Home > States > Health insurance in Missouri
See your Missouri health insurance coverage options.

Find affordable individual and family plans, small-group, short-term, or dental plans through licensed agency partners.

Missouri Health Insurance Consumer Guide
This guide was created to help you understand the health insurance options available to you and your family in Missouri. An Affordable Care Act (ACA) Marketplace plan is cost-effective for many people.
These plans are also called Obamacare or exchange plans (exchange is another word for Marketplace). Missouri uses the federally-run health insurance Marketplace, HealthCare.gov. The Marketplace website will let you shop for health plans offered by nine private insurance companies (plan availability varies from one area of the state to another).1 If you buy a plan on the Marketplace, the government may help pay for it through an income-based advance premium tax credit.
Explore our other comprehensive guides to coverage in Missouri
Dental coverage in Missouri
Get protection from the high costs of dental work. Compare different plan options to find premiums and deductibles that fit your budget.
Missouri’s Medicaid program

In 2021, Missouri adopted the ACA’s Medicaid expansion.2 By April 2023, about 1.5 million people in Missouri were enrolled in Medicaid and CHIP plans.3

Medicare coverage and enrollment in Missouri

As of April 2023, nearly 1.3 million people in Missouri have Medicare coverage.4 Our guide includes details about Medicare Advantage, Medigap, and Medicare Part D plans in Missouri.

Short-term coverage in Missouri

Missourians can get short-term health insurance plans with initial durations up to 12 months with renewals up to three years. As of 2023, there were at least 11 insurers selling short-term health insurance plans in Missouri.

