Medicaid eligibility and enrollment in Wisconsin

Wisconsin is the only non-expansion state without a coverage gap

Who is eligible for Medicaid in Wisconsin?
In Wisconsin, BadgerCare Plus refers to Medicaid coverage for low-income children, pregnant women, and adults under 65.1 These populations can qualify for coverage based on household income (MAGI), regardless of assets. For older adults and people with disabilities, the coverage is simply called Medicaid, and it has both income and asset limits. BadgerCare Plus or Medicaid is available for the following legally present Wisconsin residents:2
- Pregnant women with household income up to 300% of poverty. (Coverage for the mother continues for 60 days after the birth, although Wisconsin is seeking a waiver to allow this to continue for 90 days,3 And state lawmakers are considering bipartisan legislation in 2025 that would extend postpartum Medicaid to last for a year after the baby is born.4 Almost all states have already extended postpartum coverage to a full year.5)
- Children 19 and under with household income up to 300% of poverty.
- Adults with household income up to 100% of poverty (as described below, Wisconsin has not implemented the ACA’s Medicaid expansion, but does cover adults with income up to the poverty level, so there’s no coverage gap in Wisconsin). Non-refugee/asylee adults must be lawfully present in the U.S. for at least five years before becoming eligible for Medicaid.
- People with low income and low assets who are 65+, blind, or disabled
Apply for Medicaid in Wisconsin
Online at access.wisconsin.gov or healthcare.gov; or by phone, in person or with a paper application at local Income Maintenance Agencies.
Eligibility: The aged, blind, and disabled. Also, children and pregnant women with incomes up to 300% of poverty; other adults with incomes up to 100% of poverty.



No ACA Medicaid expansion in Wisconsin, but no coverage gap either
Although Wisconsin has not expanded Medicaid under the guidelines laid out in the Affordable Care Act (ACA), the state’s Medicaid program (which is called BadgerCare) does cover all non-elderly adults with incomes under the poverty level (to be eligible, immigrants must have been lawfully present in the U.S. for at least five years; those who have been in the country less than that are eligible for Marketplace subsidies instead).
As of January 2025, almost 198,000 non-disabled adults without minor children were enrolled in BadgerCare Plus (Wisconsin Medicaid).6 In the rest of the states that have not expanded Medicaid, these individuals would not be eligible for Medicaid, and would instead be in the coverage gap.
Wisconsin is the only non-Medicaid-expansion state that does not have a coverage gap; all low-income residents either have access to Medicaid or subsidies to help them purchase private coverage in the Marketplace.
(Georgia implemented a similar partial expansion of Medicaid in mid-2023, but Georgia’s program has a work requirement so it’s much less accessible to low-income residents.)
Premium subsidies in the Marketplace are only available if a person’s income is at least equal to the poverty level. In most states, subsidy eligibility actually starts above 138% of the poverty level, as Medicaid expansion covers adults with income up to that level. But 10 states have not expanded Medicaid under the ACA. Wisconsin is one of them, but Wisconsin does make Medicaid available to adults with income up to the poverty level. So there’s a seamless transition from Medicaid eligibility to premium subsidy eligibility in Wisconsin.
That’s not the case in the other nine states that have not expanded Medicaid (with the partial exception of Georgia, as adults who are below the poverty level but also fulfilling a work requirement are now eligible for Medicaid7). Instead, Medicaid for adults under 65 is not available at all in those states unless a person is disabled, pregnant, or caring for a minor child. And the income limits for parents tend to be quite low — well below the poverty level.
Wisconsin’s approach ensures there’s no coverage gap, but it’s also expensive for the state. Because Wisconsin hasn’t fully expanded Medicaid eligibility to 138% of the poverty level, the state is only receiving its normal federal Medicaid funding. If it were to expand Medicaid, the federal government would start to pay 90% of the cost of covering the Medicaid expansion population, including the adults with income up to the poverty level who are already covered under Wisconsin Medicaid.
There’s also a provision in the American Rescue Plan that would provide additional federal funding for a state that newly expands Medicaid, which would make it even more financially beneficial to the state. In total, Wisconsin would get $1.6 billion in federal funding over the next two years by expanding Medicaid to 138% of the poverty level, and Governor Evers has continued to push for Medicaid expansion. but the Wisconsin budget committee has continued to reject Medicaid expansion proposals, despite the financial benefits it would provide to the state.
