Home > States > Health insurance in Indiana
See your Indiana health insurance coverage options now.

Find affordable individual and family plans, small-group, short-term, or dental plans through licensed agency partners.

Indiana Health Insurance Consumer Guide
Indiana uses the federally run health insurance exchange/Marketplace, HealthCare.gov, where six private insurance companies offer individual/family coverage for 2024.1 Marketplace plans are designed to serve those without access to employer-sponsored coverage or government-run coverage like Medicare or Medicaid. This includes self-employed individuals, people who work for small businesses that don’t offer health benefits, and early retirees who aren’t yet eligible for Medicare.
Many people find Affordable Care Act (ACA) Marketplace plans to be budget-friendly, and nearly 296,000 people enrolled in private health plans through the Indiana Health Insurance Marketplace during the open enrollment period for 2024 coverage.2
If you buy a plan through the Indiana Health Insurance Marketplace, you may qualify for financial assistance through an advance premium tax credit (premium subsidy) and also possibly a subsidy that reduces your out-of-pocket costs when you get medical care.3
As of 2024, small businesses (fewer than 50 employees) in Indiana can qualify for a state tax credit if they offer an ICHRA benefit to their employees, as long as certain parameters are met.4
View our other comprehensive guides to coverage in Indiana
Dental coverage in Indiana
Get protection from expensive dental costs. Compare different plan options to find premiums and deductibles that match your budget.
Indiana’s Medicaid program

Indiana made Medicaid available to more people by adopting ACA’s expansion in 2015.5 As of August 2023, over 825,000 Indianans were covered by Healthy Indiana Plan, also known as the expanded Medicaid program in the state.6

Medicare coverage options and enrollment in Indiana

In 2023, more than 1.3 million people in Indiana were enrolled in Medicare.7 If you’re curious about signing up for Medicare in Indiana or want to know about the state’s Medigap rules, our guide has you covered.

Short-term coverage in Indiana

As of 2023, there were at least seven insurance companies offering short-term healthcare policies in Indiana.8

