Home > States > Health insurance in Texas
See your Texas health insurance coverage options.

Find individual and family plans, small-group, short-term or Medicare plans through licensed agency partners.

Texas Health Insurance Consumer Guide
This guide was developed to assist you in choosing the right Texas health insurance plan for you and your family. The coverage options found in Texas’s ACA Marketplace may be a good choice for many consumers, and we will guide you through the options below.
Texas uses the federally run health insurance exchange (Marketplace), HealthCare.gov, for residents to purchase its ACA Marketplace plans. The Marketplace provides access to health insurance products from numerous private insurers (coverage areas vary from one insurer to another; most areas of the state have plans available from multiple insurers, but there are some counties in north-central Texas where only a single insurer offers Marketplace coverage).1
Depending on your income and other circumstances, you may qualify for financial assistance through the Marketplace which can reduce your monthly insurance premium (the amount you pay to enroll in the coverage) and possibly your out-of-pocket expenses.
Texas implemented a new rule — for coverage effective in 2023 and future years — requiring health insurers to add a 35% load to the cost of silver plans to account for CSR.2 This effectively makes silver plan prices higher than most gold plan prices, resulting in larger subsidies and even more affordable premiums for bronze and gold plans.3
Explore our other comprehensive guides to coverage in Texas
Dental coverage in Texas

Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Texas.

Texas’s Medicaid program

Texas has not expanded Medicaid eligibility under the Affordable Care Act (ACA). As a result, Texas has the biggest coverage gap in the country, impacting an estimated 771,000 residents.4 The number of Medicaid beneficiaries in Texas has grown to more than 5 million people.5

Medicare coverage in Texas

Over 4.5 million people are enrolled in Medicare plans in Texas.6 Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Texas as well as the state’s Medicare supplement (Medigap) regulations.

Short-term coverage in Texas

As of 2023, there were at least six insurers selling short-term health insurance plans in Texas.7

