Home > States > Health insurance in Nevada
See your Nevada health insurance coverage options.

Find individual and family plans, small-group, short-term or Medicare plans through licensed agency partners.

Nevada Health Insurance Consumer Guide
We’ve created this Nevada health insurance guide and the FAQs below to help you understand the health coverage options and possible financial assistance available to you and your family.
Nevada created its own state-run exchange, called Nevada Health Link, which is overseen by the Silver State Health Insurance Exchange.1 (Nevada had a state-run exchange platform in 2014, switched to the federally-run HealthCare.gov platform for 2015 through 2019, then switched back to a state-run platform in 2020.)
Eight private insurance companies offer Marketplace plans through Nevada Health Link for 2024,2 including two that are new for 2024. Income-based subsidies are available through Nevada Health Link, making coverage much more affordable than it would otherwise be.
A Nevada Health Link plan can be a great coverage option if you aren’t eligible for Medicare or Medicaid, and also don’t have an offer of affordable health insurance from your employer.
Explore our other comprehensive guides to coverage in Nevada
Dental coverage in Nevada

Looking to improve your smile and save some money at the dentist’s office? Dental insurance may be a worthwhile supplement to your medical coverage. Our guide explores dental coverage options in Nevada.

Nevada’s Medicaid program

Starting in January 2014, Nevada expanded Medicaid eligibility under the ACA.3 From late 2013 to early 2023, enrollment in Nevada’s Medicaid program grew to nearly 900,000 people. This was 171% higher than enrollment had been in 2023 – the highest enrollment growth in the nation.4

Medicare Enrollment in Nevada

More than 580,000 Nevada residents were enrolled in Medicare as of April 2023.5 Our Nevada Medicare guide explains what you need to know about the various parts of Medicare, as well as Nevada’s Medigap (Medicare Supplement) regulations.

Short-term coverage in Nevada

Nevada allows short-term plans to be sold with terms of up to 185 days. As of 2023, there were at least six insurers selling short-term health plans in Nevada.6