Frequently asked questions about health insurance in Indiana
Who can buy Marketplace health insurance?
You can buy individual/family health insurance from Indiana’s Marketplace if:9
- You live in Indiana.
- You are lawfully present in the U.S.
- You don’t have Medicare.
- You are not incarcerated.
Marketplace financial assistance, such as premium subsidies and cost-sharing reductions, depends on your household income. In addition, to qualify for financial assistance, you must:
- Not have access to affordable coverage via an employer. Our Employer Health Plan Affordability Calculator can help you check if you might qualify for premium subsidies in the Marketplace.
- Not be eligible for Medicaid or CHIP/Hoosier Healthwise.
- Not be eligible for premium-free Medicare Part A. 10
- File a joint tax return with your spouse, if you’re married.11 (with very limited exceptions)12
- Not be able to be claimed by someone else as a tax dependent.11
When can I enroll in an ACA-compliant plan in Indiana?
In Indiana, you can sign up for ACA-compliant individual and family health plans during the annual open enrollment period, which runs from November 1 through January 15.13
If you sign up by December 15, your coverage starts on January 1. If you enroll between December 16 and January 15, your coverage begins on February 1.
If the open enrollment deadline passes, you may still be able to sign up for or make changes to an ACA Marketplace health plan through a special enrollment period (SEP). To qualify for a SEP, you’ll generally need a qualifying life event.
However, you can apply in some situations even if you don’t have a qualifying life event. These include:
- If you’re eligible for premium tax credits and your income is no more than 150% of the poverty level, you can enroll at any time until at least the end of 2025.14 (The federal government has proposed making this a permanent SEP opportunity.)15
- If you’re a Native American, you can enroll anytime.16
- If you lose Medicaid or CHIP between March 31, 2023 and July 31, 2024, you can use the extended SEP to enroll at any time during that window.17
How do I enroll in a Marketplace plan in Indiana?
There are a few ways to enroll in an exchange health plan in Indiana:
- You can sign up on HealthCare.gov – the ACA exchange website.
- Alternatively, you can call them at (800) 318-2596 (TTY: 1-855-889-4325). The call center is available 24 hours a day, seven days a week, but it’s closed on holidays.
- You can get help — in person, online, or over the phone, from agents, navigators, or certified application counselors.
- You can enroll via an approved enhanced direct enrollment entity.18
How can I find affordable health insurance in Indiana?
In Indiana, you can find affordable health plans through the ACA Marketplace’s website: HeathCare.gov.
Thanks to the ACA, you may be eligible for income-based premium subsidies called Advance Premium Tax Credits (APTC), which help reduce your monthly premiums.
Nearly nine out of 10 Indiana exchange enrollees were eligible for premium subsidies on 2023 plans, with an average monthly savings of about $455. People who received these subsidies pay an average monthly premium of $125.19
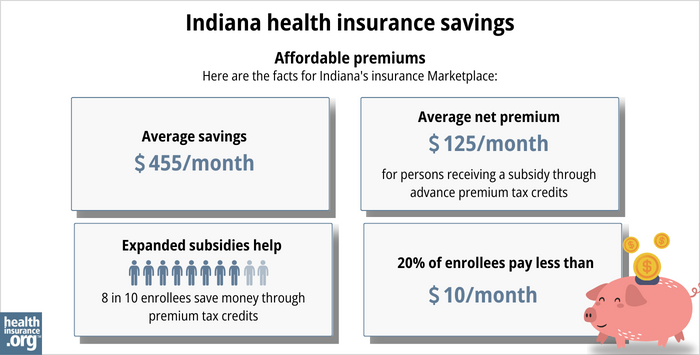
Cost-sharing reductions (CSR) also reduce costs by helping lower your deductibles and out-of-pocket costs. CSR benefits are automatically built into all of the available Silver-level plans as long as your income isn’t more than 250% of the federal poverty level.3
The federal government used to reimburse insurers for the cost of providing CSR benefits, but that ended in 2017. Since then, insurers have been adding the cost of CSR to the premiums they charge. In most states, this cost is only added to Silver-plan rates, since CSR benefits are only available on Silver plans. But Indiana is one of only two states where insurers are required to spread the cost of CSR across premiums for plans at all metal levels (broad loading, as opposed to the silver loading approach taken in most states).
