Medicaid eligibility and enrollment in Wyoming

Medicaid expansion legislation died, yet again, in the 2023 session. But a bill to extend postpartum Medicaid to 12 months was successful.

Who is eligible for Medicaid in Wyoming?
Eligibility remains mostly as it was in 2013, as Wyoming has not yet accepted federal funding to expand Medicaid under the ACA. Non-disabled, non-pregnant adults without dependent children are not eligible, regardless of income. The following legally-present Wyoming residents are eligible for Medicaid:
-
- Parents with dependent children, if their household income is up to 56% of poverty (just under $14,000 annually for a family of three as of 2023).
- Pregnant women and children age 0 – 5 with household incomes up to 159% of poverty. (Legislation was enacted in Wyoming in 2023 to extend Medicaid coverage for the mother for 12 months postpartum, instead of having it end 60 days after the birth; the American Rescue Plan provided five years of federal funding for this, and the federal spending bill enacted in late 2022 made this funding permanent.)
- Children 6 – 18 are eligible for Medicaid with household incomes up to 138% of poverty.
- Children are eligible for separate CHIP with household incomes up to 205% of poverty.
- The Pregnant by Choice program provides no-cost family planning services to women who enroll within 60 days postpartum and have household incomes that do not exceed 159% of poverty.
Apply for Medicaid in Wyoming
You can enroll online through HealthCare.gov or the state Department of Health website.
Eligibility: Pregnant women and children are eligible with household incomes up to 154% of poverty (children are eligible for CHIP with household incomes up to 200% of poverty). Parents with dependent children are eligible with household incomes up to 56% of poverty.
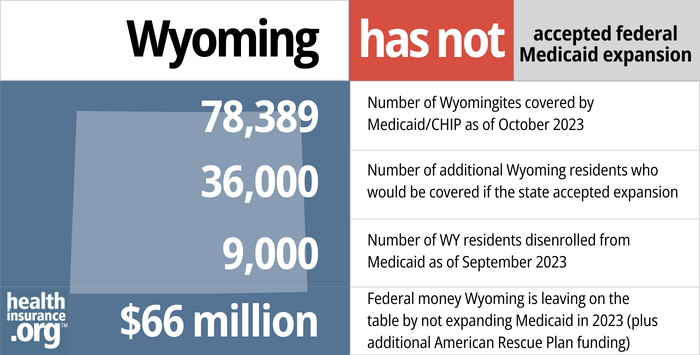
Still no Medicaid eligibility expansion in Wyoming
Wyoming is among only a dozen states where Medicaid still has not been expanded, and the state continues to refuse federal funding that would allow it to expand coverage to about 19,000 low-income residents.
An estimated 7,000 of those individuals are in the coverage gap (i.e., they essentially have no access to coverage), despite federal rules that would allow them to have coverage if Wyoming were to accept federal funding to expand Medicaid.
The majority of Wyoming residents support Medicaid expansion, and Democratic state lawmakers, along with former Governor, Matt Mead, (a Republican), have spent years pushing for Medicaid expansion. But Republican lawmakers, who hold an overwhelming majority in both legislative chambers, have thus far refused to expand Medicaid eligibility in Wyoming.
There were hopes that might change in 2020, 2021, 2022, and again in 2023, but that did not come to pass. As described below, Medicaid expansion legislation was again under consideration in Wyoming in 2023, for the ninth time in the last decade. Wyoming House Revenue Committee Chair, Rep. Steve Harshman (R, Casper), now supports Medicaid expansion, after steadfastly rejecting it in prior years, and shepherded the bill through committee early in 2023. But the measure died soon thereafter, without ever getting a reading on the full House floor.
- 78,389 – Number of Wyomingites covered by Medicaid/CHIP as of October 20231
- 36,000 – Number of additional Wyoming residents who would be covered if the state accepted expansion2
- 9,000 – Number of WY residents disenrolled from Medicaid as of September 20233
- $66 million – Federal money Wyoming is leaving on the table by not expanding Medicaid in 2023 (plus additional American Rescue Plan funding)4
Explore our other comprehensive guides to coverage in Wyoming

We’ve created this guide to help you understand the Wyoming health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.


In 2023, three insurers offer stand-alone individual/family dental coverage through Wyoming’s Marketplace.5


87% of Wyoming Medicare beneficiaries have Original Medicare, as much of the state didn’t have Medicare Advantage plans available prior to 2019.


