Medicaid eligibility and enrollment in Kansas

2025 Medicaid expansion legislation includes a work requirement in an effort to win over GOP lawmakers

Who is eligible for Medicaid in Kansas?
Kansas Medicaid, which is called KanCare, is available to individuals who meet the following income limits (plus an extra 5% in most cases, as an income disregard):1
- Children up to age 1 are covered with family income up to 166% of the federal poverty level (FPL)
- Children ages 1 to 5 are covered with family income up to 149% of FPL
- Children ages 6 to 18 are covered with family income up to 133% of FPL
- Pregnant women with family income up to 166% of FPL (coverage for the mother continues for 12 months after the baby is born)2
- Parents with dependent children are eligible with household income up to 33% of FPL
- Children with family income too high to qualify for Medicaid but not more than 227% of FPL are eligible for the Children’s Health Insurance Program (CHIP)
- Individuals who are elderly or disabled may also qualify for Kansas Medicaid; Learn more here about how Kansas Medicaid helps low-income residents who are also enrolled in Medicare
Kansas has not implemented ACA Medicaid expansion for adults with income up to 138% of the federal poverty level. As a result, childless, non-disabled, non-elderly adults are not eligible for coverage regardless of how low their income is, and parents with dependent children can only qualify if they live in extreme poverty. This creates a coverage gap in Kansas for most adults with income below the poverty level.
Legislation to expand Medicaid in Kansas has been considered several times in recent years. New Medicaid expansion legislation, including a work requirement, was introduced in the Kansas Senate and House in February 2025.3
Medicaid expansion legislation has been unsuccessful in previous years (although some bills have come close, as explained below). The 2024 bills also included work requirements, offered as a compromise solution.4 But those bills were unsuccessful and did not advance to a vote.5
Apply for Medicaid in Kansas
Children and families can apply online. Anyone needing assistance with the application process can call 1-888-369-4777 for help.
Eligibility: Children up to age 1 with family income up to 166% of FPL. Children ages 1-5 with family income up to 149% of FPL. Children ages 6-18 with family income up to 133% of FPL; children with family income up to 242% of FPL are eligible for CHIP.



Has Kansas expanded Medicaid?
No, Kansas has not expanded Medicaid. Kansas is one of only ten states where the ACA’s expansion of Medicaid still has not been implemented as of 2025. As a result, the state has an estimated 39,000 low-income residents who are stuck in the “coverage gap,” meaning that they earn too little to qualify for subsidized private health coverage, but are also ineligible for Medicaid because the state has refused to accept federal funding to expand Medicaid.6
Legislative attempts to expand Medicaid have repeatedly failed in Kansas. The most recent Medicaid expansion legislation was introduced in the Kansas Senate in February 2025.7 The two similar bills introduced in 2024 were unsuccessful.5
The expansion legislation introduced in 2024 and 2025 has included work requirements, in a compromise solution offered by Governor Laura Kelly.4 They do differ from work requirement bills that many other states have considered, in that they call for proof of employment to enroll in Medicaid (unless exempt), but not a specific number of hours that the person must work. Proof of employment can include a W-2, 1099, pay stub, etc. (one of the exemptions is proof of volunteering at least 20 hours per week).
Legislation to expand Medicaid passed in 2017, but then-Gov. Sam Brownback vetoed it. Medicaid expansion legislation passed again in the Kansas House in 2019, but died in the Senate. In 2020, Medicaid expansion legislation was announced as a bipartisan compromise by Democratic Gov. Laura Kelly and Republican Senate Majority Leader Jim Denning, but ultimately failed to pass.
The legislation that was introduced in the Kansas House in 2022 did not advance out of committee.8 And neither did the bills that were introduced in 20239
Learn how states that expanded Medicaid might reduce spending on Medicaid.
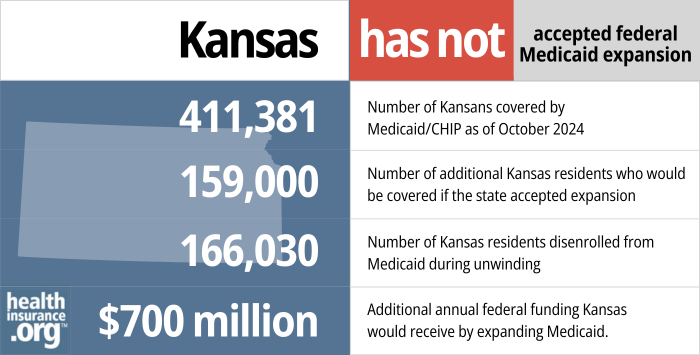
- 411,381 – Number of Kansans covered by Medicaid/CHIP as of October 202410
- 159,000 – Number of additional Kansas residents who would be covered if the state accepted expansion11
- 166,030 – Number of Georgia residents disenrolled from Medicaid during unwinding12
- $700 million – Additional annual federal funding Kansas would receive if the state expanded Medicaid13
Explore our other comprehensive guides to coverage in Kansas

Use this guide to help you find the right health plan in Kansas. Many people find an ACA Marketplace plan, also known as Obamacare or exchange, to be a cost-effective choice.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Kansas.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Kansas as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.

