Medicaid eligibility and enrollment in Utah

Utah’s Medicaid expansion took effect in January 2020

Who is eligible for Medicaid in Utah?
Medicaid coverage in Utah is available under the following eligibility rules (these numbers include a built-in 5% income disergard that’s added to the regular eligibility limits):1
- Pregnant women with household income up to 144% of poverty are eligible for Medicaid. The mother receives full Medicaid coverage throughout the pregnancy and for 60 days postpartum (this is expected to be extended to 12 months in the near future; details below).
- Children with household incomes up to 144% of poverty are eligible for Medicaid in Utah (CHIP is available to Utah children with household incomes up to 205% of poverty).
- Women with household incomes up to 250% of poverty are eligible for certain cancer screenings through the Utah Cancer Control Program (UCCP). If they are found to have breast or cervical cancer during the screening, they are eligible for full Medicaid coverage. If they have a precancerous condition (breast or cervical), they are eligible for three months of Medicaid coverage.
- Adults under age 65 (with or without dependent children) in Utah can get Medicaid coverage if their household income is up to 138% of the poverty level. This is due to Medicaid expansion under the ACA, which took effect in Utah in January 2020 under the terms of a voter-approved ballot measure.
- Utah provides Medicaid for various other select populations – check their list to see if you might be in any of the eligible groups (note that these other populations are subject to both income and asset limits to qualify for Medicaid).
A note about postpartum Medicaid coverage: The majority of the states have extended postpartum Medicaid so that it continues for 12 months.2 Utah enacted legislation in 2023 that would extend postpartum Medicaid coverage to 12 months, although with some limitations depending on the circumstances under which the pregnancy ends. The state submitted a proposal to CMS in 2023,3 but CMS does not intend to approve that proposal.4 The legislation notes that if CMS approval isn’t granted by January 2024, the state will submit an amendment to extend postpartum coverage without restrictions, and CMS has encouraged Utah to do that.
Apply for Medicaid in Utah
You can enroll online through HealthCare.gov or the state’s Medicaid website; by phone at 800-318-2596; or by mail, fax, or in person at a local office.
Eligibility: Coverage is available for low-income aged, blind, and disabled residents. It's also available for pregnant women with incomes up to 139% of poverty, children with incomes up to 200% of poverty, and adults with incomes up to 100% of poverty. Utah’s guidelines also provide for other groups to obtain coverage depending on circumstances.
ACA’s Medicaid eligibility expansion in Utah
Medicaid was partially expanded in Utah as of April 2019. But under the terms of a new waiver that CMS approved in December 2019, the state fully expanded Medicaid as of January 2020 — albeit with a work requirement, as described below. But the work requirement was suspended as of April 2020, due to the COVID-19 pandemic, and approval for it was revoked by the Biden administration in 2021. So Medicaid is fully expanded in Utah, without a work requirement.
Medicaid coverage is available to adults under the age of 65 with household income up to 138% of the federal poverty level (FPL). For a single adult, that’s $20,120 in annual income as of 2023 (the income limit changes each spring, once the state begins to use the latest FPL numbers that are published each year in January). Note that Medicaid eligibility can be determined based on either annual income or current monthly income. This differs from premium subsidy eligibility for private plans, which is always based on total annual income.
As of October 2023, there were more than 128,000 low-income adults covered under Utah’s Medicaid expansion program. (In Utah’s Medicaid enrollment report, these are broken into four categories, depending on whether they are parents and how old they are.)9
The previous partial Medicaid expansion in Utah granted eligibility to adults aged 19-64 with income as high as the poverty level (that was $12,490 for a single person in 2019). But Utah was not receiving the enhanced federal Medicaid expansion funding, which under the ACA requires expanding eligibility to 138% of FPL. Now that the full expansion has taken effect, Utah is receiving full Medicaid expansion funding (ie, the federal government pays 90% of the cost) for the entire Utah Medicaid expansion population, including the group that had already gained coverage under the partial expansion.