Frequently asked questions about health insurance in Texas
Who can buy Marketplace health insurance?
To qualify for health coverage through the Texas Marketplace, you must:
- Live in Texas
- Be lawfully present in the United States
- Not be incarcerated
- Not be enrolled in Medicare
Eligibility for financial assistance (premium subsidies and cost-sharing reductions) depends on your income. In addition, to qualify for financial assistance with your Marketplace plan you must:
- Not have access to affordable health coverage offered by an employer. If your employer offers coverage but you feel it’s too expensive, you can use our Employer Health Plan Affordability Calculator to see if you might qualify for premium subsidies in the Marketplace.
- Not be eligible for Medicaid or CHIP.
- Not be eligible for premium-free Medicare Part A.8
When can I enroll in an ACA-compliant plan in Texas?
In Texas, you can sign up for an ACA-compliant individual or family health plan from November 1 to January 15 during open enrollment.9
If you need your coverage to start on January 1, you must apply by December 15. If you apply between December 16 and January 15, your coverage will begin on February 1.10
Outside of open enrollment, a special enrollment period (typcailly linked to a specific qualifying life event) is necessary to enroll or make changes to your coverage.
If you have questions about open enrollment, you can learn more in our comprehensive guide to open enrollment. We also have a comprehensive guide to special enrollment periods.
How do I enroll in a Texas Marketplace plan?
To enroll in an ACA Marketplace plan in Texas, you can:
- Visit HealthCare.gov, the Texas health insurance marketplace.
- Purchase individual and family health coverage with the help of an insurance agent or broker, a Navigator or certified application counselor, or an approved enhanced direct enrollment entity.11
You can also call HealthCare.gov’s contact center by dialing 1-800-318-2596 (TTY: 1-855-889-4325). The call center is available 24 hours a day, seven days a week, but it’s closed on holidays.
How can I find affordable health insurance in Texas?
Texas uses the federally run exchange for individual market plans, so residents who buy their own health insurance enroll through HealthCare.gov.
In the Texas marketplace, nearly nine out of ten eligible enrollees who purchased health plans for 2023 saved money on premium payments amounting to an average savings of $539/month. With the help of these subsidies, enrollees paid premiums of $43/month on average.12
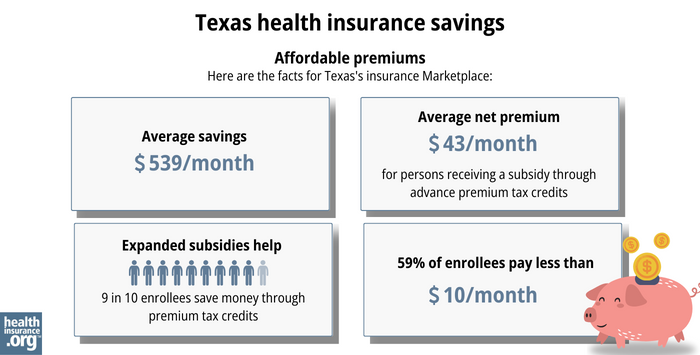
Source: CMS.gov12
In addition to premium subsidies, the Affordable Care Act also includes cost-sharing reductions (CSR), which help to reduce out-of-pocket costs on Silver-level plans for people with household income up to 250% of the poverty level.13
Between the premium subsidies and cost-sharing reductions, you may find that an ACA plan is the cheapest health insurance option for you.
And as noted above, Texas requires health plans to charge higher premiums for Silver-level plans2 (to account for the loss of federal CSR funding, but in a uniform manner).
The result is that it’s common to see Gold plans priced lower than Silver plans. If you’re not eligible for CSR, this can make a Gold plan a particularly good value in Texas.3 (If you are eligible for CSR, you’ll want to carefully consider Silver plans, as you’ll forfeit your CSR benefit if you don’t select a Silver plan.)
Texas has not expanded Medicaid under the ACA, so there is still a coverage gap in the state. An estimated 772,000 people are in the coverage gap in Texas, which means they earn less than the poverty level, are not eligible for Medicaid (due to lack of Medicaid expansion in Texas), and are also not eligible for subsidies in the Marketplace because their income is under the poverty level.14
As a result of the Affordable Care Act, federal law only allows a self-employed married couple to purchase small group health insurance if there is at least one additional employee. Even if both spouses work for their business, they aren’t considered to be two separate employees (and thus eligible for group health coverage, which requires at least two employees) under federal law. But Texas law is different, and takes precedence in this case. In Texas, a small group insurer must issue coverage to any group of two or more employees, even if the group only has two employees who are married to each other.15
