Home > States > Health insurance in Kentucky
See your Kentucky health insurance coverage options.

Find individual and family plans, small-group, short-term or Medicare plans through licensed agency partners.

Kentucky Health Insurance Consumer Guide
This guide, including the FAQs below, was developed to help you understand the health coverage options available to you and your family in Kentucky. The health plan options offered by Kentucky’s ACA Marketplace may be a good choice for many consumers.
Kentucky residents use a fully state-run health insurance Marketplace – Kynect – to shop for and purchase ACA Marketplace/exchange plans. The Marketplace provides access to health insurance products from private insurers. From 2017 through 2021, Kentucky used the federally-run HealthCare.gov enrollment platform, but reverted to a state-run platform as of the 2022 plan year.
The federal government helps pay for insurance through an income-based advance premium tax credit if you buy coverage from the exchange. Most enrollees qualify for this financial assistance.1
Kentucky had been planning to create a Basic Health Program that would have been operational as of 2024,2 but paused implementation of the BHP in late 2022.3 As of 2023, Minnesota and New York are the only states with BHPs; Oregon plans to join them by mid-2024.4
Explore our other comprehensive guides to coverage in Kentucky
Dental coverage in Kentucky

Looking to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Kentucky.

Kentucky’s Medicaid program

Medicaid expansion in Kentucky took effect in 2014. Since then, the state has been a national leader in lowering uninsured rates and expanding coverage. Kentucky's total Medicaid enrollment has grown to more than 1.5 million people.5

Medicare coverage and enrollment in Kentucky

Medicare enrollment in Kentucky stood at 964,947 people as of April 2023.6

Short-term coverage in Kentucky

In Kentucky, short-term health insurance plans adhere to federal regulations. There were at least nine insurers selling short-term health insurance plans in Kentucky in 2023.7