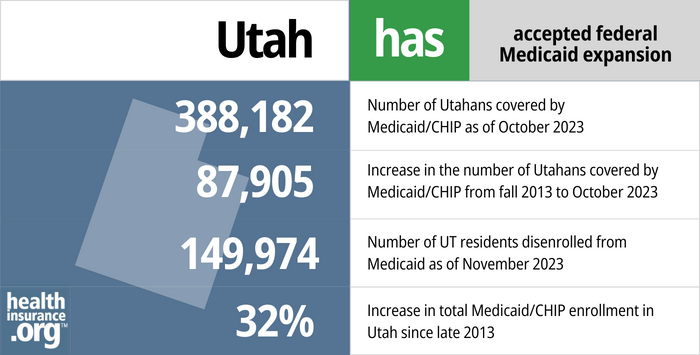
- 388,182 – Number of Utahans covered by Medicaid/CHIP as of October 20231
- 87,905 – Increase in the number of Utahans covered by Medicaid/CHIP from late 2013 to October 20232
- 149,974 – Number of UT residents disenrolled from Medicaid as of November 20233
- 32% – Increase in total Medicaid/CHIP enrollment in Utah since late 20132
Explore our other comprehensive guides to coverage in Utah

We’ve created this guide to help you understand the Utah health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.




In Utah, 444,583 people have Medicare as of 2023.4 Our guide details Medicare enrollment in Utah. It also explains how the state handles Medigap plans for enrollees under 65.


Utah residents can buy short-term health insurance plans that span up to 36 months. This includes renewals and extensions.

Frequently asked questions about Utah Medicaid
How do I enroll in Medicaid in Utah?
- You can enroll online through the Utah Medicaid office. You can also use HealthCare.gov and you’ll be routed to the Utah Medicaid office if the preliminary eligibility determination indicates that you’re eligible for Medicaid.
- You can enroll by phone (801) 526-0950 (in Salt Lake County) or toll-free at 1-866-435-7414.
- You can print a paper application (available in English and Spanish) and submit it by mail or fax (addresses and fax number here).
- You can apply in-person at your local Department of Workforce Services office (click here to see a map and find your local office).
How is Utah handling Medicaid renewals after the COVID pandemic?
During the COVID pandemic, from March 2020 through March 2023, states were prohibited from disenrolling anyone from Medicaid. But this rule ended March 31, 2023 and states are once again disenrolling people who are no longer eligible for Medicaid, or who don’t respond to a renewal notification. States have a 12-month “unwinding” period during which they must initiate eligibility redeterminations for everyone currently enrolled in Medicaid.
Medicaid disenrollments resumed in May 2023 in Utah, and CHIP premiums began to be assessed starting in mid-2023, after being suspended during the pandemic.l5 By October, 132,306 people had been disenrolled from Medicaid, mostly for procedural reasons (meaning the state didn’t have enough information to determine whether they were still eligible).3
Utah has compiled a useful list of FAQs about the unwinding process. The state chose to prioritize eligibility redeterminations for people who were most likely to no longer be eligible for Medicaid. Medicaid members in Utah can check the state’s myCase page to find out when their coverage is due for renewal. Members should ensure that their contact information is up-to-date in the state’s records, but do not otherwise need to anything until they receive a renewal packet.
When possible, the state is renewing coverage automatically, using information that the state already has on file. But if additional information is needed, a renewal packet is sent to the member. This must be completed and returned to retain coverage; even if a person is still eligible, their coverage will terminate if the state is unable to verify their eligibility (the vast majority of terminations thus far have been because the state didn’t have enough information to determine eligibility).
When a person is disenrolled from Utah Medicaid, they can enroll in other coverage, either from an employer, Medicare, or the health insurance marketplace, depending on their circumstances. If Utah Medicaid receives information indicating that the person is no longer eligible for Medicaid, their data will be transferred to HealthCare.gov and they’ll have an option to enroll in a private plan, with subsidies if eligible. There is a 16-month special enrollment period on HealthCare.gov for people who lose Medicaid, although it’s important to enroll prior to the date Medicaid ends, in order to avoid a gap in coverage.
People who are eligible to enroll in an employer’s plan have a 60-day special enrollment period to make that transition. And there’s a six-month special enrollment period when people who are eligible for Medicare can transition from Medicaid to Medicare without a late enrollment penalty.
The state has created an unwinding data dashboard where information about the number of eligibility reviews and disenrollments is available during the unwinding period.
How does Medicaid provide financial assistance to Medicare beneficiaries in Utah?