In Wyoming, short-term health insurance plans are available and adhere to federal regulations. There are at least seven insurers selling short-term health insurance plans in Wyoming in 2023.6

Frequently asked questions about Wyoming Medicaid
How do I enroll in Wyoming Medicaid?
Residents have several avenues to apply for Medicaid in Wyoming:
- You can enroll online through HealthCare.gov — or call 1-800-318-2596 for phone assistance at HealthCare.gov. (Use this option only if you’re under 65 and don’t have Medicare.)
- You can enroll online through the State Department of Health application website.
- You can print an application in English or Spanish and mail it to the Wyoming Department of Health (address here).
Once you have coverage, you can use the Wyoming Medicaid client portal, or contact their customer service department at 1-800-251-1269.
How does Medicaid provide assistance to Medicare beneficiaries in Wyoming?
Many people with Medicare receive help through Medicaid with Medicare premium costs, prescription drug expenses, and expenses that Medicare doesn’t cover — such as long-term care.
Our guide to financial resources for Medicare enrollees in Wyoming provides an overview of those programs, including Medicare Savings Programs, nursing home coverage, and income guidelines for assistance.
How is Wyoming handling Medicaid renewals after the pandemic?
Under federal rules designed to address the pandemic, states received additional federal Medicaid funding but were also not allowed to disenroll anyone from Medicaid between March 2020 and March 2023. But disenrollments could resume as early as April 1, and states are required to redetermine the eligibility of everyone enrolled in Medicaid during a year-long “unwinding” of the pandemic-era continuous coverage rule.
Wyoming Medicaid’s website has a notice advising people to ensure that their contact information is up-to-date so that they will receive renewal notifications, and the state has a basic FAQ page notifying Medicaid enrollees that renewals are being conducted between March 2023 and March 2024. By the end of July 2023, the Wyoming Department of Health reported that 10,700 people had been disenrolled from Medicaid in the period from April through July. But only about 600 of those people had officially been deemed ineligible. The vast majority — 10,100 — had been disenrolled for procedural reasons, which means the state didn’t have enough information to determine their eligibility (in general, this means the person didn’t complete their renewal forms).
As of April 2023, more than 84,000 people were enrolled in Medicaid/CHIP programs in Wyoming, and all of them will need to have their eligibility rechecked during the unwinding period. Wyoming’s April 2023 enrollment was 25% higher than enrollment had been in 2013. As of 2019, Medicaid enrollment in Wyoming had been 20% lower than the 2013 level. And as of September 2020, Wyoming was the only state where Medicaid enrollment was still below what it had been in 2013. But that was no longer the case by mid-2021.
For people who lose Medicaid and need to purchase their own replacement coverage (ie, they aren’t eligible for Medicare or an employer’s plan), HealthCare.gov is offering an extended enrollment opportunity, from March 31, 2023 through July 31, 2024, available to anyone who loses Medicaid at any time during that window.
Legislation impacting Wyoming Medicaid
Medicaid expansion legislation dies once again in Wyoming’s legislature in 2023
For years, Wyoming lawmakers have rejected Medicaid expansion. There were hopes that the legislature would pass a Medicaid expansion bill in each of the last several sessions, but that has not happened.
The latest Medicaid expansion bill (H.B.80), introduced in early 2023, passed out of the House Revenue Committee by a 6-3 vote. And Rep. Steve Harshman (R, Casper), who chairs the Revenue Committee, noted that he now supports Medicaid expansion after opposing it in the past. Before approving the bill, committee members added amendments banning coverage of gender-affirming care and abortion. And as had been the case in prior years, the legislation included a caveat that expansion would only continue as long as the federal government continues to pay at least 90% of the cost (this is a common provision that other states have incorporated into their Medicaid expansion legislation).
But the legislation ultimately died just a few weeks later, without ever getting a hearing on the House floor. So for the time being, Wyoming will continue to reject federal Medicaid expansion funding, and will continue to have a coverage gap for its poorest residents.
If Wyoming were to expand Medicaid, the Department of Health projects that the cost to the state will be $22 million every two years. But they note that the American Rescue Plan’s two years of additional federal funding for states that newly expand Medicaid would provide the state with $54 million (in addition to the normal federal funding for Medicaid expansion, which pays 90% of the cost). That would be enough to more than cover the state’s costs for the first four years.