Medicaid is another affordable health coverage for those who meet the criteria. Check out our guide on Medicaid in Indiana for more information.
Short-term plans are also available as a cost-effective option if you don’t qualify for employer plans, Medicaid, Medicare, or subsidies from the exchange. Learn more about short-term health insurance in Indiana.
How many insurers offer Marketplace coverage in Indiana?
Are Marketplace health insurance premiums increasing in Indiana?
Indiana’s individual market insurers implemented the following average rate increases for 2024,22 which amount to an overall weighted average rate increase of 2.1%.23
Indiana’s ACA Marketplace Plan 2024 Approved Rate Increases by Insurance Company |
|
|---|---|
| Issuer | Percent Increase |
| Anthem (Anthem BCBS) | -0.95% |
| Caresource | 0.73% |
| Celtic/MHC/Ambetter | 0.64% |
| Cigna | 11.62% |
| US Health and Life Insurance Company | 12.87% |
| Aetna Health | new for 2024 |
Source: HealthCare.gov22
These changes apply to the full-price premiums. But most Indiana residents who use the exchange receive financial assistance in the form of premium tax credits (premium subsidies), and thus do not pay full price.19
If you qualify for subsidies, the actual change in what you pay depends on how much your plan’s cost changes and how much financial assistance you receive from the government.
For perspective, here’s an overview of how full-price premiums have changed over the years in Indiana’s individual/family health insurance market:
- 2015: Average increase of 5%.24
- 2016: Average increase of 0.7%.25
- 2017: Average increase of 18.9%.26
- 2018: Average increase of 24%.27
- 2019: Average increase of 2.6%.28
- 2020: Average increase of 13.5%.29
- 2021: Average increase of 10.5%.30
- 2022: Average decrease of 1.7%.31
- 2023: Average increase of 5.7%.32
How many people are insured through Indiana’s Marketplace?
During the open enrollment period for 2024 coverage, 295,772 people enrolled in private individual market health plans through the Indiana Marketplace.33
The 2024 enrollment number was a record high (see chart below for historical enrollment numbers).
Enrollment has been growing since 2021, partly due to the subsidy enhancements created by the American Rescue Plan and Inflation Reduction Act.
The enrollment growth in 2024 was also due to the “unwinding” of the pandemic-era Medicaid continuous coverage. As of December 2023, more than 671,000 Indiana residents had been disenrolled from Medicaid.34 And CMS reported that by October, more than 43,000 of those people had transitioned to a Marketplace plan.35
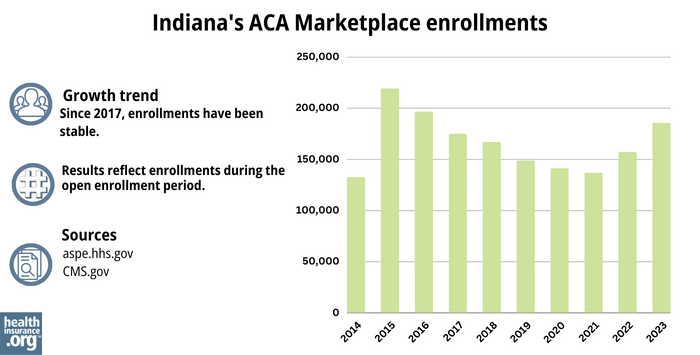
Source: 2014,36 2015,37 2016,38 2017,39 2018,40 2019,41 2020,42 2021,43 2022,44 202345
What health insurance resources are available to Indiana residents?
HealthCare.gov
800-318-2596
Indiana Department of Insurance
Oversees and licenses health insurance companies, brokers, and agents who sell insurance plans. It can be a valuable source for Indiana residents with questions or complaints about their health coverage.
Affiliated Service Providers of Indiana, Inc. (ASPIN)
A Navigator organization funded by the federal government, serving Indiana. They can assist with questions and help people enroll in Medicaid or a private insurance plan through the exchange.
Indiana State Health Insurance Assistance Information Program (SHIP)
This local service offers guidance and information to Medicare beneficiaries and their caregivers.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- Indiana 2024 ACA Filings. Indiana Department of Insurance. Accessed December 7, 2023. ⤶
- ”Marketplace 2024 Open Enrollment Period Report: Final National Snapshot” Centers for Medicare & Medicaid Services. January 2024. ⤶
- APTC and CSR Basics. Centers for Medicare and Medicaid Services. June 2023. ⤶ ⤶