Frequently asked questions about Kansas Medicaid eligibility and enrollment
How do I enroll in Medicaid in Kansas?
For children and families:
- Apply on the KanCare Medical Self-Service portal (you will need to login or create an account) or on the Healthcare.gov website (if you are under 65 years old; if it appears you’re eligible, your information will be transferred to KanCare).
- Complete an application. Call 1-800-792-4884 for help determining which application to use or to have an application mailed to you. The form describes options for returning the form.
- If you need help with the application process, contact DCF toll free at 1-888-369-4777.
For elderly or disabled individuals:
- Apply on the KanCare Medical Self-Service portal (you will need to login or create an account).
- Complete an application. Call 1-800-792-4884 for help determining which application to use or to have an application mailed to you. The form describes options for returning the form.
How many Kansas residents were disenrolled from Medicaid after the pandemic?
Under federal rules, states were not allowed to disenroll anyone from Medicaid between March 2020 and March 2023. But that rule ended March 31, 2023, allowing disenrollments to resume. Eligibility for all Medicaid enrollees had to be checked during a year-long “unwinding” period that began in the spring of 2023.
KFF reported that about 166,000 people were disenrolled from KanCare during the unwinding process, while coverage was renewed for almost 319,000 enrollees.14
Many people who were disenroled from Medicaid were able to transition to an employer’s plan, although some likely became uninsured. And more than 31,000 transitioned to private coverage purchased through the health insurance Marketplace in Kansas.15
How many people are enrolled in Medicaid in Kansas?
As of July 2013, enrollment in Kansas Medicaid/CHIP was 378,160. By October 2024, it stood at 411,381.16
Enrollment had been significantly higher during the pandemic, peaking in early 2023. But as was the case nationwide, enrollment declined during the year-long “unwinding” process, described above.
Kansas Medicaid history and details
Bipartisan Medicaid expansion legislation was considered in 2020 but did not pass
Although Kansas was considered a state to watch for Medicaid expansion legislation in 2020, the bill was ultimately unsuccessful.
Two bills were pre-filed for consideration during the 2020 session. S.B.246 was pre-filed in early December 2019. It included monthly fees that could be as high as $25 per enrollee, and would refer unemployed Medicaid expansion recipients to a job training program. And S.B.252, which was pre-filed in January, just before the start of the legislative session, was announced as a bipartisan compromise by Democratic Gov. Laura Kelly and Republican Senate Majority Leader Jim Denning, arousing hopes that Kansas will be the next state to expand Medicaid.
But then-Senate President, Susan Wagle (R, Wichita) was opposed to Medicaid expansion, and refused to allow it to come up for a vote in the Senate unless both chambers of the legislature passed a constitutional amendment that would have overturned the Kansas Supreme Court ruling that protects a woman’s access to abortion in Kansas.
At that point, abortion access was still legally protected nationwide under Row v. Wade, but abortion opponents were hoping that could be overturned at the federal level by the Supreme Court (which did happen in 2022). The Kansas court ruling upholds a woman’s right to choose in Kansas, regardless of federal rules. But Wagle and other anti-choice Republicans in Kansas would like to see that changed, and blocked the 2020 Medicaid expansion legislation in an effort to try to pass the abortion amendment.
Senate Democrats made a last-ditch attempt to bring the Medicaid expansion measure up for a vote in May, but were unsuccessful as a result of procedural rules. Denning expressed that he was “profoundly disappointed” that the bill never received a floor debate during the 2020 session.
Senator Barbara Bollier, M.D. who was among the sponsors for both Medicaid expansion bills, wrote an article on our site in 2017 about the importance of Medicaid expansion and her tireless efforts to convince other Kansas lawmakers to expand coverage. Bollier was a Republican at that point, but became a Democrat in 2018 and unsuccessfully ran for election to the US Senate in the 2020 election. Wagle was vying for the Republican nomination to run against Bollier, but dropped out in May 2020.