Many Medicare beneficiaries receive Medicaid’s help with paying for Medicare premiums, affording prescription drug costs, and covering expenses not covered by Medicare – such as long-term care.
Our guide to financial assistance for Medicare enrollees in Utah includes overviews of these benefits, including Medicare Savings Programs, long-term care coverage, and eligibility guidelines for assistance. Utah’s Medicaid 1115 waiver which was approved in 2019 (described above) provides dental benefits to Medicaid enrollees who are 65 or older.
Does Utah have a Medicaid work requirement?
Utah’s full expansion waiver approval allowed for a work requirement for the Utah Medicaid expansion population. The work requirement took effect in January 2020. But by April, the work requirement had been suspended as a result of the COVID-19 pandemic. As noted above, the Families First Coronavirus Response Act, enacted in March 2020, has been providing additional federal funding for Medicaid, but only on the condition that states don’t disenroll anyone from their Medicaid programs (this rule ends March 31, 2023). So work requirements were essentially a nonstarter during the COVID pandemic.
In addition, the Biden administration notified Utah (and all other states with approved or pending Medicaid work requirement waivers) that the work requirement waiver approval could be reconsidered to determine whether the program fits the objectives of Medicaid. Utah officials responded by asking CMS to uphold the prior approval for the work requirement, but the Biden administration revoked the approval in August 2021 (federal approval for work requirements was also revoked in all other states where the Trump administration had granted such waivers). But nothing changed at that point, as the state had already suspended the work requirement several months earlier.
Medicaid work requirements are controversial, as they ultimately result in people losing coverage no matter what (and most Medicaid enrollees who can work are already doing so). Work requirements in several other states had been overturned or pended due to lawsuits as of early 2020. Michigan and Utah were the only states where Medicaid work requirements were in effect as of early 2020, and both were soon suspended (Michigan’s was overturned by a judge in March) and not reimplemented. However, Georgia has since implemented a work requirement in conjunction with a partial expansion of Medicaid.
Legislation impacting Utah Medicaid
Voters approved Utah’s ballot initiative to expand Medicaid, but Republican lawmakers scaled it back
By 2018, Utah was in its fifth year of rejecting federal funding to expand Medicaid under the Affordable Care Act’s guidelines. But during the 2018 legislative session, Utah enacted H.B.472, which directed the state to submit an 1115 waiver proposal to CMS by January 1, 2019, requesting approval for Medicaid expansion in Utah, but only for people earning up to 95% of the federal poverty level (essentially 100%, after the 5% income disregard).
For perspective, the ACA calls for Medicaid expansion to adults with income up to 138% of the poverty level, so Utah lawmakers wanted to only cover part of that population. Their solution did eliminate the coverage gap in the state, but continued to use private plans in the exchange for people with income over the poverty level.
In the waiver amendment that Utah submitted in June 2018 (to partially expand Medicaid), Utah asked the federal government to pay 90% of the cost (under the ACA, this is only available if a state expands Medicaid to individuals earning up to 138% of the poverty level), and allow Utah to impose a work requirement on some Medicaid enrollees. (As discussed below, the Trump administration rejected the state’s request to receive enhanced federal Medicaid funding without a full expansion of Medicaid.)
While lawmakers in Utah were considering a scaled-back version of Medicaid expansion, consumer advocates were working to gather enough signatures to get a Medicaid expansion initiative on the 2018 ballot in Utah. They were successful, and the Utah Medicaid Expansion Initiative passed with more than 53% support in the 2018 election. The Utah Medicaid expansion ballot initiative, which called for Medicaid to be expanded to households with income up to 138% of the poverty level — with no strings attached — garnered support from numerous groups in the state, including AARP Utah and the Utah chapter of the American Academy of Pediatrics.
The text of the ballot initiative called for Medicaid expansion in Utah to take effect as of April 1, 2019, and for Utah to raise the state sales tax by 0.15% (from 4.7% to 4.85%) in order to fund the state’s portion of the cost of Medicaid expansion.
Utah’s then-Governor, Gary Herbert, said that he would not block Medicaid expansion if the ballot measure passed — which it did — despite his opposition to the ballot initiative (this was in contrast with Maine’s former Governor LePage, who blocked Maine’s voter-approved Medicaid expansion ballot initiative for more than a year; it was eventually implemented when a new governor took over in 2019).
