Home > States > Health insurance in Minnesota
See your Minnesota health insurance coverage options.

Find individual and family plans, small-group, short-term or Medicare plans through licensed agency partners.

Minnesota Health Insurance Consumer Guide
We’ve compiled this guide to help you choose the right health insurance plan for you and your family. An ACA Marketplace/exchange plan – or Obamacare – is a good option for many people who don’t have access to Medicare, Medicaid, or employer-sponsored health insurance. We’re here to walk you through the choices available.
In Minnesota, you can sign up for ACA Marketplace coverage through MNsure, the state’s health insurance exchange, where five private insurers offer health insurance policies. If eligible, you may also get help to lower your monthly insurance cost (premium) and your out-of-pocket expenses through MNsure.
People in Minnesota can also sign up for MinnesotaCare – Minnesota’s Basic Health Program – or income-based Medical Assistance (Medicaid) through MNsure.1
Explore our other comprehensive guides to coverage in Minnesota
Dental coverage in Minnesota
Looking to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Minnesota.
Minnesota's Medicaid program

In 2013, Minnesota adopted the ACA’s Medicaid expansion. As of April 2023, Medicaid and CHIP plan enrollment grew 61% due to the expansion and the COVID-19 pandemic.2

Enrollment for Medicare in Minnesota

As of early 2023, more than 1.1 million Minnesotans were enrolled in Medicare coverage.3 Our guide explains everything you need to know about Medicare and Medigap plans in Minnesota.

Short-term coverage in Minnesota

No carrier currently markets short-term health insurance in the state of Minnesota.