(The American Rescue Plan provides additional federal funding for the first two years to any state that expands Medicaid after March 2021. Thus far, only Oklahoma, Missouri, and South Dakota have utilized that funding. North Carolina is expected to join them by early 2024. In the first three states, Medicaid expansion came about due to voter-approved ballot measures, rather than legislation.)
Joint Revenue Interim Committee pushed for Medicaid expansion in the 2022 session
H.B.20 was introduced in January 2022, and was sponsored by the Joint Revenue Interim Committee. This was the eighth time that legislation to expand Medicaid was considered in Wyoming’s legislature, and the Joint Revenue Committee had been supportive of Medicaid expansion in recent years. But as was the case in all of the previous sessions, Medicaid expansion did not garner enough support from lawmakers to pass.
Senate committee approved Medicaid expansion in 2021, but it did not advance after that
Senate File 154, was introduced in Wyoming’s Senate in March 2021. On March 8, the Senate Labor, Health, & Social Services Committee voted 3-2 to advance the bill (you can watch the committee discussion here). But the legislation did not advance after that.
Legislative committee advanced Medicaid expansion legislation in advance of 2020 session, but legislature killed it
In November 2019, lawmakers on Wyoming’s Joint Interim Revenue Committee voted in favor of a Medicaid expansion bill that was to be sent to the full legislature once it convened in February 2020. The vote was 8-5 in support of the measure, raising hopes that it might garner enough support in the full legislature to pass in 2020 (since the state’s budget would have been involved, the bill needed two-thirds support in its originating chamber in order to advance).
A group of medical students from the University of Wyoming testified in front of the committee in favor of Medicaid expansion, noting that when patients are unable to afford their care it affects their doctors as well, leading to high rates of burnout and potentially driving doctors out of the state. The Wyoming Hospital Association also testified, explaining how the state’s uncompensated care costs would be mitigated by Medicaid expansion.
Some GOP committee members who had previously opposed Wyoming Medicaid expansion voted in favor of the measure in late 2019, but some remained steadfast in their opposition, including one who noted that he believes the federal government’s 90% funding rate for Medicaid expansion will not last (there is no evidence to support this, as federal Medicaid expansion funding has never dropped below 90% in any state).
Ultimately, the bill died in committee on the first day of the 2020 legislative session. However, as the Covid-19 pandemic struck, Wyoming lawmakers voted to have the Joint Revenue Committee again consider Medicaid expansion, with the possibility that it could be part of a special session in June. That did not come to pass, however, and the committee recommended that Medicaid expansion be reconsidered again during the regular 2021 legislative session (S.F.154, described above, was the 2021 version of Medicaid expansion legislation in the state; it did not advance during the 2021 session).
So although the issue of Medicaid expansion became more urgent than ever as a result of the widespread job and coverage losses caused by the pandemic, Wyoming opted to postpone the Medicaid expansion debate. This left rural hospitals without enough funding and thousands of low-income residents without any realistic access to health coverage. As of early 2023, nearly three years into the pandemic, that’s still the situation in Wyoming.
Lawmakers considered Medicaid expansion with a work requirement in 2019, but it didn’t pass
In 2019, lawmakers in Wyoming considered SF 146, which called for a study of the effects of Medicaid expansion if Wyoming were to expand coverage as of 2021. The measure passed with strong support in the Senate, but narrowly failed in the House.
Lawmakers also considered HB 244, which would have directed the state to work with HHS to expand Medicaid, albeit with a work requirement. But that bill failed in February in the House, by a vote of 23 to 36.
Wyoming Senate passed a bill in 2018 to impose work requirements, but it died in the House
Instead of working towards Medicaid expansion in 2018, Senate Republicans passed S.F.97 in February 2018, by a vote of 25 to 5, in an effort to impose work requirements on the state’s existing Medicaid population. The measure moved to the House, where an identical bill (H.B.148) failed on introduction in the House in mid-February, by a vote of 34-24 (it needed a two-thirds majority to advance). Ultimately, S.F.97 failed in the House, where the Labor, Health, & Social Services Committee killed it with a 4-4 tie vote, not allowing it to advance.
If S.F.97 had been enacted, the state would have submitted a waiver proposal to the federal government, seeking permission to impose a work requirement for the existing Medicaid program. There would have been a variety of exemptions, but for people not exempt, there would have been a requirement to either work, volunteer, attend school, or participate in a job training program for at least 20 hours per week. If they failed to do so, they would have lost eligibility for Medicaid for 12 months. Amendments to soften the requirement by making the ineligibility period shorter than 12 months did not pass in the Senate.
