What is a health savings account (HSA)?
A health savings account (HSA) is a tax-deductible savings account that’s used in conjunction with an HSA-qualified high-deductible health insurance plan (HDHP).
Learn more: Top ten reasons to use a health savings account.
FAQs about health savings accounts
- How does a health savings account work?
- Who should consider a high-deductible health plan?
- Can I buy HSA-compatible health insurance through the exchange?
- What's the difference between an FSA and an HSA?
- Can I use my HSA to pay for COVID testing and treatment?
- Can I use my HSA to purchase over-the-counter medications?
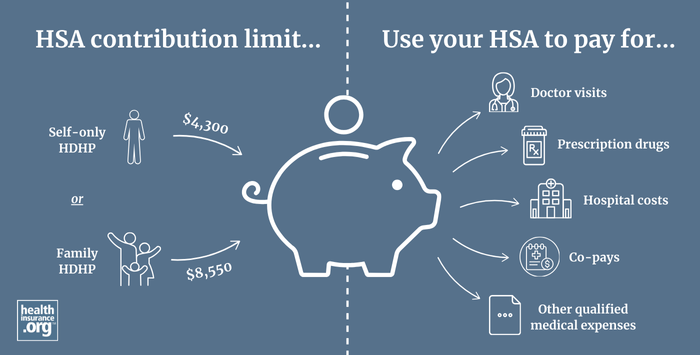
What are the HSA contribution limits for 2025?
HSA regulations allow you to legally reduce federal income tax by depositing pre-tax money into a health savings account, as long as you’re covered by an HSA-qualified HDHP. Just like IRAs, HSA contributions can be made until the tax filing deadline, which is roughly April 15 of the following year.
For 2025, you can deposit up to $4,350 if you have HDHP coverage for just yourself, or $8,550 if your HDHP covers at least one additional family member1 ("family" coverage does not have to cover an entire family). You have until April 15, 2026 to contribute some or all of this amount if you have HDHP coverage in 2025.
Account holders who are 55 or older are allowed to deposit an additional $1,000 in catch-up contributions. (This amount is not adjusted for inflation; it’s always $1,000 per year.) HSA contributions can be made throughout the year, or all at once – it's up to the account holder.
There’s no minimum deposit, but whatever you put into your account is an “above-the-line” tax deduction that reduces your adjusted gross income. If you make your HSA contributions via your employer – as a payroll deduction (salary reduction) – the money will be taken out of your check before taxes, so you'll avoid both income tax and payroll tax on the contributions.2
The health plan that pairs with an HSA
Because the HSA is paired with a high-deductible health plan (HDHP), your health insurance premiums will often be lower than they would be on a more traditional plan with a lower deductible. But HSA-qualified plans vary considerably in their out-of-pocket exposure; deductibles on HSA-qualified plans in 2025 can be as low as $1,650 for an individual and $3,300 for a family.1
If you're buying your own health insurance (as opposed to getting it from an employer), you’ll likely find HSA-qualified HDHP options available through the exchange, as well as off the exchange (note that premium subsidies are only available if you get your coverage through the exchange). These plans are available nearly everywhere.
But since the maximum out-of-pocket limits on HSA-qualified plans are lower than the maximum allowable out-of-pocket limits on other plans, there will typically be some non-HSA-qualified plans (with higher out-of-pocket exposure) that have lower premiums than the available HSA-qualified plans. So while an HSA-qualified plan will typically be among the lower-priced plans available, it won't necessarily be the lowest-cost plan available.
It’s important to note that you can only contribute to an HSA if your current health insurance policy is an HSA-qualified high-deductible health plan (HDHP). Not all plans with high deductibles are HSA-qualified, so check with your employer or your health insurance carrier if you’re unsure.
Contributions to your HSA can be made by you or by your employer, and they’re yours forever – there’s no “use it or lose it” provision with HSAs, and the money rolls over from one year to the next. HSA funds can be stored in a variety of savings vehicles, including bank accounts and brokerage accounts (ie, the funds can be invested in the stock market if you prefer that option and your HSA administrator allows it), and there are numerous HSA custodians/administrators from which to choose.
IRS expands preventive care umbrella to cover some chronic care treatments and new preventive care
The ACA requires all non-grandfathered health plans to pay for certain preventive care before the deductible, and this provision applies to HDHPs as well. But under an HDHP, non-preventive services cannot be paid for by the health plan until the insured has met the minimum deductible.
So HDHPs cannot have copays for office visits or prescriptions before the deductible is met, which is one of the ways they differ from other health plans that have high deductibles but are not HDHPs.
But under guidelines that the IRS issued in mid-2019, the list of preventive services that can be covered pre-deductible on an HDHP has been expanded to include certain treatments for certain specific chronic conditions. It's optional for insurers to classify these services as preventive, but if they do, the insurer can cover them (partially or in full) before the enrollee meets the deductible, and the health plan will continue to have its HDHP status. In late 2024, the IRS issued additional guidelines to further expand the list of preventive services that an HDHP can pay for before the deductible is met.3 These rule changes are explained in more detail in our overview of HDHPs.
Using your HSA funds
You can use the tax-free savings in your HSA to pay for doctor visits, hospital costs, deductibles, co-pays, prescription drugs, or any other qualified medical expenses. Once the out-of-pocket maximum on your health insurance policy is met, your health insurance plan will pay for your remaining covered medical expenses that year, the same as any other health plan.
If you switch to a health insurance policy that’s not HSA-qualified, you’ll no longer be able to contribute to your HSA. But you’ll still be able to take money out of your HSA at any time to pay for qualified medical expenses, with no taxes or penalties assessed. If you don’t use the money for medical expenses and still have funds available after age 65, you can withdraw them for non-medical purposes with no penalties, although income tax would be assessed at that point, with the HSA functioning much like a traditional IRA.4
In 2024, the IRS issued guidance to add male condoms to the list of qualified medical expenses, thus allowing them to be purchased with pre-tax HSA (or HRA or FSA) funds.5
You can also withdraw tax-free money from your HSA to pay Medicare premiums (for Part A, if you have to pay premiums for it – although most people don't – and for Part B and Part D, but not for Medigap plans).
Tax-free HSA funds can also be used to pay long-term care premiums. There are limits on how much you can withdraw tax-free from your HSA to pay long-term care insurance premiums. (These limits are for 2025; the IRS indexes them for inflation annually.) If your age is:6
- 40 or younger, you can withdraw $480 tax-free to pay long-term care insurance premiums
- Older than 40, but not older than 50, you can withdraw $900
- Older than 50, but not older than 60, you can withdraw $1,800
- Older than 60, but not older than 70 you can withdraw $4,810
- Older than 70, you can withdraw $6,020
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- "Revenue Procedure 2024-25" Internal Revenue Service. Accessed May 21, 2024 ⤶ ⤶
- ”The Deductibility of HSA Contributions” HSA Store. Accessed Apr. 18, 2025 ⤶
- "Notice 2024-75: Preventive Care for Purposes of Qualifying as a High Deductible Health Plan under Section 223" Internal Revenue Service. Accessed Nov. 19, 2024 ⤶
- "About Publication 969, Health Savings Accounts and Other Tax-Favored Health Plans" Internal Revenue Service. Accessed May 21, 2024 ⤶
- "Notice 2024-71. Expenses Treated as Amounts Paid for Medical Care" Internal Revenue Service. Accessed Nov. 20, 2024 ⤶
- "Revenue Procedure 2024-40" Internal Revenue Service. Accessed Apr. 18, 2025 ⤶
Explore HSA-qualified high-deductible health plans
Get your free quote now through licensed agency partners!