Frequently asked questions about health insurance in Minnesota
Who can buy Marketplace health insurance?
To be eligible to enroll in private health coverage through the Marketplace in Minnesota (MNsure), you must:
- Be a Minnesota resident
- Be either a United States citizen or national, or be lawfully present
- Not be incarcerated
- Not have Medicare coverage
While most Minnesota residents are eligible to enroll in individual/family coverage through MNsure, eligibility for financial assistance (premium subsidies and cost-sharing reductions) is different. It depends on your income, and to qualify for financial assistance with your Marketplace plan you must:
- Not be eligible to enroll in an affordable employer-sponsored health insurance plan. If your employer (or your spouse’s employer) offers coverage but you feel it’s too expensive, you can use our Employer Health Plan Affordability Calculator to see if you might qualify for premium subsidies in the Marketplace.
- Not be eligible for Medical Assistance (Minnesota Medicaid) or MinnesotaCare.
- Not be eligible for premium-free Medicare Part A.4
When can I enroll in an ACA-compliant plan in Minnesota?
In Minnesota, you can sign up for an ACA-compliant individual or family health plan from November 1 to January 15 during open enrollment.5
If you need your coverage to start on January 1, you must apply by December 15. If you apply between December 16 and January 15, your coverage will begin on February 1.
Outside of open enrollment time, you may be eligible to enroll if you experience a qualifying life event, such as giving birth or losing employer-sponsored insurance.
How do I enroll in a Marketplace plan in Minnesota?
To enroll in an ACA Marketplace plan in Minnesota, you can:
- Visit MNsure – Minnesota’s health insurance marketplace. MNsure provides an online platform to shop, compare, and choose the best health plans.
- Purchase individual and family health coverage through insurance agents or brokers, or with help from an MNsure Navigator.6
You can also call MNsure’s contact center by dialing 651-539-2099 (or 855-366-7873 if you’re outside the Twin Cities). The contact center operates from 8 a.m. to 4 p.m. from Monday to Friday.
How can I find affordable health insurance in Minnesota?
You may find affordable health insurance options in Minnesota by signing up through MNsure.
Under the Affordable Care Act, there are income-based subsidies – a type of financial assistance – called Advance Premium Tax Credits (APTC). APTCs can help lower your premium payments and reduce your overall expenses.
Families eligible for APTC in Minnesota will see an average total premium savings of $6,750 on 2024 coverage due to tax credits.7
More than half of MNsure’s private plan enrollees in the state saved around $346 per month on their 2023 premium expenses – those who qualified for subsidies pay an average monthly net premium of $203.8
If your household income is no more than 250% of the federal poverty level, you may also qualify for cost-sharing reductions (CSR). These reductions can lower your deductibles and out-of-pocket expenses. Combining APTCs and CSRs might make an ACA plan the most budget-friendly health insurance choice for you.
You can also find inexpensive health insurance through Medicaid (called Medical Assistance in Minnesota). Check to see if you meet the criteria for Medicaid in Minnesota.
If your income is too high for Medical Assistance but not more than 200% of the poverty level, you may find that you’re eligible for MinnesotaCare, which is the state’s Basic Health Program.
Minnesota also has a reinsurance program, which helps to keep premiums lower than they would otherwise be for people whose income is too high to qualify for premium subsidies.9
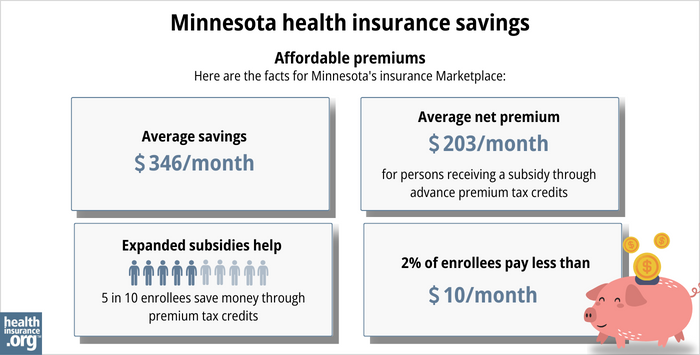
Source: CMS.gov8
How many insurers offer Marketplace coverage in Minnesota?
There are five insurers that offer exchange plans in Minnesota:10
PreferredOne, which has only offered coverage outside the exchange for the last several years, is exiting Minnesota’s individual/family market altogether at the end of 2023. People enrolled in PreferredOne’s individual plans in 2023 need to select a new plan from a different insurer in order to have coverage in 2024.11
The availability of plans varies by location. For 2024, most counties in Minnesota offer exchange plans from at least three different insurers, and every county has at least two insurers offering plans through MNsure.12
Are Marketplace health insurance premiums increasing in Minnesota?
For 2024, the following average rate changes have been approved for MNsure’s individual/family insurers,13 amounting to an overall average increase of about 4.5%:14