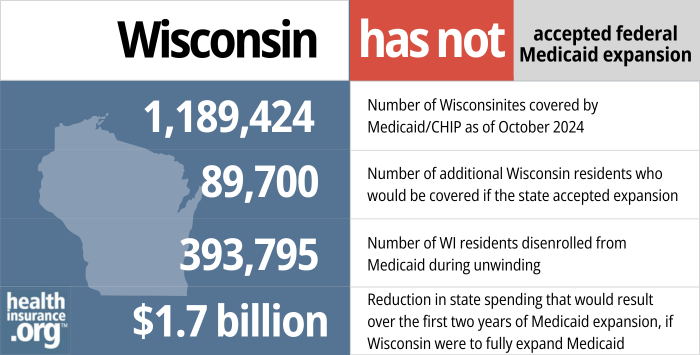
- 1,189,424 – Number of Wisconsinites covered by Medicaid/CHIP as of October 20248
- 89,700 – Number of additional Wisconsin residents who would be covered if the state accepted Medicaid expansion9
- 393,795 – Number of WI residents disenrolled from Medicaid during the unwinding process10
- $1.7 billion – Reduction in state spending that would result over the first two years of Medicaid expansion, if Wisconsin were to fully expand Medicaid.11
Explore our other comprehensive guides to coverage in Wisconsin

We’ve created this guide to help you understand the Wisconsin health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Wisconsin.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Wisconsin as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.

Frequently asked questions about Wisconsin Medicaid
How do I enroll in Medicaid in Wisconsin?
- You can enroll online at Wisconsin ACCESS (you can also start the process at HealthCare.gov, and will be referred to the state Medicaid agency if it appears you’re eligible for that coverage).
- You can also enroll in person or by phone at a local Wisconsin Income Maintenance Agency (this map shows the agency for each region – you can click on your region and it will show you the address and phone number of your local office).
- You can print a paper application and take it to your local Income Maintenance Agency or submit it by mail (the address to use depends on whether you live in Milwaukee County or not).
How does Medicaid provide financial help to Medicare beneficiaries in Wisconsin?
Many Medicare beneficiaries receive assistance from Medicaid with Medicare premiums, prescription drug costs, and expenses not covered by Medicare – including long-term care.
Our guide to financial assistance for Medicare enrollees in Wisconsin includes overviews of these benefits, including Medicare Savings Programs, Medicaid nursing home coverage, and eligibility guidelines for assistance.
How many Wisconsin residents were disenrolled from Medicaid after the pandemic?
From March 2020 through March 2023, Medicaid disenrollments were paused nationwide, even if a person’s circumstances changed and they no longer met the Medicaid eligibility guidelines.
That ended March 31, 2023, however, and states could resume disenrollments as early as April 1, 2023. During a one-year “unwinding” period, states had to redetermine eligibility for everyone enrolled in Medicaid.
The first round of disenrollments in Wisconsin came at the end of June 2023. By the end of the year-long unwinding process, 393,795 Wisconsin residents had been disenrolled from Medicaid, while Medicaid coverage had been renewed for just over one million enrollees.12
Total enrollment in BadgerCare Plus and Medicaid had reached a high of 1,676,787 in May 2023, and then began to decline at the end of June. By mid-2024, enrollment stood at about 1.2 million,12 and it was still roughly at that level by late 2024.8
See Wisconsin’s renewal data dashboard, and a summary of month-by-month enrollment numbers during the unwinding process.
People disenrolled from Medicaid could switch to employer-sponsored coverage if it was available, or to a self-purchased plan in the Wisconsin Marketplace (HealthCare.gov). CMS reported that 71,778 Wisconsin residents transitioned from Medicaid to a Marketplace plan during the unwinding process.13
Wisconsin Medicaid history and details
BadgerCare Reform Demonstration was suspended due to COVID-19
Former Governor Scott Walker, who was opposed to the ACA, opted not to accept federal funding for Wisconsin Medicaid expansion under the ACA, in part because he was concerned that the federal government would not keep its promise to continue to pay at least 90% of the cost. But because Wisconsin has not expanded Medicaid, the state is only receiving its regular federal match rate of 60.4%,14 and the state is paying the rest.
If the state were to expand Medicaid to cover adults earning up to 138% of the poverty level, the federal government would pay 90% of the cost of covering able-bodied, childless adults — including the almost 198,000 non-disabled adults without minor children who are already enrolled in BadgerCare Plus.6
A 2020 analysis by the Robert Wood Johnson Foundation estimated that 120,000 people would gain access to Medicaid if the state were to accept federal funding to fully expand coverage, and that the state’s uninsured rate would drop by 16%. And because Wisconsin is currently covering adults with income up to the poverty level under the state’s regular state/federal funding split, Wisconsin is the only non-expansion state that would see a direct reduction in state spending by expanding Medicaid (since the federal government would start to pay 90% of the cost of covering the entire Medicaid expansion population, including non-disabled adults with income under the poverty level who are already covered under the state’s non-expansion approach).
Wisconsin’s approach means that the state has essentially expanded Medicaid using its own funds. Georgia is the only other state that has taken a similar approach, although Georgia’s work requirement ensures that only a fraction of adults with income under the poverty level will actually qualify for Medicaid. Utah attempted to get enhanced federal funding for a partial expansion of Medicaid (up to 100% of the poverty level, similar to Wisconsin’s approach), but was unsuccessful. Utah ultimately implemented full Medicaid expansion and is now receiving the enhanced federal funding.