Frequently asked questions about health insurance in Kentucky
Who can buy Marketplace health insurance?
To qualify for health coverage through the Kentucky Marketplace, you must:8
- Live in Kentucky
- Be lawfully present in the United States
- Not be incarcerated
- Not be enrolled in Medicare
Eligibility for financial assistance (premium subsidies and cost-sharing reductions) depends on your income and how it compares with the cost of the second-lowest-cost Silver plan in your area – which depends on your age and location. In addition, to qualify for financial assistance with your Marketplace plan you must:
- Not have access to affordable health coverage through your employer. If your employer offers coverage but you feel it’s too expensive, you can use our Employer Health Plan Affordability Calculator to see if you might qualify for premium subsidies in the Marketplace.
- Not be eligible for Medicaid or CHIP.
- Not be eligible for premium-free Medicare Part A.9
- File a joint tax return, if you’re married.10 (with very limited exceptions)11
- Not be able to be claimed by someone else as a tax dependent.12
When can I enroll in an ACA-compliant plan in Kentucky?
In Kentucky, the open enrollment period for individual and family health insurance runs from November 1 to January 15.13
Enrollments must be submitted by December 15 to have coverage effective January 1. Enrollments submitted in the final month of the open enrollment window have an effective date of February 1 instead.8
Outside of open enrollment, a special enrollment period (usually linked to a specific qualifying life event) is necessary to enroll or change your coverage. If you have questions about open enrollment, you can learn more in our comprehensive guide to open enrollment. We also have a comprehensive guide to special enrollment periods.
Several bills are under consideration in 2024 in Kentucky that would make pregnancy a qualifying life event.14 Similar legislation was considered in 2023 but did not pass.15
How do I enroll in a Marketplace plan in Kentucky?
To enroll in an ACA Marketplace plan in Kentucky, you can:
- Visit Kynect to access Kentucky’s state-run health insurance Marketplace. Here you will find an online platform to shop, compare, and choose the best health plans.
- Purchase individual and family health coverage with the help of an insurance agent or broker, or a kynector (Kynect-certified enrollment assister).16
How can I find affordable health insurance in Kentucky?
You may find affordable health insurance options in Kentucky through its state-run health insurance exchange. Kentucky residents use Kynect (not HealthCare.gov) to shop, review, and enroll in health coverage as well as to determine any available subsidies.
For residents using the Kentucky exchange, about 83% of eligible enrollees save money on premium payments amounting to an average savings of $495/month in 2023. The subsidies resulted in an average after-subsidy premium of $124/month in 2023.17
People with household incomes of no more than 250% of the federal poverty level also qualify for cost-sharing reductions (CSR). CSR benefits reduce deductibles and other out-of-pocket expenses, as long as the enrollee selects a Silver plan.18
Between the premium subsidies and cost-sharing reductions, you may find that an ACA plan is the cheapest health insurance option for you.
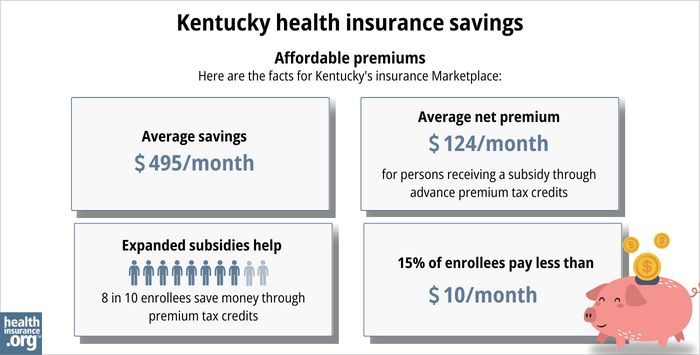
Source: CMS.gov17
How many insurers offer Marketplace coverage in Kentucky?
Are Marketplace health insurance premiums increasing in Kentucky?
The following average rate changes were approved for 2024 for Kentucky’s individual market insurers:20
Kentucky’s ACA Marketplace Plan 2024 Proposed Rate Increases by Insurance Company |
|
|---|---|
| Issuer | Percent Increase |
| Anthem | 6.5% |
| CareSource | 11.5% |
| Ambetter/Wellcare | -1.6% |
| Molina | -2.2% |
For perspective, here’s a summary of how average pre-subsidy premiums have changed in Kentucky’s individual/family market over the years:
- 2015: Average increase of 7%.21
- 2016: Average increase of 14%.22
- 2017: Average increase of 24.5%.23
- 2018: Average increase of 45%.24
- 2019: Average increase of 12.5%.25
- 2020: Average increase of 3.7%.26
- 2021: Average increase of 5%.27
- 2022: Average decrease of 3.8%.28
- 2023: Average increase of 6.25%.29
How many people are insured through Kentucky’s Marketplace?
74,882 people enrolled in private coverage through Kynect during the open enrollment period for 2024 coverage.30
Most states have experienced record-high Marketplace enrollment in 2023 and 2024 — due in large part to the American Rescue Plan (ARP), which expanded enrollee access to ACA’s premium subsidies.31 However, Kentucky has not followed that trend (see chart below for prior year enrollment data).