Details of the bipartisan Medicaid expansion proposal that was introduced in 2020
A summary of the bipartisan Medicaid expansion legislation (S.B.252) is available here. In a nutshell, here is what was being proposed, although the legislation was ultimately unsuccessful:
- Full Medicaid expansion, as outlined in the ACA, would have taken effect as of January 2021.
- Kansas would have conducted an actuarial study related to reinsurance and the possibility of switching people with income between 100 and 138% of the poverty level back to the exchange (this group is already eligible for coverage in the exchange — it’s only people under the poverty level who are in the Medicaid coverage gap — but they would have transitioned to Medicaid as of 2021 under the terms of S.B.252).
- By 2021, Kansas would have submitted a 1332 waiver to CMS, seeking to implement a reinsurance program. Reinsurance programs lower premiums across the board in the individual market, although the lower premiums are really only felt by people who pay full price for their coverage. For those who get subsidies (which includes the large majority of enrollees), the subsidy amounts decline along with premiums — in some cases, people who get subsidies end up paying more with a reinsurance program in place.
- At the same time, Kansas would submit an 1115 waiver to CMS, seeking approval to switch people earning 100-138% of the poverty level back to the exchange. If approved, this waiver would essentially mean that this population would have gone from private, subsidized plans in the exchange in 2020, to Medicaid in 2021, and back to private subsidized plans in the exchange in 2022.
- The plan to seek approval to transition people above the poverty level back to private insurance was a nod to conservative Medicaid expansion proposals, and was part of the bipartisan appeal of S.B.252. But this proposal was much less likely to be approved, as CMS has not yet approved it anywhere, despite some states efforts. (Most recently, Utah tried to receive Medicaid expansion funding while only expanding coverage to 100% of the poverty level, and CMS said no. Utah ultimately agreed to fully expand coverage, to 138% of the poverty level, in order to get full Medicaid expansion funding from the federal government.)
- And the legislation clarified that if CMS doesn’t approve the 1115 waiver (or the 1332 waiver, although that’s much less likely to be an issue), full Medicaid expansion would continue in Kansas.
- Unemployed Medicaid expansion enrollees would be referred to the Kansas Works Program (this is a work referral program, as opposed to a work requirement; people would receive assistance with job training and securing work, but would not lose their health insurance as a result of not having a job).
- Premiums of up to $25/month could be charged for people with income above the poverty level. But people would not have beenlocked out of Medicaid expansion for failure to pay the premiums (instead, they’d have been subject to collection under the rules for debts owed to the state of Kansas). The $25/person fee would be allowed to amount to as much as $100 per month per family, but children under the age of 19 are eligible for Medicaid or CHIP in Kansas with family incomes as high as 230% of the poverty level, so they would not be subject to the fee, as they would not be newly-eligible for Medicaid under the expansion rules.
- As explained here by Charles Gaba and Dave Anderson (when Kansas considered similar legislation in 2019), a fee of $25/month would put some low-income Kansans in a worse financial spot than they currently have with subsidized coverage in the exchange. But non-disabled, non-pregnant adults without minor children are not currently eligible for Medicaid at all in Kansas if their income is below the poverty level. So even with a fee, Medicaid expansion would be better for them than the status quo. It’s also worth noting that the legislation includes a stipulation that monthly premiums for Medicaid expansion enrollees could not exceed 2% of income (it’s not clear, however, if the $25/month “fee” would is considered a premium). For a single person, that would amount to a premium cap of less than $25/month as long as their income didn’t exceed $15,000/year.
Medicaid expansion passed the House in 2019 but died in the Senate
H.B.2066, which called for Medicaid expansion, passed in the Kansas House in March 2019 by a vote of 69-54 (note that the bill was revised; it initially dealt with nursing regulations, but that text was replaced with the Medicaid expansion text in the final version). But it never reached a floor vote in the Senate, as explained here by Kansas Representative Brett Parker. H.B.2066 included a job training referral program and a monthly fee of up to $25 for Medicaid expansion enrollees.
2017: House and Senate passed expansion but Governor Brownback vetoed it
In September 2016, Sandy Praeger, a Republican and former Kansas Insurance Commissioner, called on Governor Brownback and Kansas lawmakers to expand Medicaid, saying that there was “no logical explanation” for the state’s continued rejection of federal funding for Medicaid expansion, and noting that the decision has been based on politics rather than cost analysis.
And the state’s primary election in August 2016 resulted in several moderate Republicans getting onto the ballot for November, energizing Medicaid expansion advocates. Supporters became more confident than ever that they could get a bill passed in 2017 to expand coverage, particularly given that several of the primary winners had been outspoken about their support for Medicaid expansion.
