the nearly 3,000 employers who are enrolled in the Insure Oklahoma program (with a 60/25/15, state/employer/employee split on the premiums).
As of early 2023, there were nearly 9,700 enrollees in the employer-sponsored insurance program. (Total enrollment had stood at around 30,000 enrollees in 2013, but that included an individual insurance program that is no longer needed due to Medicaid expansion. And Medicaid expansion also makes the employer-sponsored insurance program through InsureOklahoma less necessary.)
Funding for Insure Oklahoma comes from tobacco taxes and matching federal funds that were scheduled to cease at the end of 2013 and be replaced with Medicaid expansion funding. But because Oklahoma did not accept Medicaid expansion at that point, the state has instead continued to negotiate with the federal government to get extensions for Insure Oklahoma funding.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Oklahoma?
Explore more resources for options in OK including ACA coverage, short-term health insurance, dental and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- “October 2025Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed February 2026 ⤶
- “Medicaid Enrollment – New Adult Group”, Medicaid.gov, Accessed February 2026 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed February 2026 ⤶