Minnesota’s ACA Marketplace Plan 2024 Approved Rate Increases by Insurance Company |
|
|---|---|
| Issuer | Percent Increase |
| Blue Plus | 3.0% |
| Health Partners, Inc. | 5.5% |
| Medica | 1.9% |
| UCare | 5.5% |
| Quartz | 3.2% |
Source: Minnesota Commerce Department10
Keep in mind that these average rate increases are for full-price plans. However, more than half of the people who enroll through MNsure get premium tax credits that help reduce costs.15
These subsidies are adjusted each year to match changes in the benchmark plan (the second-lowest-cost Silver plan) in each area. As a result of the American Rescue Plan and the Inflation Reduction Act, the subsidies are larger and more widely available than they were in the past.
If the cost of your current plan increases, you may find that a different MNsure plan might be a better fit for your needs and budget.
How many people are insured through Minnesota’s Marketplace?
During the open enrollment period for 2023 coverage, 118,431 people enrolled in private health coverage through the Minnesota exchange.16 This doesn’t include people enrolled in MinnesotaCare and Medical Assistance.
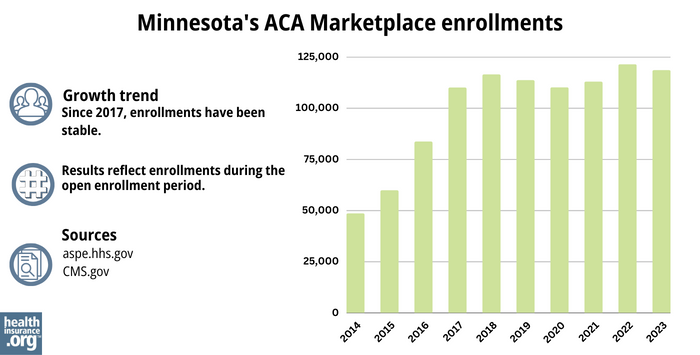
Source: 2014,17 2015,18 2016,19 2017,20 2018,21 2019,22 2020,23 2021,24 2022,25 202326
What health insurance resources are available to Minnesota residents?
MNsure: Minnesota’s health insurance marketplace provides financial help for individual plan premiums exclusively to state residents. To reach MNsure for more information, dial (651) 539-2099 or (855) 366-7873 if outside the Twin Cities.
Minnesota Department of Human Services: The Minnesota Department of Human Services offers health care coverage programs and resources. You can call their customer service at 651-297-3862 or 800-657-3672 for assistance.
Local tribal or county health care office: To receive assistance with health care programs, you can contact your local tribal or county health care office.
Minnesota State Health Insurance Assistance Program: You can find information and resources for Minnesota’s Medicare beneficiaries.
Medical Assistance: Minnesota’s Medical Assistance (Medicaid) program helps low-income individuals and families with medical coverage. This program has eligibility requirements, and more information is available on the Minnesota Department of Health website.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- Applying for Medical Assistance (MA) and MinnesotaCare. Minnesota Department of Human Services. Accessed November 2023. ⤶
- "Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment" KFF.org, April 2023 ⤶
- “Medicare Monthly Enrollment” CMS.gov, April 2023 ⤶
- Medicare and the Marketplace, Master FAQ. Centers for Medicare and Medicaid Services. Accessed November 2023. ⤶
- “Open Enrollment Period” MNsure.org, 2023 ⤶
- Navigators. MNsure. Accessed November 2023. ⤶
- MNsure’s Annual Health Insurance Open Enrollment Window Starts Today. MNsure. November 2023. ⤶
- “2023 OEP State-Level Public Use File (ZIP)” CMS.gov, March 23, 2023 ⤶ ⤶
- 2023 Health Insurance Rates. Minnesota Commerce Department. Accessed November 2023. ⤶
- 2024 Health Insurance Rates. Minnesota Commerce Department. Accessed November 2023. ⤶ ⤶
- Individual Plans. PreferredOne. Accessed November 2023. ⤶
- MN Dept of Commerce approves 2024 rates for individual and small group health insurance in Minnesota. Minnesota Commerce Department, September 2023. ⤶
- MN Dept of Commerce approves 2024 rates for individual and small group health insurance in Minnesota. Minnesota Commerce Department, September 2023. ⤶
- Minnesota: *Final* Avg. Unsubsidized 2024 #ACA Rate Change: +4.5%. ACA Signups. October 2023. ⤶
- “Effectuated Enrollment: Early 2023 Snapshot and Full-Year 2022 Average” Centers for Medicare and Medicaid Services. ⤶
- “Health Insurance Marketplaces 2023 Open Enrollment Report” CMS.gov ⤶
- “ASPE Issue Brief (2014)” ASPE, 2015 ⤶
- “Health Insurance Marketplaces 2015 Open Enrollment Period: March Enrollment Report”, HHS.gov, 2015 ⤶
- “HEALTH INSURANCE MARKETPLACES 2016 OPEN ENROLLMENT PERIOD: FINAL ENROLLMENT REPORT” HHS.gov, 2016 ⤶
- “2017 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2017 ⤶
- “2018 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2018 ⤶
- “2019 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2019 ⤶
- “2020 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2020 ⤶
- “2021 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2021 ⤶
- “2022 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2022 ⤶
- “Health Insurance Marketplaces 2023 Open Enrollment Report” CMS.gov, 2023 ⤶