Utah’s limited Medicaid expansion was costing the state more and covering fewer people than full expansion
But just weeks after the 2018 election, GOP lawmakers in Utah intervened to stop the implementation of the Medicaid expansion that voters had approved, opting instead for a version of Medicaid expansion that would cover fewer people and cost the state more, at least in the first few years. S.B.96 was enacted in the 2019 legislative session, reiterating H.B.472’s call for Medicaid expansion only to those with income up to the poverty level.
S.B.96 was enacted in February 2019. The state’s Medicaid expansion ballot initiative had called for expansion to take effect by April 2019, which meant there was very little time to secure federal approval for the modifications the GOP lawmakers wanted to make to Utah’s version of Medicaid expansion.
But since the state already had a pending waiver proposal at CMS with very similar terms to those called for in S.B.96, CMS was able to grant a modified approval of that earlier proposal — albeit at the state’s regular federal funding match rate of about 68%, instead of the 90% federal funding rate that applies in states that have fully expanded Medicaid. The approval came in late March, just in time for the state to implement its limited Medicaid expansion on April 1, 2019. Utah residents with income up to the poverty level were able to begin applying for expanded Medicaid at that point.
As of late May, more than 31,000 people had enrolled in the state’s expanded Medicaid program. Utah automatically transitioned about 17,500 Primary Care Network enrollees (this program is described below in more detail) to the new Medicaid expansion program, but the rest of the new enrollees had applied for coverage after the partial expansion coverage became available.
In addition to partial Medicaid expansion, Utah’s approved waiver also allowed the state to impose a Medicaid work requirement starting in 2020 (this continued to be allowed under the full expansion waiver approval that was granted in late 2019, although the work requirement was suspended due to the COVID pandemic and approval was subsequently withdrawn by the Biden administration).
The initial approved waiver also allowed the state to stop enrolling eligible residents in the expanded Medicaid program if “projected costs for the Adult Expansion Population exceed annual state appropriations.” That provision would have allowed the state to put eligible enrollees on a waitlist if and when enrollment was capped. But the enrollment cap has been eliminated under the approval for full Utah Medicaid expansion.
Despite partial expansion, Utah wanted enhanced federal funding that applies to states with full expansion. CMS said no.
The Utah Department of Health published an implementation guide for the limited Medicaid expansion and the state’s future plans. It noted that an estimated 70,000 to 90,000 people would be covered under the newly approved version of Medicaid expansion. And Utah’s limited Medicaid expansion did eliminate the coverage gap in the state.
But about 45,000 more people would have been eligible for Medicaid if the state had implemented the Medicaid expansion ballot initiative (as the state ended up doing in 2020). Instead, these individuals (with income from 101% to 138% of the poverty level) continued to be eligible for substantial premium subsidies and cost-sharing subsidies in the exchange in 2019 (their total out-of-pocket costs, including premiums and cost-sharing, would have been lower with Medicaid; the new waiver approval means they became eligible for Medicaid as in 2020).
Utah’s 2018 waiver proposal — based on H.B.472 and mostly approved by CMS in March 2019 — requested enhanced federal funding for Utah’s limited Medicaid expansion proposal (ie, the 90/10 split that otherwise applies only in states that have fully expanded Medicaid). Although CMS granted temporary approval (through January 2021) for Utah to expand Medicaid to adults earning up to the poverty level and impose a work requirement as of 2020, CMS clarified that the state would only receive its regular federal funding match, which is about 68%.
(Note that under the terms of the full expansion waiver that was subsequently submitted and approved, Utah is receiving 90% federal funding for the entire Medicaid expansion population.)
Because 32% of the cost of covering up to 90,000 people would have been a larger amount than 10% of the cost of covering up to 130,000 people, Utah’s initial approach actually would have resulted in the state spending more of its own money to cover fewer of its residents.
The specifics of Utah’s per capita cap proposal
In May 2019, Utah published a draft of their next proposed 1115 waiver (referred to as the “per capita cap” waiver proposal), opening up a public comment period that ran through June 2019.
The per capita cap waiver proposal asked the federal government to switch to the enhanced funding model while still maintaining the income cap for Medicaid expansion eligibility at 100% of the poverty level and keeping the already-approved work requirement.
