
Medicaid eligibility and enrollment in Rhode Island
Some people who lost Medicaid after the pandemic were automatically enrolled in HealthSource RI (exchange) plans

Who is eligible for Medicaid in Rhode Island?
In addition to the aged, blind, and disabled, the following residents are eligible for Medicaid coverage in New Hampshire:1
- Non-disabled adults under 65 with incomes up to 138% of poverty level (this is Medicaid expansion under the ACA)
- Pregnant women with household incomes up to 253% of poverty level (doula services are covered, effective mid-2021. And as part of the state’s fiscal year 2023 budget, Medicaid coverage for the mother continues for 12 months after the baby is born)
- Children with household incomes up to 261% of poverty level.
- Women with household incomes up to 250% of poverty level who lose coverage under RIte Care (Medicaid managed care) 60 days postpartum are eligible for two years of Extended Family Planning coverage that provides gynecological check-ups and contraceptives.
for 2026 coverage
0.0%
of Federal Poverty Level
Apply for Medicaid in Rhode Island
Online at HealthSourceRI or HealthyRhode.ri.gov, or you can use a paper application. HealthSourceRI can also help you find local in-person assistance.
Eligibility: The aged, blind, and disabled. Also, adults with income up to 138% of poverty, pregnant women with income up to 253% of poverty, and children with incomes up to 261% of poverty.



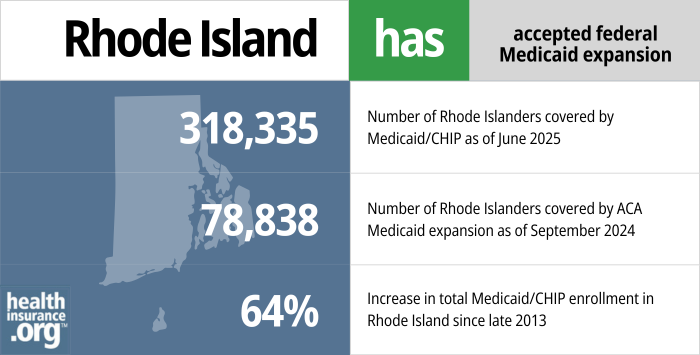
ACA’s Medicaid eligibility expansion in Rhode Island
Rhode Island embraced the provision to expand Medicaid in 2014 under the Affordable Care Act (ACA). Federal funding covered the full cost of expansion through 2016, after which the state began to pay part of the cost. The federal/state split is now 90/10, so states that have expanded Medicaid receive $9 in federal money for every $1 they spend to provide care for the Medicaid expansion population.
Rhode Island’s Medicaid/CHIP population grew by almost 114,000 people (a 60% increase) from the fall of 2013 through the fall of 2025.2 Nationwide, the average enrollment growth stood at 35% as of 2025. The increase in Medicaid enrollment stems mostly from Medicaid expansion under the ACA, as the enrollment spike due to the three-year COVID-related ban on Medicaid disenrollments had been mostly erased by 2025.
In 2023, when the uninsured rate across U.S. states ranged from 3% to nearly 19%, Rhode Island’s uninsured rate was on the lower end, at 5.4%.3
- 303,351 – Number of Rhode Islanders covered by Medicaid/CHIP as of September 20254
- 76,553 – Number of Rhode Islanders covered by ACA Medicaid expansion as of March 20255
- 60% – Increase in total Medicaid/CHIP enrollment in Rhode Island since late 20132
Explore our other comprehensive guides to coverage in Rhode Island

The ACA Marketplace allows individuals and families to shop for and enroll in ACA-compliant health insurance plans. Subsidies may be available based on household income to help lower costs.
Learn about the health insurance Marketplace in Rhode Island.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Rhode Island.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Rhode Island as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.
Learn about short-term insurance regulations in Rhode Island.