Frequently asked questions about health insurance in Nevada
Who can buy Marketplace health insurance?
In order to sign up for private health coverage through Nevada Health Link, you must:7
- Live in Nevada
- Be lawfully present in the United States
- Not be incarcerated
- Not be enrolled in Medicare8
By those rules, most Nevada residents qualify to use the exchange. But a bigger question for most people is financial assistance, and there are a few additional parameters to be eligible for subsidies in Nevada’s exchange.
To qualify for income-based Advance Premium Tax Credits (APTC) or cost-sharing reductions (CSR), you must:
- Not have access to affordable health coverage through an employer. If you have access to an employer’s plan but it seems too expensive, you can use our Employer Health Plan Affordability Calculator to see if you might qualify for premium subsidies via Nevada Health Link.
- Not be eligible for Medicaid or Check Up (CHIP).
- Not be eligible for premium-free Medicare Part A.9
Beyond those basic parameters, qualifying for Nevada Health Link subsidies depends on your household income, which is an ACA-specific calculation of MAGI.
When can I enroll in an ACA-compliant plan in Nevada?
You can sign up for an ACA-compliant individual or family health plan in Nevada between November 1 and January 15, which is the annual open enrollment period.
For coverage to take effect on January 1, you need to complete your application by December 31.10 (This is later than the deadline in most states.) If you enroll between January 1 and January 15, your coverage will take effect on February 1.11
Outside of the annual open enrollment window, you may be eligible to enroll if you experience a qualifying life event, such as giving birth or losing other health coverage. Note that some people can enroll year-round even without a specific qualifying life event.12
Enrollment in Nevada Medicaid/Check Up (CHIP) is available year-round.
A note about off-exchange enrollment: From 2014 through 2019, Nevada law required plans sold outside the exchange to be available for purchase year-round, with a waiting period of up to 90 days before the coverage would take effect. But Section 56 of Nevada SB482, enacted in 2019,13 eliminated the requirement that health plans be available year-round outside the exchange. The law took effect October 1, 2019, bringing Nevada’s rules into line with the rest of the country: Both on-exchange and off-exchange, individual major medical plans can only be purchased outside of open enrollment if the applicant has a special enrollment period triggered by a qualifying event.
How do I enroll in a Nevada Marketplace plan?
To enroll in an ACA Marketplace/exchange plan in Nevada, you can:
- Visit Nevada Health Link, which is Nevada’s health insurance exchange (another word for Marketplace). Nevada Health Link is an online platform where you can compare plans, determine whether you’re eligible for financial assistance, and enroll in the plan that best meets your needs.
- Purchase Nevada Health Link coverage with the help of an insurance broker or navigator.14
You can reach the Nevada Health Link call center by calling 1-800-547-2927, Monday to Friday, 9 am to 5 pm.
How can I find affordable health insurance in Nevada?
The Affordable Care Act (ACA) provides income-based subsidies that can help lower your premium payments each month. These subsidies are available to Nevada residents who meet the eligibility requirements and enroll in coverage through Nevada Health Link.
Eighty-six percent of Nevada Health Link enrollees were receiving premium subsidies as of early 2023, and these subsidies reduced their average health insurance premiums by $439/month. After subtracting subsidies, the average enrollee’s premium was about $104/month.15
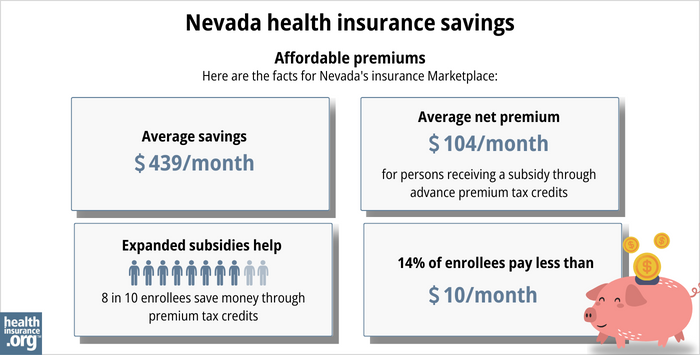
Source: CMS.gov16
If your household income is no more than 250% of the federal poverty level, you may also be eligible for cost-sharing reductions (CSR), which will reduce your deductible and other out-of-pocket expenses. These benefits are built into Silver-level plans if the applicant is eligible for them. As of 2023, nearly half of Nevada Health Link’s enrollees were receiving CSR benefits. 17
You can use both APTC and CSR benefits if you’re eligible for both and you select a Silver-level plan through Nevada Health Link (APTC can be used with plans at any metal level, but CSR benefits are only available on Silver plans).
Public option with reinsurance coming in 2026