But in order to make the arrangement more palatable for the federal government, Utah was proposing a per capita funding cap for the enhanced federal funding. As outlined in the draft 1115 waiver, the state planned to work with CMS to develop a per-enrollee base amount that would be adjusted annually and would vary for each of the state’s enrollment groups to account for differing costs across distinct populations.
The state would be able to use leftover funding (ie, if expenses fall below the per capita cap) to offset excess spending in a future year, but if total costs exceed the per capita cap, the state’s funding for that portion of the costs would be covered at the normal Medicaid federal matching rate (ie, for Utah, that’s about 68%)
In July 2019, before Utah had officially submitted the 1115 waiver, they received word from the Trump administration that their request for full Medicaid expansion funding was not going to be approved if they only partially expanded Medicaid. CMS explained that the state’s proposal to receive full Medicaid expansion funding while having people with income between 100% and 138% of the poverty level enroll in subsidized private plans in the exchange “would invite continued reliance on a broken and unsustainable Obamacare system.” (The Trump administration was fairly hostile toward the ACA.)
Utah did go ahead and submit the waiver proposal in late July. CMS sent Utah a letter in August 2019 detailing the fact that full Medicaid funding for partial expansion would not be permitted, but that other aspects of the waiver proposal were still being considered by the agency. The state’s efforts to cap Medicaid expansion at 100% of the poverty level are now a moot point, since full expansion took effect in January 2020. But the per-capita cap proposal is still pending at CMS.
In addition to the per-capita cap, the waiver proposed several other changes, including:
- Up to 12 months of continuous Medicaid eligibility.
- A six-month period of ineligibility if a person commits an “intentional program violation.” The waiver proposal outlines what counts as a violation, but it’s essentially fraud with the intent to receive benefits or coverage that the person would not otherwise be eligible to receive.
- Elimination of presumptive eligibility determined by a hospital.
When CMS informed Utah officials that their request for enhanced Medicaid expansion funding was not going to be approved, Gov. Herbert, Senate President Stuart Adams, and House Speaker Brad Wilson expressed their disappointment in a statement, and noted that they would continue to work on a solution for Medicaid expansion.
Utah’s “fallback plan” approved by CMS in December 2019
Although the federal government rejected Utah’s proposal to receive full federal funding for a partial Medicaid expansion, and also rejected the proposal to allow people with income above the poverty level to have a choice between Medicaid and a subsidized plan in the exchange, Utah had already outlined contingency plans earlier in 2019.
The state submitted its “fallback plan” waiver proposal to CMS in November 2019, after accepting public comments earlier in the fall. The fallback plan called for expanding Medicaid eligibility in Utah to households with income up to 138% of the poverty level (ie, what voters approved in the 2018 election), but with a work requirement as well as a lock-out period for “intentional program violations,” premiums for enrollees with income above the poverty level, a ban on presumptive eligibility determinations under Medicaid expansion guidelines, and various other provisions.
CMS granted approval in December 2019, and the new Medicaid eligibility guidelines took effect in January 2020. The work requirement provision of the waiver proposal was approved and did take effect in 2020, but it was suspended by April due to the COVID pandemic and approval for it was later withdrawn by the Biden administration.
Utah had a contingency plan in case their work requirement was rejected. In that case, Utah’s final plan, if no waiver approval had been granted by July 1, 2020, was to simply implement Medicaid expansion as called for in the ACA (and in the state’s ballot initiative), without a waiver.
The state had created an at-a-glance chart that compared the details of the bridge plan, the per capita cap plan, the fallback plan and the regular expansion plan. The Utah Department of Health has also published a chart showing enrollment over time in both the partial expansion and the full expansion program.
Very limited expansion was approved in 2017; enrollees were transitioned to expanded Medicaid in 2019
In March 2016, Utah Governor Gary Herbert signed HB437 into law, providing for a limited version of Medicaid expansion. Utah’s version was much less comprehensive than the Medicaid expansion called for in the Affordable Care Act (ACA). Utah House Majority Leader Jim Dunnigan noted that the legislation “targets those in extreme poverty.”
Instead of expanding coverage to roughly 130,000 people (as would have been the case if the state had accepted federal funding for the ACA’s version of Medicaid expansion), HB437 was expected to provide Medicaid coverage to about 9,000 – 11,000 of Utah’s poorest residents (by 2019, however, nearly 17,500 people were enrolled). The limited expansion provided Medicaid for 12 months to Utahns who are homeless, mentally ill, in need of treatment for substance abuse, or recently released from incarceration.