Frequently asked questions about Rhode Island Medicaid
How do I enroll in Medicaid in Rhode Island?
The state Medicaid office has worked together with HealthSourceRI (the ACA-created state-run exchange) to streamline the application process for Medicaid. You can apply online via these websites:
- HealthSourceRI (use this option if you’re under 65 and don’t have Medicare)
- HealthyRhode.ri.gov
Alternately, you can print a paper application and mail the completed form to HealthSourceRI, HZD Mailroom, 74 West Road, Suite 900, Cranston, RI, 02920-8413.
You can also call 855-609-3304 for phone assistance, or visit 70 Royal Little Drive in Providence for in-person assistance. HealthSourceRI can help you find local in-person assistance as well.
How does Medicaid provide financial assistance to Medicare beneficiaries in Rhode Island?
Many Medicare beneficiaries receive Medicaid’s help with paying for Medicare premiums, affording prescription drug costs, and covering expenses not reimbursed by Medicare – such as long-term care.
Our guide to financial assistance for Medicare enrollees in Rhode Island includes overviews of these benefits, including Medicare Savings Programs, long-term care coverage, and eligibility guidelines for assistance.
How did Rhode Island handle Medicaid renewals after the pandemic?
During the pandemic, federal rules prevented states from disenrolling anyone from Medicaid, even if they were no longer eligible or didn’t respond to an updated eligibility determination information request. But that rule ends March 31, 2023, and states were allowed to start disenrolling people from Medicaid as soon as April 1, 2023. This process, which lasted about a year, was known as “unwinding,” as it referred to an unwinding of the pandemic-era continuous coverage rule.
Rhode Island created a new protocol to automatically enroll people in a plan through HealthSource RI if they lost Medicaid and their household income was no more than 200% of the poverty level. And for people up to 250% of the poverty level who transitioned to a plan through HealthSource RI (including those with income above 200% of FPL who manually selected a plan), the state paid their after-subsidy premiums for the first two months.6
By 2025, the program was only paying the after-subsidy premium for one month, and that ends at the end of 2025.7 But the auto-enrollment and premium assistance played an important rule in helping people maintain coverage in Rhode Island after the pandemic.
During the unwinding period, 5,923 people in Rhode Island transitioned from Medicaid to a Marketplace plan. Nearly 2,500 of those people were automatically enrolled in a Marketplace plan (most states do not have a process for automatically enrolling a person in Marketplace coverage when they’re disenrolled from Medicaid).8
Rhode Island Medicaid history and details
Rhode Island Medicaid covers transgender healthcare
As of November 2015, Rhode Island joined eight other states and the District of Columbia in adding transgender healthcare to the covered services under the state’s Medicaid program.9 Rhode Island Medicaid now covers gender reassignment surgery and hormone therapy for transgender individuals.
Several other states have since added similar provisions to their Medicaid programs, ensuring access to transgender healthcare.10
Hepatitis C drug coverage expanded
Sovaldi and Harvoni have been heralded as miracle drugs for their ability to cure a significant percentage of Hepatitis C cases. But they’re breathtakingly expensive.11 As a result, many state Medicaid programs — including Rhode Island’s — required patients to meet a pre-determined set of criteria before the Hep C drugs could be prescribed. There were concerns, however, that states were too restrictive in setting their requirements, and the benefits of paying for Hep C treatment sooner and for more patients may outweigh the additional cost of the medication.
In 2015, Rhode Island was denying the majority of claims for Hepatitis C drugs. But in the spring of 2016, Medicaid director Anna Rader Wallack said that the issue was being revisited to determine whether Medicaid should take a larger role in covering the drugs that can cure Hepatitis C. And in early 2018, the state announced a new policy with regards to Hepatitis C treatment: Patients with Hepatitis C no longer need to have severe liver damage or cirrhosis to qualify for Hepatitis C drug coverage. That was welcome news for patient advocates, but the increased Medicaid spending for Hepatitis C temporarily pushed Medicaid costs over budget.
This website has details on how each state’s Medicaid program handles coverage for the drugs that treat Hepatitis C. Rhode Island is one of the states that gets an A+ grade.
Rhode Island Medicaid enrollment numbers
As of September 2025, total Rhode Island Medicaid and CHIP enrollment was 303,351,12 which was 60% higher than enrollment had been in 2013.13
Although the federal government is paying nearly all of the cost of covering the newly-eligible population, the state pays nearly half of the cost of covering the traditional Medicaid population (pregnant women, elderly people, etc. who aren’t part of the Medicaid expansion population).14
Learn more about how Medicaid funding works.
Enrollment for Medicaid and CHIP are year-round, but tend to spike during the general open enrollment due to outreach from the exchanges.
Rhode Island Medicaid history
The first states to implement Medicaid did so in January 1966, and Rhode Island wasn’t far behind them. Medicaid became available in the state in July 1966. Rhode Island uses a Medicaid managed care model to provide coverage. RIte Care and Rhody Health Partners (UnitedHealthcare) are the managed care programs in the state. RIte Care is for pregnant women and children, and utilizes UnitedHealthcare Community Plan of New England, Tufts, or Neighborhood Health Plan of RI to provide coverage.
RIte Share is a premium assistance program that pays all or a portion of an eligible employee’s share of employer-sponsored health insurance premiums.
Rhode Island Medicaid expansion history
Rhode Island was among the states that immediately moved forward with Medicaid expansion as called for in the ACA. Former Governor Lincoln Chafee made it clear immediately after the Supreme Court ruling (which made Medicaid expansion optional for states) that Rhode Island would be implementing Medicaid expansion and fully embracing the ACA (the state also set up its own state-run exchange).
Governor Chafee signed the fiscal year 2014 budget in July 2013, and it included a provision to expand Medicaid starting January 1, 2014. Eligible residents were able to begin enrolling on October 1, 2013, when the state’s health insurance exchange opened for business.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Rhode island?
Explore more resources for options in RI including ACA coverage, short-term health insurance, dental and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- ”Medicaid, Children’s Health Insurance Program, & Basic Health Program Eligibility Levels” Medicaid.gov. Accessed Dec. 30, 2025 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed Dec. 30, 2025 ⤶ ⤶
- ”Uninsured Rates, by State” Public Health Watch. June 7, 2025 ⤶
- “September 2025 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed Dec. 30, 2025 ⤶
- “Medicaid Enrollment – New Adult Group”, Medicaid.gov, Accessed Dec. 30, 2025 ⤶
- ”Rhode Island Looks to Auto-Enrollment to Ease Transitions from Medicaid to Marketplace” National Academy for State Health Policy. Nov. 14, 2022 ⤶
- ”Transitioning from Medicaid to a Qualified Health Plan” Health Source RI. Accessed Dec. 30, 2025 ⤶
- ”State-based Marketplace (SBM) Medicaid Unwinding Report” Centers for Medicare & Medicaid Services. Data through September 2024; Accessed Dec. 30, 2025 ⤶
- ”Health Care | Transgender, Health Care | Rhode Island” Glad Law. Accessed Dec. 30, 2025 ⤶
- ”Healthcare Laws and Policies: Medicaid Coverage for Transgender-Related Health Care” Movement Advancement Project. Accessed Dec. 30, 2025 ⤶
- ”This drug costs $84,000” Vox. Dec. 2, 2014 ⤶
- ”September 2025 Medicaid & CHIP Enrollment Data Highlights” Medicaid.gov. Accessed Dec. 30, 2025 ⤶
- ”Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment” KFF.org. Accessed Dec. 30, 2025 ⤶
- ”Federal Medical Assistance Percentage (FMAP) for Medicaid and Multiplier” KFF.org. Accessed Dec. 30, 2025 ⤶