On February 23, 2017, H.B.2044 passed the Kansas House of Representatives, 81-44. A month later, the bill passed the Senate, 25-14. But then-Governor Sam Brownback remained steadfast in his opposition to Medicaid expansion, and vetoed the bill. Although the Medicaid expansion legislation passed by a wide margin in both chambers, it was a few votes shy of a veto-proof majority.
On April 3, the House voted to uphold Brownback’s veto. The final margin was 81-44, three votes shy of the 84 votes that would have been necessary to override the Governor’s veto. Two representatives who had voted for expansion ended up voting to uphold the veto, while two others who had opposed the expansion vote shifted sides and voted to override the veto. In the end, the numbers ended up the same as they had been the prior week, and the governor’s veto remained in effect.
Brownback listed several reasons for vetoing H.B.2044:
- He wanted Medicaid reform to eliminate the existing waiting lists for disabled Kansans (a population that was already eligible for Medicaid pre-ACA)
- He wanted Medicaid reform to be budget neutral for the state (expanded Medicaid is funded almost entirely by the federal government, but states began paying 5% of the cost in 2017, and that has grown to 10% in 2020 and future years).
- He wanted a work requirement for able-bodied adults (as opposed to the work referral program in H.B.2044)
- He wanted Medicaid reform to cut funding for Planned Parenthood, and H.B.2044 did not do that.
- He believed it would be “unwise” to expand Medicaid given the uncertainty of the ACA on the federal level (ultimately, the ACA has remained in place; efforts to repeal it legislatively have failed, and the Supreme Court has upheld the law three times)
In 2014, Brownback signed legislation (H.B.2552) that required legislative approval to expand Medicaid (as opposed to allowing it via executive action, which is the path that governors in some states have used to expand Medicaid without having to obtain approval from lawmakers). H.B.2552 was popular with Brownback and 2014’s more-conservative legislature, particularly given the strong-than-anticipated gubernatorial campaign of then-House Minority Leader, Paul Davis — a Democrat who supported Medicaid expansion.
The American Cancer Society, which supports Medicaid expansion, reported that 82% of Kansas survey respondents wanted the state to accept federal funding to expand Medicaid. Hospital leaders in Kansas also pushed hard for Medicaid expansion, noting that without expansion, some rural hospitals would be forced to close. Although the measure passed by a wide margin in both chambers, it simply wasn’t enough to overcome the governor’s veto.
Lawmakers again considered Medicaid expansion during the 2018 legislative session, although the bill did not pass. Jeff Colyer, who assumed the Governor’s office in January 2018 when Brownback left the join the Trump Administration, was also opposed to Medicaid expansion in the state, and would have been likely to veto an expansion bill, just as Brownback did.
The Senate Public Health and Welfare Committee passed the 2018 Medicaid expansion bill (S.B.38) in February, but it did not advance after that. House Democrats also tried amending other 2018 bills, including a budget bill, to include Medicaid expansion, but were unsuccessful.
KanCare 2.0 waiver proposal initially called for a work requirement and 36-month cap on Medicaid benefits. CMS rejected the 36-month cap and Kansas withdrew the work requirement
The KanCare Medicaid program operates with a waiver from CMS that must be periodically extended. The state was given a temporary extension, through the end of 2018,17 but needed a longer-term renewal by the end of 2018. The state’s initially proposed KanCare renewal, dubbed KanCare 2.0, called for a work requirement for able-bodied, non-exempt adults, and would also have imposed a 36-month limit on Medicaid eligibility for adults who were subject to, and in compliance with, the work requirement (those who do not comply with the work requirement would lose access to Kansas Medicaid after just three months).
In May 2018, CMS notified Kansas that the 36-month cap on Medicaid eligibility would not be allowed. The federal government was still considering the rest of the state’s proposal at that point, but the letter indicated that CMS was likely to approve the state’s proposed work requirements, and reiterated the fact that CMS has been willing to approve lock-out periods for people who don’t comply with work requirements, which was part of Kansas’ proposal.
But the KanCare extension approval, granted in late 2018 by CMS, noted that the state had asked CMS to defer consideration of the work requirement. The Colyer administration clarified that the state legislature had determined that a work requirement would need to go through the budget process, and would thus not be implemented as part of the KanCare extension that took effect in 2019.
Hospital closure puts a spotlight on Medicaid expansion
In October 2015, Mercy Hospital in Independence, Kansas announced that it would close, becoming the first Kansas hospital to shut down in nine years. The hospital’s closure was linked to the state’s rejection of Medicaid expansion. In states that don’t expand Medicaid, the uninsured rate remains higher and hospitals continue to struggle with higher levels of uncompensated (charity) care – particularly since federal funds to offset uncompensated care costs are being phased out now that states have the option to expand Medicaid.