Since Medicaid has not been expanded in Wyoming, the state only provides Medicaid to low-income elderly residents who need long-term care, low-income disabled residents (those two populations account for about 60% of the state’s Medicaid spending), low-income children and pregnant women, and very low-income parents who are caring for a dependent child. In Wyoming, those parents are only eligible if their household income doesn’t exceed 56% of the federal poverty level (51% plus a built-in 5% income disregard). For a family of three, that’s about $1,160 in monthly income in 2023.
In general, the Medicaid work requirement would only have applied to that last category, of very low-income parents. Low-income parents whose child is over the age of six would have been subject to the work requirement. The state estimated that about 2,500 to 3,500 people would have been subject to the work requirement—the Wyoming Department of Health confirmed that the rest of the state’s Medicaid population (roughly 57,000 more people) would either have been exempt from the work requirement or are already working.
But those 2,500 to 3,500 very low-income parents would have had to start working (or volunteering or participating in a job-training program) at least 20 hours per week in order to keep their Medicaid coverage if S.F.97 had been enacted and the federal government had approved a waiver proposal. But that did not come to pass, as the legislation did not advance in the Wyoming House.
Prior efforts to expand Medicaid, but no progress
Although Wyoming’s lawmakers have been reluctant to expand Medicaid thus far, a downturn in oil and gas revenues and the resulting shortfall in Wyoming’s budget may eventually make them reconsider; former Governor Matt Mead estimated that expanding Medicaid would bring $268 million in federal dollars into Wyoming.
Governor Mead was initially opposed to Medicaid expansion when he took office in 2011, but by 2013, he had begun exploring options for expansion of coverage, and by the end of 2014, he was a proponent of expanding Wyoming’s Medicaid program using a Section 1115 waiver to implement a state-specific version of expansion.
In the fall of 2015, Governor Mead’s administration was working to obtain estimates from CMS regarding federal spending for Medicaid expansion in Wyoming, and Mead provided two versions of his 2016 budget to lawmakers. One version included Medicaid expansion, and the other didn’t, so that lawmakers could see the financial ramifications of continuing to reject Medicaid expansion. But lawmakers continued to reject Medicaid expansion.
In 2016, Governor Mead tried again, including Medicaid expansion in his budget proposal. The Joint Appropriations Committee removed it, but Medicaid expansion supporters attempted to put it back in via a budget amendment. That effort failed, however, with only 10 senators voting in favor and 20 voting against it. Opposition in the House was even stronger, so Medicaid expansion proponents in the House didn’t attempt a budget amendment of their own.
Hospitals in the state have thrown their weight behind the efforts to expand Medicaid, noting that their budgets are already tight, and that they face considerable uncompensated care losses unless the state accepts federal funding to expand Medicaid. In just three months in 2015, Wyoming hospitals had already used up more than half of a small fund set aside by the state to offset uncompensated care losses.
In 2017, Mead noted that he regretted the fact that the state hadn’t expanded Medicaid, and pointed out that Wyoming was missing out on $100 million per year in federal funding by rejecting Medicaid expansion. But Medicaid expansion still has not gained traction in the Wyoming legislature as of 2019, due to strong Republican opposition. Even when a work requirement was added to the expansion legislation (2019’s HB 244), the measure failed to pass.
Early expansion discussions
In November 2014, Governor Mead’s administration released the details of their SHARE (Strategy for Health, Access, Responsibility and Employment) proposal for modified Medicaid expansion.
The governor’s proposal included having newly-eligible enrollees pay a small premium ($20 to $50 per month for most households) if their income was between 100% and 138% of poverty level, and there would also have been small copays for most newly-eligible enrollees. Mead’s proposal also included access to vocational rehabilitation and job search services to encourage unemployed enrollees to enter the job market. Officials noted that the job training and placement portion of the program would not have been a requirement for participation (which would have been a hard sell in terms of winning federal approval under the Obama Administration, which flatly rejected work requirements and similar provisions), but rather a benefit for enrollees.
Governor Mead’s proposal had not yet been officially approved by HHS, but Mead and his administration were reasonably certain that HHS would ultimately approve their plan for Medicaid expansion, as it had been thoroughly vetted by the federal government and approved as budget neutral for the state.