Governor Tony Evers, who took office in early 2019, wants to expand Medicaid in Wisconsin but lawmakers have thus far rejected that option.
Learn how states that expanded Medicaid might reduce spending on Medicaid.
In June 2017, Wisconsin submitted a proposed 1115 waiver to CMS, detailing reforms the state wanted to make to its existing Medicaid program for childless adults ages 19-64. The proposed changes were called for under the terms of the 2015-2017 budget bill (Act 55) that the state enacted. CMS approved the waiver in October 2018, but with some modifications. And the state submitted a proposal in late 2020, seeking permission to amend the BadgerCare Reform Demonstration by adding a health savings account component; that request was still pending federal approval as of 2025.15
The state’s reforms for childless adult BadgerCare Plus enrollees were slated to take effect in 2020. But in response to the COVID-19 pandemic, Wisconsin enacted Assembly Bill 1038 (Act 185) in April 2020, implementing a wide range of measures. Section 105 of the legislation allowed the state to suspend or delay the reforms called for the BadgerCare Reform Demonstration. This enabled Wisconsin to comply with federal requirements for the state to receive the additional federal Medicaid funding that was provided to states to address the pandemic (to receive the funding, states could not impose new premiums or disenroll people from Medicaid between March 2020 and March 2023; new premiums and a work requirement would have run counter to those rules).
And in April 2021, CMS notified Wisconsin that the federal government was revoking its approval for the community engagement (work) requirement portion of the BadgerCare Reform Demonstration. Here’s a look at what else is in the demonstration project, if and when the state can implement the changes:
The 2018 waiver approval extends Wisconsin Medicaid through the end of 2023, and although it initially allowed the state to implement a work requirement for enrollees aged 19 to 49 (that approval has since been revoked), CMS did not approve the state’s proposal to require drug testing as a condition of eligibility for Medicaid. Instead, Wisconsin revised its proposal to include the completion of a health risk assessment as a condition of eligibility. People can be referred for substance abuse treatment based on their health risk assessments, but would not lose their Medicaid eligibility for Medicaid (the substance use disorder monitoring protocol has received specific federal approval).
The state has an FAQ page about the waiver extension and amendment. The approved changes include:
- A Medicaid premium of $8 per month for childless adults with household income between 51 and 100% of the poverty level. There is an option for enrollees to reduce this premium by half if they either don’t engage in behaviors that create a health risk, or if they do but also attest to managing the behavior to improve their health. Healthy behaviors include things like wearing a seat belt, avoiding tobacco products, and maintaining a healthy weight. The premium requirements have been suspended during the COVID-19 pandemic, in order to allow the state to receive additional federal Medicaid funding. Although new premiums (and disenrollments) are once again allowed under federal rules as of April 2023, Wisconsin’s Medicaid handbook indicates that the premiums were still suspended as of August 2023.
- An $8 copay for non-emergency use of the emergency department.
- Completion of a health and wellness questionnaire as a condition of eligibility. This replaced the originally proposed drug screening/testing as a condition of eligibility. Although enrollees whose questionnaire answers indicate a need for drug treatment can be referred to treatment options, they will not lose their eligibility for coverage. The health assessment program was also suspended during the COVID-19 pandemic.
- Increased coverage for substance abuse treatment, including full residential treatment as an option for all BadgerCare members.
- The work requirement portion of the BadgerCare Reform Demonstration has been eliminated altogether. It was designed to limit Wisconsin Medicaid eligibility to 48 months for non-disabled, non-pregnant enrollees age 19 to 49. After a person reached a total of 48 months of coverage, Wisconsin Medicaid eligibility would have ceased for six months. However, any month during which a Wisconsin Medicaid enrollee was working or engaged in work training for at least 80 hours would not count towards the 48-month limit. Coverage in Wisconsin for childless, non-disabled adults is limited to those with income under the poverty level ($14,580 for a single adult in 2023), so avoiding the lifetime benefit cap while continuing to receive benefits would have involved working enough to satisfy the 80-hour-per-month requirement, while not earning more than $14,580 during the year (the poverty level is adjusted slightly higher each year). But implementation of the work requirement was delayed as a result of COVID-19, and the work requirement approval was entirely revoked by the Biden administration in April 2021.
Wisconsin Medicaid history
Prior to 2014, Wisconsin Medicaid had much more generous eligibility guidelines than programs in most other states. It was still limited to children, pregnant women, and parents with dependent children, but it covered them with incomes up to 200% of poverty level (300% for children and pregnant women).