So if you and your spouse are self-employed together, you can consider Texas small group plans as well as individual market plans. Marketplace subsidies are not available for small group plans, but you might find that there are factors that make the small group plans preferable (such as the provider network), especially if you’re not eligible for Marketplace subsidies due to your income.
How many insurers offer Marketplace coverage in Texas?
The Texas individual/family Marketplace has 16 participating insurers that offer coverage for 2024,16 although plan participation varies from one area to another.
In most Texas counties, at least three insurers are offering health plans on the exchange in 2024, although some counties in the north-central part of the state only have plans available from one insurer. But there are also numerous counties where five or more insurers offering Marketplace plans.1
Are Marketplace health insurance premiums increasing in Texas?
In the Texas individual/family health insurance market, insurance companies have implemented the following average rate changes for 2024, applicable to full-price (pre-subsidy) premiums,16 which amount to a weighted average rate increase of about 5.3%:17
Texas’ ACA Marketplace Plan 2024 Approved Rate Increases by Insurance Company |
|
|---|---|
| Issuer | Percent Increase |
| Aetna/CVS | 14.94% |
| Celtic/Ambetter | 5.53% |
| Superior Health Plan/Ambetter | 4.93% |
| Blue Cross Blue Shield of Texas | -0.24% |
| CHRISTUS | -1.42% |
| Community First Insurance Plans * | 4.73% |
| Community Health Choice | 6.90% |
| Moda | 9.39% |
| Molina | 8.23% |
| Oscar | 3.39% |
| Sendero | -10.54% |
| Scott & White Health Plan ** | 1.20% |
| UnitedHealthcare | 4.99% |
| Ascension Personalized Care (US Health and Life Insurance) | 13.40% |
| Cigna | 12.40% |
| Imperial Insurance Companies | 10.98% |
Source: Texas Rate Review Submissions16
*Community First Health Plans policies are not available to new enrollees during the open enrollment period for 2024, as enrollments are suppressed due to network issues until May 2024. But existing CFHP policies are not affected, and will renew for 2024.
**FirstCare’s individual/family plans are no longer available in Texas as of 2024.18 FirstCare was bought by Scott & White Health in 2019.19 FirstCare enrollees have the option of switching to any available plan in their area for 2024, even if they’re automatically transitioned to a Scott & White plan.
Prior to the 2023 plan year, Texas did not have an effective rate review program, so the federal government reviewed insurers’ rate proposals in Texas. But that changed as of the 2023 plan year, and the Texas Department of Insurance now handles rate review for individual/family health plans.20
For perspective, here’s an overview of how full-price (pre-subsidy) premiums have changed in the Texas individual/family market over the years:
- 2015: Average increase of 5%.21
- 2016: Average increase of 15.8%.22
- 2017: Average increase of 34%.23
- 2018: Average increase of 32.5%.24
- 2019: Average increase of 2.3%.25
- 2020: Average decrease of 1.4%.26
- 2021: Average increase of 7.4%.27
- 2022: Average rate increase of 3%.28
- 2023: Average increase of 4.9%.29
How many people are insured through Texas’s Marketplace?
Enrollment was far higher in the Texas marketplace in 2023 than in any previous year: During the 2023 open enrollment period, more than 2.4 million people enrolled in private plans.12 And that came on the heels of a previous record high in 2022.30
The surge in enrollment during these years is likely due to the American Rescue Plan (ARP). Under the ARP, ACA’s premium subsidies are more significant and widely available.31 The ARP’s subsidy enhancements have been extended through 2025 by the Inflation Reduction Act.
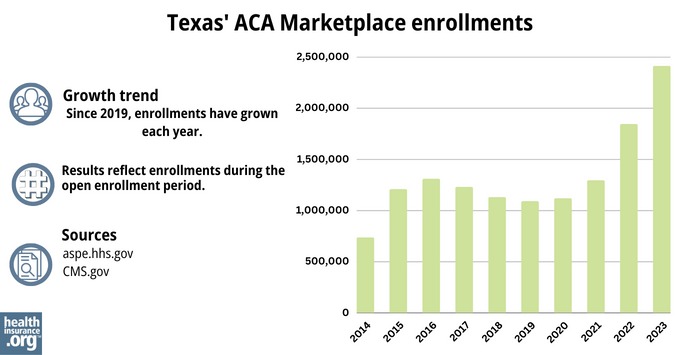
Texas health insurance Marketplace enrollments