Nevada S.B.420, signed into law in June 2021,18 calls for the state to create a public option health plan that will be available in the individual market as of 2026. The idea is to create premium reduction targets, similar to the approach that Colorado is using.
Gov. Lombardo, who took office in 2023, has long been critical of the public option approach, and is working to transform it into a “market stabilization program” instead. Under Lombardo’s plan there will still be a public option component, with a quality incentive payment program for insurers to prevent reimbursement cuts for medical providers due to the premium reduction targets. Lombardo’s plan also calls for a reinsurance program that would use federal funding to reduce premiums in the individual market.19 (Reinsurance programs are already in use in 17 states.)
Depending on your income and circumstances, you may be able to enroll in free or low-cost health coverage through Medicaid or Check Up (Nevada’s CHIP). You can learn more about whether you might meet the criteria for Medicaid in Nevada.
How many insurers offer Marketplace coverage in Nevada?
For 2024 coverage, eight insurers offer a total of 163 Marketplace/exchange plans in Nevada, with coverage areas that vary from one insurer to another.20 This includes two carriers that are new for 2024: Imperial Insurance Companies and Molina Healthcare of Nevada.[enf_note]Nevada: *Final* Avg. Unsubsidized 2024 #ACA Rate Changes: +3.8%; Molina & Imperial Joining Market. ACA Signups. October 2023.[/efn_note]
Are Marketplace health insurance premiums increasing in Nevada?
For 2024 coverage, the following average rate changes were implemented (calculated before any subsidies are applied):21
Nevada’s ACA Marketplace Plan 2024 Approved Rate Increases by Insurance Company |
|
|---|---|
| Issuer | Percent Increase |
| Anthem Blue Cross Blue Shield (HMO Nevada) | -4.2% |
| Health Plan of Nevada | 4.8% |
| SelectHealth | 5% |
| Silver Summit | 6.4% |
| Aetna Health | 1.16% |
| Hometown Health Plan | -8.34% |
| Imperial Insurance Companies | New for 2024 |
| Molina Healthcare of Nevada | New for 2024 |
Source: Nevada Division of Insurance22
For plans sold via Nevada Health Link, the approved rate changes for 2024 amount to an overall average rate increase of 2.8%, before any subsidies are applied (for the entire individual market, including plans sold only outside the exchange, the average rate increase was 3.6%).2
It’s important to remember that these average rate increases are for full-price plans, and most enrollees do not pay full price: As of 2023, 86% of Nevada Health Link enrollees were receiving premium subsidies that reduced their monthly payments.17
The subsidy amount is different for each enrollee and changes each year depending on the cost of the second-lowest-cost Silver plan relative to the enrollee’s household income. As a result of the American Rescue Plan and the Inflation Reduction Act, subsidies are larger and more widely available than they were in the past, and that will continue to be true at least through 2025.23
Changes in full-price premiums depend on the insurer and the plan (premium changes vary across the plans that each insurer offers), as well as the enrollee’s age and zip code.
For people who receive premium tax credits – which includes the vast majority of Nevada Health Link enrollees – the net premium change also depends on how much the subsidy amount changes from one year to the next.
Here’s an overview of how average full-price premiums have changed over the years in Nevada’s individual/family market:
- 2015: Average increase of 4%.24
- 2016: Average increase of 9.6%.25
- 2017: Average increase of 10.6%.26
- 2018: Average increase of 38.2%.27
- 2019: Average increase of 0.4%.28
- 2020: Average increase of 1.7%.29
- 2021: Average increase of 4.9%.30
- 2022: Average increase of 4.1%.31
- 2023: Average increase of 9.2%.32
How many people are insured through Nevada’s Marketplace?
According to Centers for Medicare & Medicaid Services (CMS) data, 95,930 people selected private plans through Nevada Health Link during the open enrollment period for 2023 coverage.33
Effectuated enrollment is always a little lower than the number of people who select plans during open enrollment. CMS reported that effectuated enrollment through Nevada Health Link stood at 93,262 people as of early 2023.17
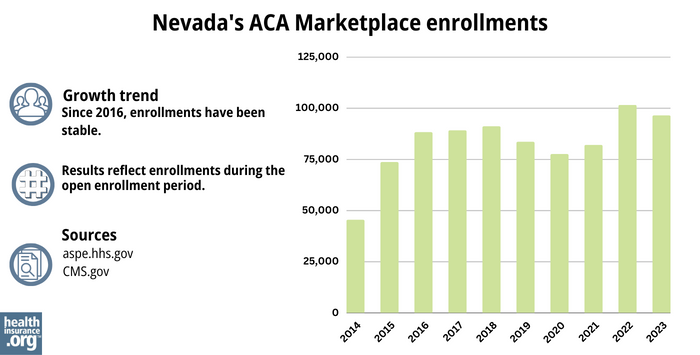
Source: 2014,34 2015,35 2016,36 2017,37 2018,38 2019,39 2020,40 2021,41 2022,42 2023 43
What health insurance resources are available to Nevada residents?