Frequently asked questions about health insurance in Missouri
Who can buy Marketplace health insurance?
You can buy individual and family health insurance from Missouri’s Marketplace if:5
- You live in Missouri.
- You are lawfully present in the U.S.
- You don’t have Medicare.
- You are not incarcerated.
Eligibility for financial assistance with your Marketplace coverage will depend on your income. In addition, to be eligible for financial assistance in the Marketplace:
- You must not be eligible for affordable employer-sponsored health coverage.
- You must not be eligible for Medicaid/CHIP (MO HealthNet).
- You must not be eligible for premium-free Medicare Part A.6
When can I enroll in an ACA-compliant plan in Missouri?
In Missouri, the open enrollment period to sign up for ACA-compliant individual and family health plans is from November 1 to January 15.
- If you enroll by December 15, your coverage starts on January 1.
- If you enroll between December 16 and January 15, your coverage starts February 1.7
Outside of open enrollment, you can still make plan changes or enroll in the Marketplace if you qualify for a special enrollment period (SEP). Most SEPs require a qualifying life event, such as involuntary loss of coverage, marriage, or having a baby.
But there are instances where you don’t need a qualifying life event to apply.8 For example:
- If you’re eligible for premium tax credits and your income is not more than 150% of the poverty level, you can enroll anytime until at least 2025.9
- If you’re a Native American, you can enroll anytime.10
- If you lose Medicaid or CHIP between March 31, 2023 and July 31, 2024, you can enroll through the extended SEP that continues throughout that window.11
How do I enroll in a Marketplace plan in Missouri?
In Missouri, you have a few options to enroll in a Marketplace health plan:
- Directly through HealthCare.gov – the ACA exchange
- By phone at (800) 318-2596
- By contacting agents, navigators, certified application counselors or an approved enhanced direct enrollment entity.12
- By mailing in a paper application
Many people – like early retirees not yet on Medicare, self-employed people, and those who work for small businesses without health benefits – use the ACA Marketplace.
How can I find affordable health insurance in Missouri?
In Missouri, you can find affordable health plans through the ACA Marketplace’s website: HeathCare.gov.
Under ACA, you may qualify for income-based subsidies called Advance Premium Tax Credits (APTC). These credits lower your premiums.
In 2023, more than 90% of people enrolled in Missouri’s exchange received premium subsidies, saving about $584 per month. Those who received subsidies pay an average monthly premium of $94.13
If your income isn’t more than 250% of the federal poverty level, you may also receive cost-sharing reductions (CSR), as long as you enroll in a Silver-level plan.14 CSRs reduce your out-of-pocket costs when you use your health insurance.
Missourians may also find affordable coverage through Medicaid if eligible. Missouri expanded Medicaid eligibility guidelines in 2021, under the terms of a voter-approved ballot measure that implemented the ACA’s Medicaid expansion. This allows adults to enroll in Medicaid with a household income up to 138% of the poverty level. Learn more in our Missouri Medicaid guide.
Short-term plans are also a low-cost option for people who are not eligible for employer plans, Medicaid, Medicare, or subsidies through the exchange.
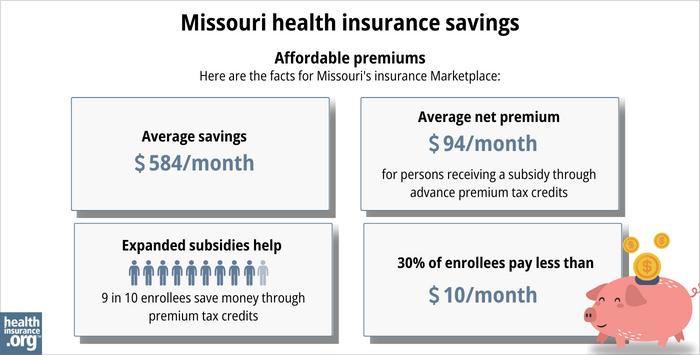
Source: CMS.gov15
How many insurers offer Marketplace coverage in Missouri?
Nine insurers offer coverage in the Missouri Health Insurance Marketplace for 2024, including a few that have expanded their coverage areas for 2024, resulting in more available plans in some areas of the state.1
There were ten insurers offering plans in 2023,16, but Cigna is exiting Missouri’s individual insurance market at the end of 2023.17
Are Marketplace health insurance premiums increasing in Missouri?
Here are the 2024 average approved rate changes for Missouri’s individual/family health insurance market (before any subsidies are applied):18
Missouri’s ACA Marketplace Plan 2024 Proposed Rate Increases by Insurance Company |
|
|---|---|
| Issuer | Percent Increase |
| Aetna | 6.09% |
| Blue Cross Blue Shield of Kansas City | -4.30% |
| Celtic Insurance Company | 4.36% |
| Cox Health Systems Insurance Company | -4.11% |
| Healthy Alliance Life Insurance Company (Anthem) | 5.8% |
| Medica Insurance Company | -0.19% |
| Oscar Insurance Company | 1.38% |
| SSM Health Insurance Company | 18.71% |
| United HealthCare Insurance Company | 5.79% |
Source: Missouri Department of Insurance19
Cigna will not offer individual and family health plans on Missouri’s Marketplace in 2024.
The approved rate increases are for full-price premiums, and amount to a weighted average rate increase of 4.6% for 2024.20
Since most people on Missouri’s exchange receive premium tax credits, they don’t pay the full price.21 If you qualify for subsidies, your net rate change depends on changes in your plan rates and your subsidy amounts.
A note about rate review in Missouri: Prior to 2017, Missouri did not have an effective rate review program, but that changed in 2017 (as of 2023, only two states — Oklahoma and Wyoming — do not have an effective rate review program and thus rely on the federal government for this).22
Since 2017, under the terms of SB865, the Missouri Department of Insurance has taken an active role in reviewing insurers’ proposed rate changes.23 State regulators determine whether the proposed rates are justified, although they are not allowed to prevent an insurer from implementing a rate change, even if the state does not consider it to be justified (this is the same as the federal rate review process).