- New tax credit a boon for Indiana Small Business Health Insurance. Take Command Health. September 2023. ⤶
- “Federal Officials Approve Indiana Medicaid Expansion Plan” The Commonwealth Fund, Jan. 27, 2015 ⤶
- “Medicaid Monthly Enrollment Reports” Family and Social Services Administration, In.gov ⤶
- “Medicare Monthly Enrollment” CMS.gov, April 2023 ⤶
- “Availability of short-term health insurance in Indiana” healthinsurance.org, Feb. 23, 2023 ⤶
- “Are you eligible to use the Marketplace?” HealthCare.gov, 2023 ⤶
- Medicare and the Marketplace, Master FAQ. Centers for Medicare and Medicaid Services. Accessed November 2023. ⤶
- Premium Tax Credit — The Basics. Internal Revenue Service. Accessed MONTH. ⤶ ⤶
- Updates to frequently asked questions about the Premium Tax Credit. Internal Revenue Service. February 2024. ⤶
- “Where can you get health insurance?” HealthCare.gov, 2023 ⤶
- “An SEP if your income doesn’t exceed 150% of the federal poverty level” healthinsurance.org, Feb. 1, 2023 ⤶
- HHS Notice of Benefit and Payment Parameters for 2025 Proposed Rule. Centers for Medicare and Medicaid Services. November 2023. ⤶
- “Who doesn’t need a special enrollment period?“ healthinsurance.org, Accessed August 2023 ⤶
- “Temporary Special Enrollment Period (SEP) for Consumers Losing Medicaid or the Children’s Health Insurance Program (CHIP) Coverage Due to Unwinding of the Medicaid Continuous Enrollment Condition– Frequently Asked Questions (FAQ)” CMS.gov, Jan. 27, 2023 ⤶
- “Entities Approved to Use Enhanced Direct Enrollment” CMS.gov, April 28, 2023 ⤶
- “2023 Marketplace Open Enrollment Period Public Use Files” CMS.gov, March 2023 ⤶ ⤶
- Indiana 2024 ACA Filings. Indiana Department of Insurance. Accessed December 2023. ⤶
- Aetna CVS Health to enter the Affordable Care Act (ACA) individual insurance exchange marketplace in Indiana for January 1, 2024. PR Newswire. October 2023. ⤶
- ”Indiana Rate Review Submissions” HealthCare.gov, 2023 ⤶ ⤶
- Indiana: *Final* Avg. Unsubsidized 2024 #ACA Rate Changes: +2.1%. ACA Signups. August 2023. ⤶
- Analysis Finds No Nationwide Increase in Health Insurance Marketplace Premiums. The Commonwealth Fund. December 2014. ⤶
- Indiana: Approved 2016 Weighted Avg. Rates Confirmed As Only 0.7%. ACA Signups. September 2015. ⤶
- Avg. UNSUBSIDIZED Indy Mkt Rate Hikes: 25% (49 States + DC). ACA Signups. October 2016. ⤶
- UPDATE: Indiana Chooses The Worst Possible Way Of Spreading Their CSR Load. ACA Signups. October 2017. ⤶
- 2019 Rate Hikes. ACA Signups. October 2018. ⤶
- Indiana: *Final* Avg. 2020 #ACA Premium Rate Hikes: IN DOI Says 9.7%. The Math Says 13.5%. ACA Signups. October 2019. ⤶
- 2021 Rate Changes. ACA Signups. October 2020. ⤶
- Indiana 2022 ACA Filings. Indiana Department of Insurance. Accessed December 2023. ⤶
- Indiana: Final Avg. Unsubsidized 2023 #ACA Rate Changes: +5.7%. ACA Signups. October 2022. ⤶
- ”Marketplace 2024 Open Enrollment Period Report: Final National Snapshot” Centers for Medicare & Medicaid Services. January 24, 2024. ⤶
- ”Medicaid Enrollment and Unwinding Tracker” KFF. February 13, 2024. ⤶
- ”HealthCare.gov Marketplace Medicaid Unwinding Report” Centers for Medicare & Medicaid Services. Data through October 2023. ⤶
- “ASPE Issue Brief (2014)” ASPE, 2015 ⤶
- “Health Insurance Marketplaces 2015 Open Enrollment Period: March Enrollment Report”, HHS.gov, 2015 ⤶
- “HEALTH INSURANCE MARKETPLACES 2016 OPEN ENROLLMENT PERIOD: FINAL ENROLLMENT REPORT” HHS.gov, 2016 ⤶
- “2017 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2017 ⤶
- “2018 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2018 ⤶
- “2019 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2019 ⤶
- “2020 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2020 ⤶
- “2021 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2021 ⤶
- “2022 Marketplace Open Enrollment Period Public Use Files” CMS.gov, 2022 ⤶
- “Health Insurance Marketplaces 2023 Open Enrollment Report” CMS.gov, 2023 ⤶