Nevada Health Link: This is Nevada’s Marketplace, used to enroll in individual/family health plans and receive income-based subsidies. You can contact Nevada Health Link at 800-547-2927.
Nevada Department of Health and Human Services: The Nevada Department of Health and Human Services (DHHS) administers Medicaid and Check Up (CHIP), as well as other social services programs. You can reach Nevada DHHS by phone at (775) 684-4000 or by email at [email protected]
Nevada Division of Insurance: Regulates Nevada’s insurance industry, and assists consumers and businesses with insurance-related questions and concerns.
Nevada State Health Insurance Assistance Program: A local service for Medicare beneficiaries and their caregivers. Provides information and assistance with questions related to Medicare eligibility, enrollment, and claims.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- “Silver State Health Insurance Exchange” nevadahealthlink.com, Accessed August 2023 ⤶
- OCTOBER 2, 2023 – Discover Your Best Health Plan: 2024 Rates and Options Now Available. Nevada Division of Insurance. October 2023. ⤶ ⤶
- “Nevada Medicaid Fact Book” NV.gov, Accessed August 2023 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”KFF.org, April 2023 ⤶
- “Medicare Monthly Enrollment” CMS.gov, April 2023 ⤶
- “Availability of short-term health insurance in Nevada” healthinsurance.org, Aug. 14, 2023 ⤶
- ”Who can use Nevada Health Link?” Nevada Health Link, Accessed August 2023 ⤶
- Medicare and the Marketplace, Master FAQ. Centers for Medicare and Medicaid Services. Accessed November 2023. ⤶
- Medicare and the Marketplace, Master FAQ. Centers for Medicare and Medicaid Services. Accessed November 2023. ⤶
- Nevada deadline confirmed via email with Nevada Health Link’s communications department in November 2023 ⤶
- “How to Enroll” Nevada Health Link, Access August 2023 ⤶
- “Who doesn’t need a special enrollment period?“ healthinsurance.org, Accessd August 2023 ⤶
- Nevada Senate Bill 482. BillTrack50. Enacted May 2019. ⤶
- “Entities Approved to Use Enhanced Direct Enrollment” CMS.gov, April 28, 2023 ⤶
- ”2023 OEP State-Level Public Use File” CMS.gov, March 23, 2023 ⤶
- ”2023 OEP State-Level Public Use File” CMS.gov, March 23, 2023 ⤶
- “Effectuated Enrollment: Early 2023 Snapshot and Full Year 2022 Average“CMS.gov, March 15, 2023 ⤶ ⤶ ⤶
- Nevada Senate Bill 420. BillTrack50. Enacted June 2021. ⤶
- Governor Joe Lombardo Announces Plan to Transform the Nevada Public Option into Market Stabilization Program. Nevada Governor Joe Lombardo. October 2023. ⤶
- Plan Year 2024 Open Enrollment Period Health Insurance Plans and Rates Are Available Now on NevadaHealthLink.com. Nevada Health Link. October 2023. ⤶
- “Health Insurance Rate Change Search Results”Nevada Division of Insurance, Accessed August 2023 ⤶
- Health Insurance Rate Change Search Results. Nevada Division of Insurance, Accessed December 2023 ⤶
- “Health Insurance Marketplaces 2023 Open Enrollment Report”CMS.gov, Accessed August 2023 ⤶
- Analysis Finds No Nationwide Increase in Health Insurance Marketplace Premiums. The Commonwealth Fund. December 2014. ⤶
- FINAL PROJECTION: 2016 Weighted Avg. Rate Increases: 12-13% Nationally* ACA Signups. October 2015. ⤶
- Avg. UNSUBSIDIZED Indy Mkt Rate Hikes: 25% (49 States + DC). ACA Signups. October 2016. ⤶
- 2018 Rate Hikes. ACA Signups. October 2017. ⤶
- 2019 Rate Hikes. ACA Signups. October 2018. ⤶
- 2020 Rate Changes. ACA Signups. October 2019. ⤶
- 2021 Rate Changes. ACA Signups. October 2020. ⤶
- 2022 Rate Changes. ACA Signups. October 2021. ⤶
- UPDATED: FINAL Unsubsidized 2023 Premiums: +6.2% Across All 50 States +DC. ACA Signups. Accessed November 2023. ⤶
- “Marketplace 2023 Open Enrollment Period Report: Final National Snapshot” CMS.gov, Jan. 25, 2023 ⤶
- “ASPE Issue Brief (2014)” ASPE, 2015 ⤶
- “Health Insurance Marketplaces 2015 Open Enrollment Period: March Enrollment Report”, HHS.gov, 2015 ⤶
- “HEALTH INSURANCE MARKETPLACES 2016 OPEN ENROLLMENT PERIOD: FINAL ENROLLMENT REPORT” HHS.gov, 2016 ⤶
- “2017 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2017 ⤶
- “2018 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2018 ⤶
- “2019 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2019 ⤶
- “2020 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2020 ⤶
- “2021 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2021 ⤶
- “2022 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2022 ⤶
- “Health Insurance Marketplaces 2023 Open Enrollment Report”CMS.gov, Accessed August 2023 ⤶