Enrollment in Kentucky’s Marketplace declined for several years, from 2019 through 2023. Although it did grow in 2024, the enrollment total was still well below the record high set in 2015, before Kentucky transitioned to the HealthCare.gov platform for a few years.
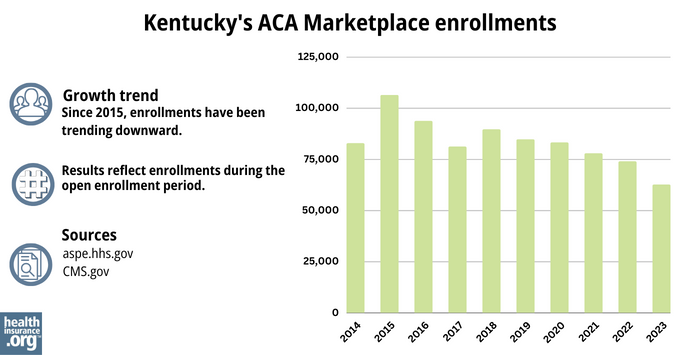
Source: 2014,32 2015,33 2016,34 2017,35 2018,36 2019,37 2020,38 2021,39 2022,40 202317
What health insurance resources are available to Kentucky residents?
Kynect – Kentucky’s Healthcare Connection
855-4kynect (855-459-6328)
Kentucky Health Benefit Exchange
Administrative site for Kentucky’s Marketplace
Foundation for a Healthier Kentucky
Kentucky Health Insurance Advocate, Kentucky Department of Insurance
Assists people insured by private health plans, Medicaid, or other plans in resolving problems pertaining to their health coverage; assists uninsured residents with access to care.
(877) 587-7222 /[email protected]
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- Effectuated Enrollment: Early 2023 Snapshot and Full Year 2022 Average. Centers for Medicare and Medicaid Services. Accessed November 2023. ⤶
- Basic Health Program. Kentucky Cabinet for Health and Family Services. Accessed November 2023. ⤶
- Center for Open Government: Beshear administration hits pause on their “public option” health plan. Bluegrass Institute. December 2022. ⤶
- Basic Health Program (BHP) OHPB Update. Oregon Health Authority. July 2023. ⤶
- “April 2023 Medicaid & CHIP Enrollment Data Highlights” Medicaid.gov, April 28, 2023 ⤶
- “Medicare Monthly Enrollment” CMS.gov, April 2023. ⤶
- “Availability of short-term health insurance in Kentucky” healthinsurance.org, April 6, 2023 ⤶
- ”A quick guide to the Health Insurance Marketplace” HealthCare.gov ⤶ ⤶
- Medicare and the Marketplace, Master FAQ. Centers for Medicare and Medicaid Services. Accessed November 2023. ⤶
- Premium Tax Credit — The Basics. Internal Revenue Service. Accessed MONTH. ⤶
- Updates to frequently asked questions about the Premium Tax Credit. Internal Revenue Service. February 2024. ⤶
- Premium Tax Credit — The Basics. Internal Revenue Service. Accessed January 12, 2024. ⤶
- “Need Health Insurance” Kentucky.gov, 2023 ⤶
- ”Kentucky SB34, Kentucky HB10, Kentucky HB734, Kentucky HB380, and Kentucky HB700” BillTrack50. Accessed March 19, 2024. ⤶
- Kentucky House Bill 286; 2023 Session. BillTrack50. Accessed November 2023. ⤶
- Get Local Help. Kynect. Accessed November 2023. ⤶
- “2023 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2023 ⤶ ⤶ ⤶
- Cost-Sharing Quick Reference Guide. Kynect Health Coverage. Accessed November 2023. ⤶
- “2024 Health Insurance Companies” (Maps at bottom of page) Kentucky.gov, Accessed November 2023 ⤶ ⤶
- “Health Rate Filings” Kentucky Public Protection Cabinet, Kentucky.gov, Accessed August 2023 ⤶
- Analysis Finds No Nationwide Increase in Health Insurance Marketplace Premiums. The Commonwealth Fund. December 2014. ⤶
- Kentucky: APPROVED 2016 Weighted Avg. Rate Hikes: 13.8% Likely, 15.2% Maximum. ACA Signups. August 2015. ⤶
- Kentucky: *Approved* Avg. 2017 Rate Hikes: 24.5% (Vs. 23.6% Requested). ACA Signups. August 2016. ⤶
- 2018 Rate Hikes. ACA Signups. October 2017. ⤶
- Kentucky: APPROVED 2019 #ACA Rate Hikes: ~12.5%, But WOULD Likely Be FLAT W/Out #ACASabotage. ACA Signups. August 2018. ⤶
- Kentucky: *Approved* Avg. 2020 #ACA Premiums: 3.7% Increase (Down From 5.0%). ACA Signups. September 2019. ⤶
- Kentucky: Approved Avg. 2021 #ACA Premiums: +5.0% Indy Market, +8.8% Sm. Group Market. ACA Signups. October 2020. ⤶
- Kentucky: Approved Avg. 2022 #ACA Rate Changes: -3.8% Individual Market; +10.4% Sm. Group. ACA Signups. September 2021. ⤶
- “KY final average unsubsidized rates 2023” ACAsignups.net, Oct. 19, 2022 ⤶
- ”Marketplace 2024 Open Enrollment Period Report: Final National Snapshot” Centers for Medicare & Medicaid Services. January 24, 2024. ⤶
- “Health Insurance Marketplaces 2023 Open Enrollment Report” CMS.gov, Accessed August 2023 ⤶
- “ASPE Issue Brief (2014)” ASPE, 2015 ⤶
- “Health Insurance Marketplaces 2015 Open Enrollment Period: March Enrollment Report”, HHS.gov, 2015 ⤶
- “HEALTH INSURANCE MARKETPLACES 2016 OPEN ENROLLMENT PERIOD: FINAL ENROLLMENT REPORT” HHS.gov, 2016 ⤶
- “2017 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2017 ⤶
- “2018 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2018 ⤶
- “2019 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2019 ⤶
- “2020 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2020 ⤶
- “2021 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2021 ⤶
- “2022 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2022 ⤶