Mercy Hospital’s announcement triggered renewed calls for Medicaid expansion in Kansas, but the Brownback Administration and the Colyer Administration remained steadfast in their refusal to expand Medicaid to all adults with household income up to 138% of the poverty level. In response to editorials calling for Medicaid expansion in the state, an email from Brownback’s deputy communications director Melika Willoughby described Medicaid expansion as “morally reprehensible” and an “Obamacare ruse [that] funnels money to big city hospitals.” The email also said that Medicaid expansion would create a new entitlement “for able-bodied adults without dependents, prioritizing those who choose not to work before intellectually, developmentally, and physically disabled, the frail and elderly, and those struggling with mental health issues.” (This is disingenuous, as 60% of adults in the coverage gap are in an employed household; the problem is that their jobs are low-paying and don’t provide health insurance.)
But then-State Senator Jeff King, a Republican, who was vice president of the Kansas Senate until 2017 (King did not seek re-election in 2016), represented the district where Mercy Hospital is located, and was swift in his condemnation of Willoughby’s email. King supported Medicaid expansion, albeit with a waiver that would allow Kansas to use private health insurance to cover the newly-eligible population (this is an approach that Arkansas uses to implement Medicaid expansion; New Hampshire and Iowa also used it, but have since transitioned to regular Medicaid managed care. The Kansas Hospital Association also disagreed with Willoughby’s position, and has repeatedly called for Medicaid expansion in the state.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Kansas?
Explore more resources for options in Kansas including ACA coverage, short-term health insurance, dental insurance and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”Medicaid, Children’s Health Insurance Program, & Basic Health Program Eligibility Levels” Centers for Medicare & Medicaid Services. December 2023. ⤶
- ”Governor Kelly Announces Approved Expansion of Medicaid Coverage to Kansas Mothers Postpartum” KFRM. Accessed Feb. 11, 2025 ⤶
- ”Kansas SB257” and “Kansas HB2375” BillTrack50. Introduced Feb. 10. 2025 ⤶
- Kansas governor unveils revenue neutral Medicaid expansion plan with work requirement. Kansas Reflector. December 14, 2023. ⤶ ⤶
- ”Kansas SB355” and “Kansas HB2556” BillTrack50. Introduced January 2024 ⤶ ⤶
- ”How Many Uninsured Are in the Coverage Gap and How Many Could be Eligible if All States Adopted the Medicaid Expansion?” KFF. Feb. 26, 2024. ⤶
- ”Kansas SB257” BillTrack50. Introduced Feb. 10. 2025 ⤶
- ”Kansas HB2675” BillTrack50. Accessed Feb. 11, 2025 ⤶
- ”Kansas HB2415” and Kansas SB225” BillTrack50. Accessed Feb. 11, 2025).
Although Kansas has not implemented the ACA’s Medicaid expansion, the state did implement the American Rescue Plan provision that allows states to extend postpartum Medicaid coverage to 12 months (postpartum Medicaid coverage previously ended 60 days after the baby was born). In Kansas, the postpartum Medicaid coverage extension took effect in April 2022.[efn_note]”Governor Kelly Announces Approved Expansion of Medicaid Coverage to Kansas Mothers Postpartum” KFRM. Accessed Feb. 11, 2025 ⤶
- ”October 2024 Medicaid & CHIP Enrollment Data Highlights“, Medicaid.gov, Accessed August 2024 ⤶
- “3.7 Million People Would Gain Health Coverage in 2023 If the Remaining 12 States Were to Expand Medicaid Eligibility” , urban.org, Accessed July 2022 ⤶
- Medicaid Enrollment and Unwinding Tracker. KFF. Accessed Feb. 11, 2025 ⤶
- Kansas governor unveils revenue-neutral Medicaid expansion plan with work requirement. Kansas Reflector. December 2023. ⤶
- Medicaid Enrollment and Unwinding Tracker (Archived Kansas data). KFF. Accessed Feb. 11, 2025 ⤶
- ”HealthCare.gov Marketplace Medicaid Unwinding Report” Centers for Medicare & Medicaid Services. Data through November 2023. ⤶
- ”October 2024 Medicaid & CHIP Enrollment Data Highlights. Medicaid.gov, Accessed Feb. 11, 2025 ⤶
- ”KanCare One Year Extension” KanCare. Accessed Jan. 21, 2025 ⤶