Medicaid expansion under the ACA would have extended Medicaid coverage to everyone — including adults without dependent children — with incomes up to 138% of poverty. But the Supreme Court ruled in 2012 that states could not be penalized if they didn’t expand their programs, and Wisconsin’s former Governor Scott Walker saw an opportunity to revamp the state’s Medicaid program, providing access to coverage for everyone while relying as much as possible on private coverage.
ACA subsidies to purchase private plans in the exchange are only available to people with incomes of at least 100% of the poverty level. So Governor Walker decided to make Wisconsin Medicaid available to everyone with incomes up to 100% of the poverty level (pregnant women and children are still eligible with household incomes up to 300% of poverty level). This meant that about 83,000 adults without dependent children became newly eligible for Wisconsin Medicaid on April 1, 2014.
But in trade, Walker’s plan called for switching to private coverage through the exchange for about 72,000 residents with incomes between 100% and 200% of poverty level. This group was comprised almost entirely of parents with dependent children, and they were eligible for Wisconsin Medicaid under the old rules. Although this group is now eligible for significant subsidies in the exchange, there are concerns among consumer advocates that the people who were previously insured through Wisconsin Medicaid might not have been able to afford private coverage in the exchange (including the out-of-pocket costs for claims), even with subsidies.
For the people who lost Medicaid eligibility, the exchange provided a special enrollment period that ran through the end of June 2014. But by September 2014, the state estimated that there were still 28,500 former Wisconsin Medicaid enrollees who had not enrolled in coverage through the exchange. As a result, a new special enrollment period was enacted, running from September 4 to November 2, 2014. Ultimately, the state estimated that less than 60% of the people who lost access to Medicaid were able to transition to a private plan in Wisconsin’s exchange.
An expensive choice
By not accepting federal funding to expand Medicaid under the ACA, Wisconsin has missed out on billions in federal funding since the beginning of 2014. If the state had accepted Medicaid expansion to cover adults with income up to 138% of the poverty level, the federal government would have paid 100% of the cost through the end of 2016, and would be paying 90% of the cost in 2020 and beyond. But because Wisconsin cuts off Medicaid eligibility at 100% of the poverty level, they aren’t eligible for the enhanced federal match provided by the ACA.
Under the Obama and Trump administrations, some states proposed expanding Medicaid to 100% of the poverty level with full federal funding. But HHS did not agree to that provision, insisting that to receive ACA Medicaid expansion funding, states had to expand coverage to 138% of the poverty level (133%, with a built-in 5% income disregard).
Because Wisconsin has taken a unique approach to partially expanding Medicaid, they have been paying more in state funds than they would if they had expanded Medicaid as called for in the ACA. According to the Robert Wood Johnson Foundation, Wisconsin’s direct costs for Medicaid would drop by nearly 7% if the state expanded Medicaid, despite the fact that more people would be covered.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Wisconsin?
Explore more resources for options in Wisconsin including ACA coverage, short-term health insurance, dental insurance and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”Badger Care Plus” Wisconsin Department of Health Services. Accessed Feb. 18, 2025 ⤶
- ”Information About Your Enrollment and Benefits” Wisconsin Department of Health Services. Accessed Feb. 18, 2025 ⤶
- ”Wisconsin Postpartum Coverage 1115 Waiver” CMS.gov. Accessed Feb. 18, 2025 ⤶
- ”Wisconsin SB23” BillTrack50. In committee Feb. 5, 2025 ⤶
- ”Medicaid Postpartum Coverage Extension Tracker” KFF.org. Jan. 17, 2025 ⤶
- ”Monthly enrollment by category” Forward Health, Wisconsin Serving You. Data for January 2025. Accessed Feb. 18, 2025 ⤶ ⤶
- ”Georgia Pathways to Coverage” Georgia Department of Community Health. Accessed Feb. 18, 2025 ⤶
- “October 2024 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed January 2025 ⤶ ⤶
- ”GOVERNOR EVERS’ 2023-25 BIENNIAL BUDGET“, WI DHHS, April 2023 ⤶
- ”Medicaid Enrollment and Unwinding Tracker“, KFF.org, August 2024 ⤶
- ”The Picture of Health? Considering Medicaid Expansion in Wisconsin” Wisconsin Policy Forum. Sep. 2024 ⤶
- ”Medicaid Enrollment and Unwinding Tracker” KFF.org. Jan. 31, 2025 ⤶ ⤶
- ”HealthCare.gov Marketplace Medicaid Unwinding Report” Centers for Medicare & Medicaid Services. Data through April 2024. Accessed Feb. 18, 2025 ⤶
- ”EXHIBIT 6. Federal Medical Assistance Percentages (FMAPs) and Enhanced FMAPs (E-FMAPs) by State” MACPAC. Dec. 2024 ⤶
- ”Medicaid: BadgerCare Waiver” Wisconsin Department of Health Services. Accessed Feb. 18, 2025 ⤶