For perspective, here’s a summary of how unsubsidized premiums have changed over the years in Missouri’s individual/family health insurance market:
How many people are insured through Missouri’s Marketplace?
During the 2023 open enrollment, 257,629 people signed up for private health plans through Missouri’s exchange/Marketplace.33
Usually, when a state expands Medicaid, Marketplace enrollment drops. That’s because people with income between 100 and 138% of the federal poverty level transfer from Marketplace plans to Medicaid.
But Missouri’s Marketplace enrollment grew in 2022 and 2023 despite the 2021 Medicaid expansion. This growth is likely because of larger subsidies from the American Rescue Plan and the Inflation Reduction Act. The larger and more accessible subsidies make coverage more affordable.34
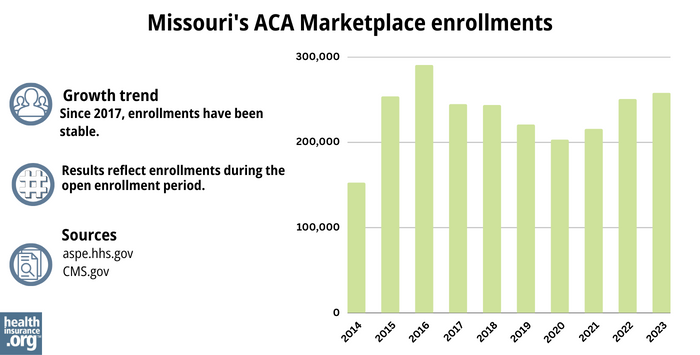
Source: 2014,35 2015,36 2016,37 2017,38 2018,39 2019,40 2020,41 2021,42 2022,43 202344
What health insurance resources are available to Missouri residents?
HealthCare.gov
The official federal website where you can sign up for health insurance plans through the ACA Marketplace.
Missouri Department of Insurance
Oversees and regulates health plans, brokers, and agents.
MO HealthNet
Missouri’s Medicaid.
Missouri State Health Insurance Assistance Program (Missouri SHIP)
Helps Missourians with Medicare benefits.
Medicare Rights Center
National resource with a website and call center to provide information and help for people on Medicare.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- Missouri Department of Commerce and Insurance releases health insurance rates for 2024 with more choices for Missourians. Missouri Department of Commerce and Insurance. November 2023. ⤶ ⤶
- “Missouri Medicaid Expansion Brings Quality Essential Health Coverage to More than 275,000 Missourians” CMS.gov, Oct. 4, 2021 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment“ KFF.org, April 2023 ⤶
- “Medicare Monthly Enrollment” CMS.gov, April 2023 ⤶
- ”A quick guide to the Health Insurance Marketplace” HealthCare.gov ⤶
- Medicare and the Marketplace, Master FAQ. Centers for Medicare and Medicaid Services. Accessed November 2023. ⤶
- “A quick guide to the Health Insurance Marketplace®” HealthCare.gov, Accessed August, 2023 ⤶
- “Who doesn’t need a special enrollment period?“ healthinsurance.org, Accessed August 2023 ⤶
- “An SEP if your income doesn’t exceed 150% of the federal poverty level” healthinsurance.org. Accessed August 2023 ⤶
- “AIAN ACA 2021” CMS.gov, Accessed September 2023 ⤶
- “temp-sep-unwinding-faq.pdf” CMS.gov, Jan. 27, 2023 ⤶
- “Entities Approved to Use Enhanced Direct Enrollment” CMS.gov, April 28, 2023 ⤶
- “2023 Marketplace Open Enrollment Period Public Use Files” CMS.gov, March 2023 ⤶
- “Federal Poverty Level (FPL)” HealthCare.gov, 2023 ⤶
- “2023 OEP State-Level Public Use File (ZIP)” CMS.gov, March 23, 2023 ⤶
- “Missouri 2023 Single Risk Pool Final Rates as of 11/1/2022” Missouri Department of Insurance, Accessed September 2023 ⤶
- ”Health Insurance Rate Filings for 2024 Plan Year” Missouri Department of Insurance. Accessed October 2023. ⤶
- Missouri 2024 Single Risk Pool Final Rates as of 11/1/2023. Missouri Department of Insurance, insurance.mo.gov, Accessed December 2023 ⤶
- Missouri 2024 Single Risk Pool Final Rates as of 11/1/2023. Missouri Department of Insurance, insurance.mo.gov, Accessed December 2023 ⤶
- Missouri: *Final* Avg. Unsubsidized 2024 #ACA Rate Changes: +4.6%. ACA Signups. November 2023. ⤶
- “Effectuated Enrollment: Early 2023 Snapshot and Full Year 2022 Average” CMS.gov, March 15, 2023. ⤶
- ”State Effective Rate Review Programs” Centers for Medicare and Medicaid Services. Accessed October 2023. ⤶
- ”Missouri SB865; enacted 2016” BillTrack50. Accessed October 2023. ⤶
- Analysis Finds No Nationwide Increase in Health Insurance Marketplace Premiums. The Commonwealth Fund. December 2014. ⤶
- FINAL PROJECTION: 2016 Weighted Avg. Rate Increases: 12-13% Nationally* ACA Signups. October 2015. ⤶
- Avg. UNSUBSIDIZED Indy Mkt Rate Hikes: 25% (49 States + DC). ACA Signups. October 2016. ⤶
- Alabama, Hawaii, Missouri, Wyoming: Wrapping Up The 2018 Rate Hike Project W/An Assist From Avalere. ACA Signups. October 2017. ⤶
- 2019 Rate Hike Project Wrap-Up: FINAL/APPROVED Rate Changes For Missouri & New Hampshire. ACA Signups. November 2018. ⤶
- Missouri: *Final* Avg. 2020 #ACA Rate Changes: 2.0% Decrease. ACA Signups. October 2019. ⤶
- Missouri: Preliminary Avg. 2021 #ACA Premiums: +4.7% Indy Market, +9.25% Sm. Group. ACA Signups. September 2020. ⤶
- 2022 Rate Changes. ACA Signups. October 2021. ⤶
- Missouri: Final Avg. Unsubsidized 2023 #ACA Rate Changes: +11.0% (Updated). ACA Signups. July 2022. ⤶
- “Marketplace 2023 Open Enrollment Period Report: Final National Snapshot” CMS.gov, January 2023 ⤶
- “Health Insurance Marketplaces 2023 Open Enrollment Report” CMS.gov, Accessed August 2023 ⤶
- “ASPE Issue Brief (2014)” ASPE, 2015 ⤶
- “Health Insurance Marketplaces 2015 Open Enrollment Period: March Enrollment Report”, HHS.gov, 2015 ⤶
- “HEALTH INSURANCE MARKETPLACES 2016 OPEN ENROLLMENT PERIOD: FINAL ENROLLMENT REPORT” HHS.gov, 2016 ⤶
- “2017 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2017 ⤶
- “2018 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2018 ⤶
- “2019 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2019 ⤶
- “2020 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2020 ⤶
- “2021 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2021 ⤶
- “2022 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2022 ⤶
- “Health Insurance Marketplaces 2023 Open Enrollment Report” CMS.gov, 2023 ⤶