Source: 2014,32 2015,33 2016,34 2017,35 2018,36 2019,37 2020,38 2021,39 2022,40 202312
What health insurance resources are available to Texas residents?
HealthCare.gov
800-318-2596
Texas Health Plan Compare (a service of the Texas Department of Insurance)
State Exchange Profile: Texas
The Henry J. Kaiser Family Foundation overview of Texas’ progress toward creating a state health insurance exchange.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- Plan Year 2024 Qualified Health Plan Choice and Premiums in HealthCare.gov Marketplaces. Centers for Medicare and Medicaid Services. October 25, 2023. ⤶ ⤶
- ACA Rating Rule. Texas Department of Insurance. April 2022. ⤶ ⤶
- How the Texas Legislature Learned to Stop Worrying and Love the ACA Marketplace. Sprung, Andrew. The American Prospect. April 2022. ⤶ ⤶
- “How Many Uninsured Are in the Coverage Gap and How Many Could be Eligible if All States Adopted the Medicaid Expansion?” KFF.org, March 31, 2023 ⤶
- “Medicaid & CHIP Enrollment Data Highlights” Medicaid.gov, April 2023 ⤶
- “Medicare Monthly Enrollment" CMS.gov, April 2023. ⤶
- “Availability of short-term health insurance in Texas” healthinsurance.org, Jan. 11, 2023 ⤶
- Medicare and the Marketplace, Master FAQ. Centers for Medicare and Medicaid Services. Accessed November 2023. ⤶
- “When can you get health insurance?” HealthCare.gov, 2023 ⤶
- “A quick guide to the Health Insurance Marketplace®” HealthCare.gov, Accessed August, 2023 ⤶
- “Entities Approved to Use Enhanced Direct Enrollment” CMS.gov, April 28, 2023 ⤶
- “2023 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2023 ⤶ ⤶ ⤶ ⤶
- APTC and CSR Basics. Centers for Medicare and Medicaid Services. June 2023. ⤶
- How Many Uninsured Are in the Coverage Gap and How Many Could be Eligible if All States Adopted the Medicaid Expansion? KFF. March 2023. ⤶
- Frequently Asked Questions for Health Carriers. Guaranteed Issuance and Renewability for Mom and Pop Groups. Texas Department of Insurance. Accessed December 2023. ⤶
- “Texas Rate Review Submissions” HealthCare.gov, 2023 ⤶ ⤶ ⤶
- So How’d I Do On My 2024 Avg. Rate Change Project? Not Bad At All! ACA Signups. December 2023. ⤶
- FirstCare to discontinue individual and family plans in 2024. FirstCare. Accessed December 2023. ⤶
- Scott and White Health Plan Acquires FirstCare Health Plans. FirstCare. January 2019. ⤶
- Texas Rate Review Requirements for Health Benefit Plans. Texas Department of Insurance. Accessed December 2023. ⤶
- Analysis Finds No Nationwide Increase in Health Insurance Marketplace Premiums. The Commonwealth Fund. December 2014. ⤶
- FINAL PROJECTION: 2016 Weighted Avg. Rate Increases: 12-13% Nationally* ACA Signups. October 2015. ⤶
- Avg. UNSUBSIDIZED Indy Mkt Rate Hikes: 25% (49 States + DC). ACA Signups. October 2016. ⤶
- 2018 Rate Hikes. ACA Signups. October 2017. ⤶
- Texas: FINAL/APPROVED 2019 #ACA Rate Hikes: 2.3%, But WOULD Likely Have DROPPED 8% W/Out #ACASabotage. ACA Signups. November 2018. ⤶
- Texas: *Final* Avg. 2020 #ACA Premiums: 1.4% Decrease. ACA Signups. October 2019. ⤶
- 2021 Rate Changes. ACA Signups. October 2020. ⤶
- *APPROVED* Avg. 2022 #ACA Rate Changeapalooza! AK, CA, GA, HI, IL, KS, LA, MA, MS, MO, NE, NH, TX, WY. ACA Signups. November 2021. ⤶
- Texas: Average Unsubsidized 2023 #ACA Rate Increases Drop From 8.8% To 4.9% “Thanks” To Bright & Friday Leaving… ACA Signups. October 2022. ⤶
- “2022 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2022 ⤶
- “Health Insurance Marketplaces 2023 Open Enrollment Report” CMS.gov, Accessed August 2023 ⤶
- “ASPE Issue Brief (2014) ASPE, 2015 ⤶
- Health Insurance Marketplaces 2015 Open Enrollment Period: March Enrollment Report, HHS.gov, 2015 ⤶
- “HEALTH INSURANCE MARKETPLACES 2016 OPEN ENROLLMENT PERIOD: FINAL ENROLLMENT REPORT” HHS.gov, 2016 ⤶
- “2017 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2017 ⤶
- “2018 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2018 ⤶
- “2019 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2019 ⤶
- “2020 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2020 ⤶
- “2021 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2021 ⤶
- “2022 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2022 ⤶