Utah’s limited expansion of Medicaid was slated to cost the state about $30 million a year ($13.6 million of that from hospitals in the state), and the federal government about $70 million a year. Democratic lawmakers — who felt that HB437 was “less than crumbs” — noted that full expansion of Medicaid would have cost the state $44 million a year (some estimates say $50 million), but would have brought in $420 million a year in federal funds, garnering far more value from those state dollars.
Utah submitted a Section 1115 waiver proposal (the Primary Care Network demonstration) to CMS in July 2016, but CMS quickly responded, asking for additional information and an additional public comment period. The state had planned to implement the limited Medicaid expansion proposal in January 2017, but CMS approval didn’t come until October 31, 2017.
Under the terms of the approved waiver, the state was able to begin enrolling people as of November 2017. Utah residents could qualify for up to 12 months of coverage under the Medicaid waiver if they had income of no more than 5% of the federal poverty level (that amounted to no more than $603 in 2018), and were either chronically homeless or involved in the criminal justice program, and/or in need of substance abuse treatment.
In 2019, Utah transitioned Primary Care Network enrollees to the Medicaid expansion program.
What was Utah Access Plus?
Utah Access Plus was a compromise proposal reached by Utah’s “gang of six” in 2015, after lawmakers rejected Governor Herbert’s Healthy Utah Medicaid expansion proposal during the 2015 legislative session. If it had won legislative support, Utah Access Plus would have used Medicaid funds to purchase private coverage for eligible residents. Because it was an alternative method of expanding Medicaid, it would have also needed HHS approval in order to obtain federal funding.
The “gang of six” included then-Governor Gary Herbert, Lt. Governor Spencer Cox, Senate President Wayne Niederhauser, House Speaker Greg Hughes, House Majority Leader Jim Dunnigan and Senator Brian Shiozawa. They worked together during the summer of 2015 to flesh out the details of a plan to replace two previous proposals (Gov. Herbert’s Healthy Utah plan and the House of Representatives’ Utah Cares plan). The gang of six announced in July 2015 that they had come to an agreement on a path to Medicaid expansion, but GOP lawmakers rejected their proposal, putting the state back to square one.
Prior rejection
Governor Herbert worked for years to expand Medicaid. The House’s failure to support Utah Access Plus was the second time he had offered a proposal to lawmakers only to see it rejected. In October 2014, Herbert announced that he had come to a tentative agreement with HHS on his Healthy Utah plan that would have offered a modified, somewhat unique approach to expansion.
Governor Herbert unveiled the details of the HHS-approved Healthy Utah program at a meeting with legislators in December 2014. The proposal would have covered 126,000 Utah residents, but the legislation to implement it, SB 164, failed in committee in March 2015.
Lawmakers in the House Business and Labor Committee instead voted to recommend the Utah Cares proposal (HB 446) for further consideration. Utah Cares would have cost the state more, garnered less in federal funding, and covered fewer people with much more limited benefits. It had also not received tentative approval from HHS the way Herbert’s Healthy Utah plan had. Ultimately, neither bill advanced in the legislature during the 2015 session.
Enrollment dropped from 2016 to 2019, but increased again under expansion and the COVID pandemic
From 2013 to July 2016, total enrollment in Utah’s Medicaid/CHIP program increased by 4% (12,828 people), but by March 2019, enrollment was about 3% lower than it had been in 2013. This was despite an increased eligibility limit for low-income parents, and the limited expansion of Medicaid for homeless people with no income, which took effect in November 2017.
However, enrollment in Utah’s Medicaid program grew rapidly once coverage was expanded to adults with income under the poverty level. As of mid-2023, it was 41% higher than it had been in 2013, even though tens of thousands of people had been disenrolled from the program at that point in the post-pandemic “unwinding” process.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- “October 2023 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed December 2023 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed December 2023 ⤶ ⤶
- Medicaid Enrollment and Unwinding Tracker. KFF. Accessed December 2023 ⤶ ⤶
- “Medicare Monthly Enrollment” CMS.gov, April 2023 ⤶
- Unwinding Medicaid Eligibility. Utah Department of Health and Human Services. September 2023. ⤶