But it also had to be approved by Wyoming lawmakers, which didn’t happen. Mead noted that if the legislature didn’t approve his plan, he “would ask and expect them to have an alternative for the 17,000 people” who have no realistic access to coverage in Wyoming due to the state’s failure to expand Medicaid.
In December 2014, the Joint Interim Labor, Health, and Social Services Committee approved a different Medicaid expansion bill, created by the committee’s chairman, Charles Scott, a Republican from Casper. This alternative passed the committee by a 10 – 4 vote, but it hadn’t been vetted by the feds, and nobody knew how it would perform from the perspective of the state’s budget. The committee also voted on the SHARE proposal, but it didn’t pass (7-7).
Scott’s alternative proposal — loosely modeled on Indiana’s plan — called for having the Medicaid expansion population put funds into health savings accounts (HSAs), supplemented by additional government funds (since this proposal had not been approved by the federal government, it remained unclear whether the state would have to fund the HSAs rather than relying on federal Medicaid funds). Scott had long advocated for HSAs as a measure of healthcare reform, but they’re rarely useful for people who are living in poverty.
Initially, after the committee vote, it appeared that Wyoming lawmakers would use Scott’s plan as the focus of their Medicaid expansion discussions during the 2015 legislative session. A concern was that the plan has not been approved or even reviewed by HHS, and similar proposals had been rejected by HHS. But then in late January, Indiana announced that their Medicaid expansion waiver had been approved by HHS, creating hope that perhaps Scott’s plan could also get approval.
In January 2015 the Senate Labor and Health Committee approved a Medicaid expansion bill (SF 129) that was essentially a combination of the SHARE proposal and Scott’s HSA proposal. The committee voted 4-1 to approve the bill and send it to the Senate floor. But on February 6, the Senate rejected the bill on a 19 – 11 vote.
A House committee had been scheduled to consider another Medicaid expansion proposal on the same day, but the committee abandoned their efforts after seeing the results of the SF 129 vote in the Senate. As a result, Medicaid expansion was off the table for the 2015 legislative session in Wyoming. And efforts to expand coverage in subsequent sessions have also failed, even when a work requirement provision was added to the legislation.
Wyoming Medicaid can seek recovery of birth costs from unmarried fathers
Wyoming enacted legislation in 2018 (HB 86) that allows the state to seek to recover a portion of the cost of Medicaid-funded births in certain situations. As of July 2018, when a baby is born to a mother who is on Medicaid and not married to the baby’s father, the state can work to determine paternity and then bill the father for a portion of the cost of the birth.
The amount billed depends on the father’s income. Fathers with income below 200% of the poverty level do not have to pay the state for the cost of their baby’s birth. But fathers with income above that level have to pay a percentage of the cost, ranging from 10% to 50%, depending on how high the father’s income is.
The legislation doesn’t apply to fathers who are married to the mother of the child, since Medicaid eligibility is based on household income. In other words, those fathers’ incomes are already taken into consideration when determining whether the mother is eligible for Medicaid to cover her pregnancy costs. But when the mother and father have separate tax households, the mother can qualify for Medicaid without the father’s income being taken into consideration. So the intent of the legislation is to ensure that fathers with financial means are accountable, at least to some extent, for the cost of their baby’s birth.
Legislation like this is controversial, however, and consumer advocates worry that it is a counterproductive approach in terms of the overall health of the mother and baby.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- “October 2023 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed November 2023 ⤶
- ”3.7 Million People Would Gain Health Coverage in 2023 If the Remaining 12 States Were to Expand Medicaid Eligibility“, Matthew Buettgens and Urmi Ramchandani Urban Institute, July 2022 ⤶
- ”Medicaid, Kid Care disenrollments fall amid ‘unwinding’“, WyoFile, October 2023 ⤶
- ”Last 11 States Should Expand Medicaid to Maximize Coverage and Protect Against Funding Drop as Continuous Coverage Ends“, Center on Budget and Policy Priorities, January 2023 ⤶
- Damico, Anthony, Gretchen Jacobson, and Tricia Neuman. “Medicare Advantage 2018 Data Spotlight: First Look.” Kaiser Family Foundation. Accessed October 13, 2023. ⤶
- “Supplement Insurance (Medigap) Plans in Wyoming.” Medicare.gov. Accessed October 13, 2023. ⤶







